Playlist
Show Playlist
Hide Playlist
Microangiopathic Hemolytic Anemia: Etiology
-
Slides Microangiopathic Hemolytic Anemia.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
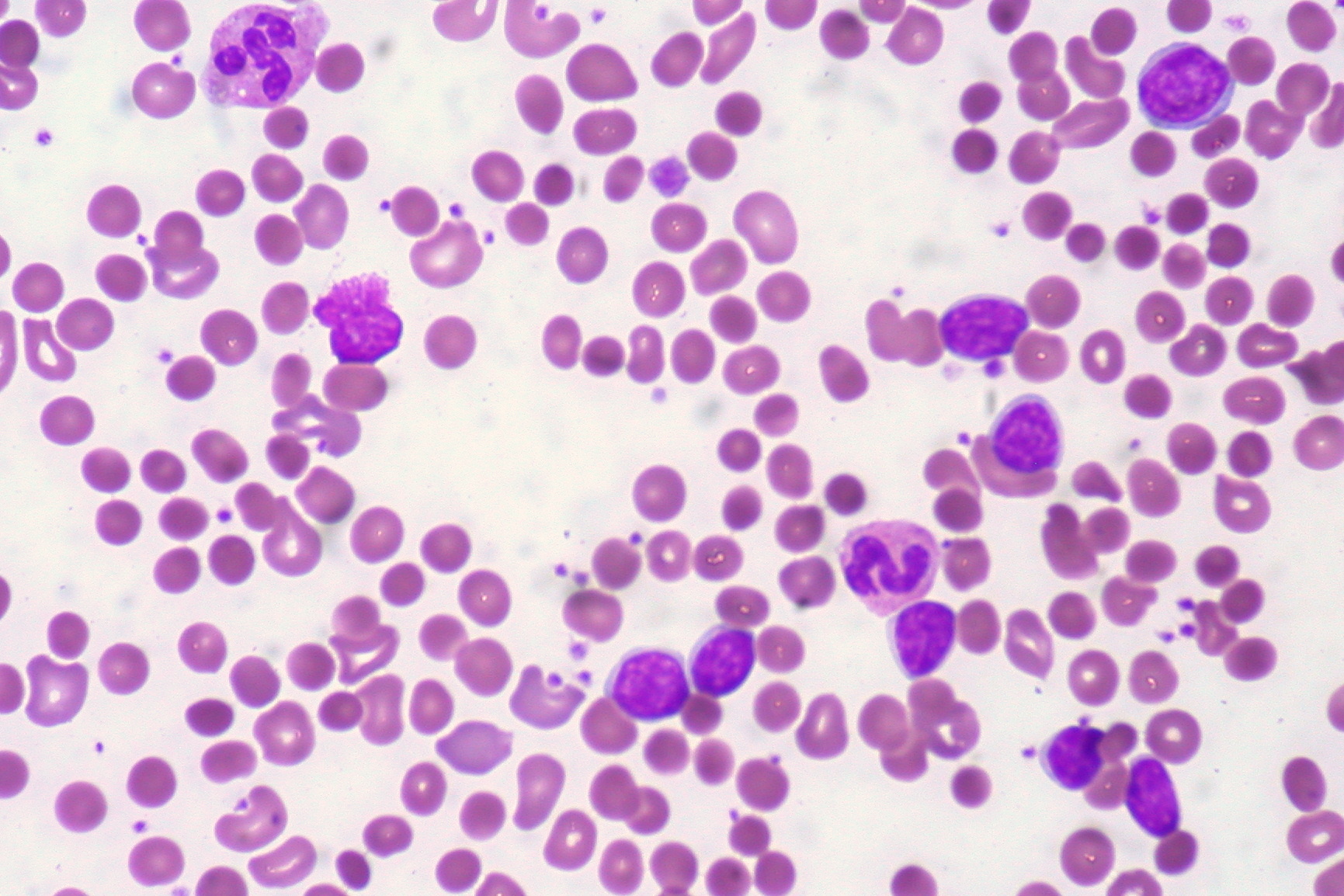
00:01 What if you're inside your blood vessel and you're an RBC, and you ended up hitting an obstructive and your head was chopped off? That's not very nice. 00:10 Welcome to microangiopathic hemolytic anemia. 00:13 And what we're going to do with our had been chopped off with an RBC referring to a schistocyte. 00:19 Hence you should wear helmets, helmets cells. 00:23 Let's continue. 00:24 So what we have here is inside my blood vessel, and we begin by looking at microangiopathic . 00:29 It's a mechanical damage, meaning to say that this is not a problem within the RBC. 00:35 So therefore, you would then refer to this as being an extrinsic problem. 00:39 By extrinsic we mean that the issue is taking place outside the RBC. 00:43 Where are you in your blood vessel? There are several potential mechanisms through which a red blood cell may be damaged by the blood vessel. 00:51 First, if a patient has a mechanical heart valve, that turbulent blood through the mechanical valve itself may induce damage to the red blood cells. 00:59 Or secondly, malignant hypertension can create a prothrombotic environment, resulting in small clots forming in the microvasculature. 01:07 As the red blood cells try to pass through these occluded vessels, their cell walls are deformed and ultimately damaged. 01:12 Continuing. 01:13 So let's say that you're in a little blood vessel and in the little blood vessel, you are then forming a thrombus. 01:20 Why? Well, that thrombus formation is not homeostatic, in terms of it wasn't dissolved quickly, and you have excess thrombi in your microvasculature. 01:33 Well, same consequence. 01:35 We talked about hypertension maybe or mechanical type of issues with heart valves. 01:40 But then if you have little thrombi, in which it offers resistance to an RBC to the point, it's actually causing extrinsic damage to the RBC, here, once again, they are we see what gets sheared, it look like it's just the same. 01:52 You call this a helmet cell. 01:54 The three conditions that often are associated with thrombotic disorders include DIC, TTP, and HUS. 02:04 Couple of things real quick, if it's DIC, it's devastating. 02:08 If this patient, when you see this patient with DIC rolling into your room, then this is not good because this is as close to death as you shall see with the patient There's a bleeding thatt's taking place in every single orifice. 02:22 Every single platelet has been consumed, every single coagulation factor has been consumed. 02:29 So therefore, you're going to find an increase in PT, PTT, bleeding time, or you're going to find an decrease in platelet count. 02:36 And so therefore, you have all this thrombi up and down the body guaranteed, your patient DIC is going to have what kind of anemia? It will be a normocytic hemolytic type of microangiopathic hemolytic anemia. 02:51 Clear. 02:53 Now, the triggers for DIC are quite unique. 02:57 Maybe, maybe it was Acute Myelogenous Leukemia type 3. 03:02 How many letters in DIC, 1-2-3, M3. 03:08 Maybe it was amniotic fluid emboli. 03:11 Maybe it was sepsis. 03:12 Sepsis is a big one. 03:14 Maybe it was some type of venom, maybe perhaps from snake venom. 03:18 So the origin or the true etiology of the DIC, it's a little peculiar, but when it takes place and you have that trigger, oh, it's really dangerous, really dangerous, close to death, if not already.
About the Lecture
The lecture Microangiopathic Hemolytic Anemia: Etiology by Carlo Raj, MD is from the course Hemolytic Anemia – Red Blood Cell Pathology (RBC).
Included Quiz Questions
What is the term used to describe an RBC that is abnormal in shape due to mechanical shearing and destruction?
- Schistocyte
- Dacryocyte
- Echinocyte
- Acanthocyte
- Spherocyte
Which of the following conditions are the most likely causes of microangiopathic hemolytic anemia?
- Disseminated intravascular coagulation, hemolytic uremic syndrome, thrombotic thrombocytopenic purpura
- Diabetes mellitus, disseminated intravascular coagulation, hemolytic uremic syndrome
- Hemolytic uremic syndrome, thrombotic thrombocytopenic purpura, idiopathic thrombocytopenic purpura
- Diabetes mellitus, idiopathic thrombocytopenic purpura, thrombotic thrombocytopenic purpura
What are the typical lab findings seen in disseminated intravascular coagulation?
- Low platelets, increased PT, increased PTT, increased bleeding time
- Low platelets, increased PT, increased PTT, normal bleeding time
- Normal platelets, increased PT, increased PTT, increased bleeding time
- Normal platelets, increased PT, normal PTT, normal bleeding time
- Low platelets, normal PT, normal PTT, increased bleeding time
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |