Playlist
Show Playlist
Hide Playlist
Mineralization of the Bone Matrix
-
Slides 09 Types of Tissues Meyer.pdf
-
Reference List Histology.pdf
-
Download Lecture Overview
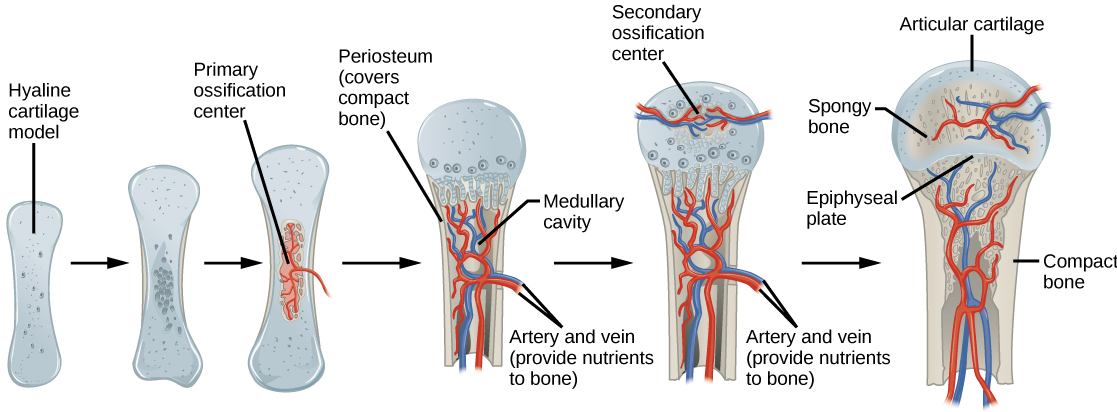
00:01 The mineralization of bone matrix is rather a complex process. I have just listed here a few of the events that happen and probably the critical event is the first one. For bone to be mineralized, for the osteoblast to release matrix vesicles that they developed inside them, there has to be concentrations of calcium and phosphate far beyond what is normal in other tissues. So initially these osteoblasts secrete osteocalcin and a few other different sorts of proteins and molecules. And that binds calcium in their immediate area and by binding extracellular calcium into that matrix area, the concentration increases. 00:59 Osteoblasts sense that and they secrete alkaline phosphatase and that increases the concentration of phosphate, which itself starts a big revolving wheel increasing calcium. 01:16 So the process goes on and on and on until finally those calcium and phosphate levels far exceed threshold and then the osteoblast then release their matrix vesicles by exocytosis and then crystals form. Crystals of hydroxyapatite crystals and the mineralization begins and these crystals then disappear and form right throughout the matrix of the bone. 01:43 Far more complicated in that but that to summarizes some of the main events. 01:50 I briefly just want to point out the structure of a synovial joint. We can return to our previous section of this growing bone. I pointed out the two articular surfaces. They are supported on all the way around the joint by a very strong ligament. You can see that ligament in this section. It is the red stained component at the bottom of the slide and also on the top of the image. It is collagen, very dense collagen. The joint cavity is that space between the two articular surfaces. It is full of synovial fluid that is secreted by the synovial organ, very special part of the joint cavity with a very special epithelial cell that secretes that synovial fluid and that synovial fluid gives nutrition to the articular cartilage as I described in a lecture in this course on cartilage and it also acts as a lubricant for the joint. It is a diarthrotic joint. There are different sorts of joints in the body that the anatomists would describe to you. This is a very simple joint that most of us are familiar with, perhaps the knee joint or the hip joint. 03:12 And finally I just want to mention that bone is a mineral reservoir. Two hormones secreted by the parathyroid and also the thyroid control calcium levels. The parathyroid hormone as is stated there stimulates osteocytes and osteoclasts to resorb bone to take up bone when there are low calcium levels in the blood. And conversely calcitonin secreted by the thyroid gland, then inhibits the action and so there is no more calcium being taken up from the bone and therefore calcium levels can be monitored and controlled to be normal. 03:55 These are very, very very important hormones and again I have discussed these hormones in another lecture in this course on the endocrine system. So, let me now summarize what I have tried to describe in this lecture. The list here is similar to the list I put up at the very start. 04:15 I want you to be able to know and understand the way in which bone forms, from that basic cartilage model or bone can form purely by mesenchymal cells differentiating to osteoprogenitor cells and then becoming osteoblasts and laying bone down in this membranous component such as we see when bones of the skull are made. There is no cartilage template. The cartilage model that is formed in certain parts of the body corresponds to regions where long bone and other bones are going to develop. It is a part of a skeleton. Part of the skeleton that is involved with movement and the bones have muscles attached to them. Those bones go through endochondral ossification, a process where the bone is formed from a cartilage model. 05:19 But cartilage undergoes waves of proliferation and then finally they hypertrophy, die, the matrix becomes calcified, bone is laid down on that matrix and resolved or retained or remodeled depending on where the bone is. It could be spongy bone or in the medullary cavity. The bone on the diaphysis is produced by periosteum and I guess it is the form of intramembranous ossification because that periosteum being a membrane just lays down the bony collar, which is going to be compact bone that forms a diaphysis of the bone. And I think it is important to remember that the primary ossification center starts before birth. It starts to lay down the diaphysis and the medullary cavity that creates the zone that is going to develop into the epiphysial plate that is going to be responsible for the elongation of the bone after birth until puberty. And then there is that secondary ossification center remember that is formed, that really is just modeling the epiphysial head of the bone, and mainly it is going to be spongy bone as you see in the diagram to the right. And then I've briefly mentioned the importance of bone in maintaining calcium levels, the action of parathyroid hormone and thyroid hormone. And then finally I've briefly described the structure of a simple synovial joint. 07:04 So thank you very much for listening to this lecture. I hope you now have some understanding about the way in which bone forms and the way in which bone grows.
About the Lecture
The lecture Mineralization of the Bone Matrix by Geoffrey Meyer, PhD is from the course Bone Tissue.
Included Quiz Questions
Which cell is primarily responsible for endochondral and membranous ossification?
- Osteoblasts
- Osteoclasts
- Osteocytes
- Chondrocytes
- Chondroblasts
Osteocalcin is secreted by which of the following cells?
- Osteoblasts
- Osteocytes
- Macrophages
- Chondrocytes
- Osteoclasts
Articular cartilage receives nutrition from which of the following sources?
- Synovial fluid
- Medullary cavity
- Blood vessels
- Osteon
- Synovial membrane
Which of the following causes parathyroid hormone-induced stimulation of osteocytes and osteoclasts?
- Decreased serum calcium concentration
- Increased serum calcium concentration
- Increased serum magnesium concentration
- Decreased serum phosphate concentration
- Increased serum calcitonin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |