Playlist
Show Playlist
Hide Playlist
Meningioma: Clinical Presentation and Evaluation
-
Strowd CNS Tumors Meningioma.pdf
-
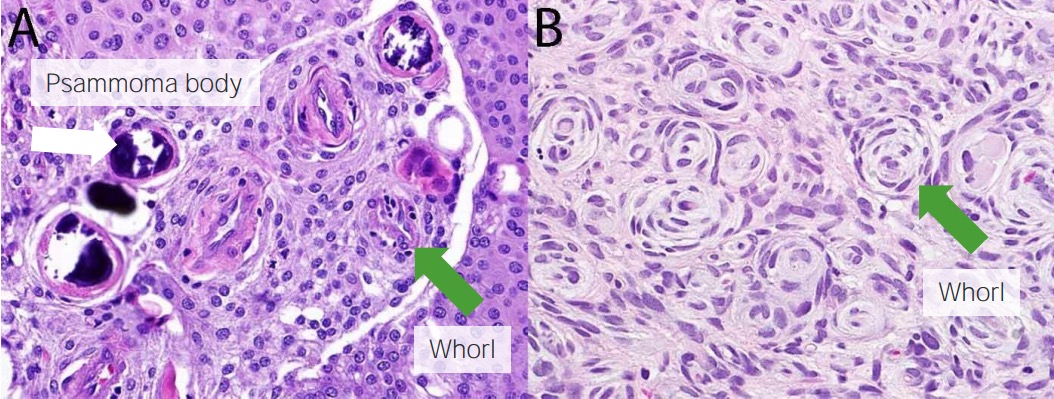
Download Lecture Overview
00:01 How do patients present with a meningioma? What's listed in that clinical vignette that should tip us off to be concerned about a meningioma? Well, first many of these are incidentally discovered. 00:12 So patients may present with a motor vehicle accident or headache and undergo an MRI. 00:17 And we find this incidentally. 00:18 We shouldn't have found that it wasn't causing symptoms. 00:21 Meningiomas are found in up to 1% of all brain MRIs. 00:25 All patients that are walking around we see 1% may have an incidental meningioma. 00:31 The other presentation is a patient may be symptomatic. 00:34 So what types of symptoms do we see arise from meningiomas? Well, symptoms can occur because of compression of surrounding structures. 00:41 And patients may present with a focal neurologic deficit from compression of that structure. 00:47 We can see blockage of cerebrospinal fluid flow and patients may present with altered mental status from hydrocephalus or increased intracranial pressure from a problem with cerebral spinal fluid dynamics. 00:59 We can see invasion into surrounding brain tissue and see seizures in some of those patients. 01:04 And we can even see them in the spine and so some patients may present with spinal symptoms, or a paraparesis weakness below a level of the spinal cord. 01:15 Where do we see meningiomas? Well, this schematic is a good representation of where they can be seen on brain imaging. 01:21 We can see them at the skull base, the base of the skull down beneath the brain in places like the lateral sphenoid wing, the medial sphenoid wing, the olfactory groove is a very common place it's commonly tested olfactory groove meningiomas, and even down at the base of the brain and the foramen magnum. 01:39 We can see them in other midline skull base structures like the cavernous sinus and those patients can present with eye movement abnormalities. 01:47 The tuberculum sellae or around the sella turcica that area around the pituitary, and the petroclival junction, which is right in the temporal lobe and may present with seizures. 01:58 We commonly see meningiomas in the convexity of the brain. 02:01 And here you see some examples of where those may occur. 02:04 The parasagittal area and the lateral convexity, as where as parafalcine right next to the falx cerebri, which does divides the two halves or hemispheres of the brain. 02:16 How do we evaluate patients with a meningioma? Well, classically, we think about doing CTs and MRI scans. 02:24 Both can give important signals for what the diagnosis may be. 02:28 And we'll look mostly at MRIs and look at the imaging signature of meningiomas on an MRI. 02:35 The classic imaging findings include a homogeneously enhancing a white dural-based lesion with a dural tail with or without invasion of adjacent brain. 02:47 And here you see on the left, a parafalcine meningioma. 02:50 You see it's homogeneously enhancing. 02:52 The entire tumor is very white and all the same signal intensity. 02:56 And we can start to see that there's some contrast extending along the dural surface that may indicate a dural tail. 03:04 And we'll see that in a few subsequent slides. 03:06 Another good example here of a parafalcine meningioma. 03:11 For patients who undergo surgery, and we'll talk about surgery in a minute, the classic histologic finding, there are two key things that we should think about. 03:19 The first are whorls, which we'll see in a minute and psammoma bodies, which are important board and testable buzzwords to think about when you're evaluating a patient with meningioma. 03:29 Here we see an example of a whorl, also in the middle of whorl as circular structure, and then some psammoma bodies. 03:37 These small round red inclusions within the meningioma cells that suggest a diagnosis of meningioma. 03:46 On imaging, we talked about a dural tail, which is a very important imaging signature that hints at a diagnosis of meningioma. 03:53 This is the enhancing, the contrast enhancing edge extension of the tumor along the dural surface, which you can see here with the green arrow. 04:03 We also see this. 04:04 This is a nice example of a cerebellopontine angle meningioma, a meningioma at the CP angle, with a dural tail extending along the medial structures of the meninges and skull base. 04:16 And meningiomas can occur anywhere. 04:18 And here we see a temporal pole meningioma at the just anterior portion of the left temporal lobe, probably presenting with seizures, or maybe aphasia, difficulty with language. 04:28 And here we see some surrounding and invasion or irritation of the brain parenchyma. 04:33 On the left scan, this is a T1 post-contrast imaging showing homogeneously enhancing lesion, which is consistent with a meningioma. 04:42 And on the right, we see some surrounding swelling, or edema white signal T2 signal in the brain indicating swelling around this lesion, which may indicate a higher grade. 04:55 When we classify meningiomas, we classify them based on their grade. 04:59 And we think of three grades, which is outlined by the World Health Organization criteria. 05:04 WHO grade I meningiomas are benign. 05:07 And this is the vast majority of meningiomas that we see making up 80% of meningiomas. 05:13 They are benign. 05:14 And there are a number of types that our pathologist say they describe and see when we look histologically. 05:20 And here are some examples of those, that I don't need you to remember all the individual names. 05:26 Histologically, we don't see that these tumor cells are dividing. 05:29 There's only occasional mitotic figures. 05:31 Mitosis is where you see a cell in the active division and we see that rarely for WHO grade I benign meningiomas. 05:40 And the rate of recurrence for these benign tumors is very low ranging 7 to 25%, depending on the treatment. 05:47 We can compare that to grade 2 meningiomas. 05:49 These are less common. They make up 17% of meningiomas. 05:53 There are also some types which I don't need you to remember all those names, but some are atypical, clear cell, and choroid meningiomas. 06:01 Histologically, we see that these are slightly more aggressive. 06:05 The cells are dividing. There is more mitotic activity. 06:08 There may be some brain invasion like we saw in that temporal pole meningioma on their MRI scan a few slides ago. 06:15 And we typically see three or more other features that suggest a higher grade or more aggressive tumor, prominent nucleoli, increase cellularity or cells, small cells with high nuclear-to-cytoplasmic ratio, which you shouldn't see in a normal cell. 06:31 A sheet light growth pattern, meaning there's a lot of cells growing all next to each other, and localized spontaneous necrosis. 06:38 And there's a slightly higher recurrence rate for these tumors ranging 30 to 60%. Again, depending on the treatment. 06:46 Grade III or malignant meningiomas. 06:49 These are cancers are uncommon. 06:51 They make up 1.7, less than 2% of meningiomas and are not frequently seen. 06:57 They are malignant, this is a type of cancer. 07:00 There are certain types that I'd like you to know of these names papillary, anaplastic, and rhabdoid meningiomas, because it means that's a more aggressive tumor. 07:10 And we see that histologically. 07:12 The cells are actively dividing with 20 or more mitoses, or actively dividing cells seen in each pathologic slide. 07:21 We see loss of the typical growth pattern infiltration of the brain, atypical mitosis, weird looking cells, and a multifocal spontaneous necrosis pattern in some patients. 07:32 And recurrence rate is very high for these malignant meningiomas ranging from anywhere from 60 to up to 94%.
About the Lecture
The lecture Meningioma: Clinical Presentation and Evaluation by Roy Strowd, MD is from the course CNS Tumors.
Included Quiz Questions
Which of the following is a characteristic histologic finding of a meningioma?
- Psammoma bodies
- Pseudopalisading
- Hypercellular Antoni A areas
- Chicken-wire capillary pattern with "fried egg" cells
- Rosenthal fibers
Which one of the following features best characterizes the histologic appearance of a grade I meningioma?
- Occasional mitotic figures
- Prominent nucleoli
- Small cells with high nuclear-to-cytoplasmic ratio
- Loss of typical growth patterns
- Sheet-like growth
Which of the following is a type of grade III meningioma?
- Papillary meningioma
- Psammomatous meningioma
- Metaplastic meningioma
- Choroid meningioma
- Clear-cell meningioma
Which is a histologic feature of a grade II meningioma?
- Localized spontaneous necrosis
- 20 or more mitoses per 10 high-powered fields
- Infiltration of the brain
- Multifocal spontaneous necrosis
- Loss of typical growth patterns
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |