Playlist
Show Playlist
Hide Playlist
Membranous Nephropathy
-
Slides NephroticSyndrome RenalPathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
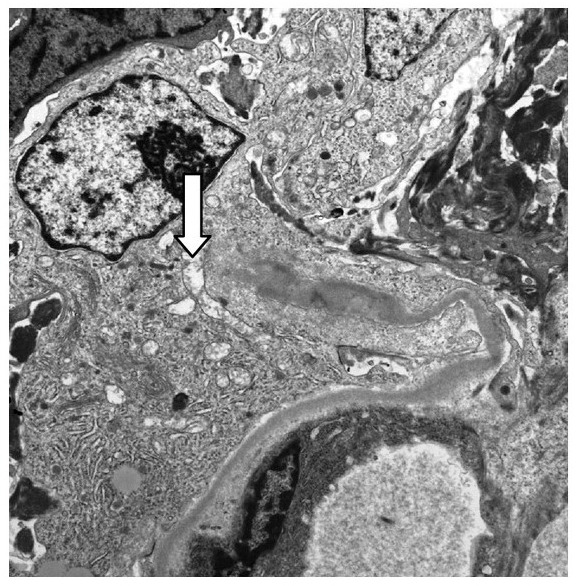
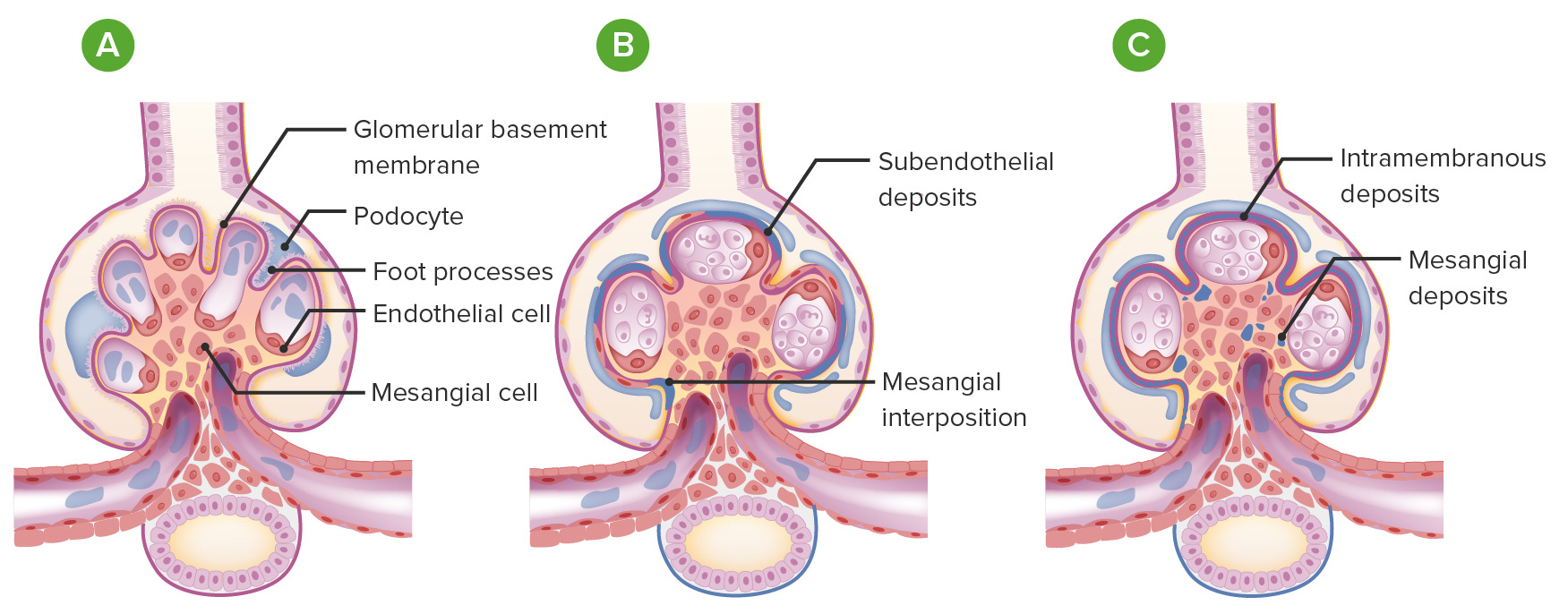
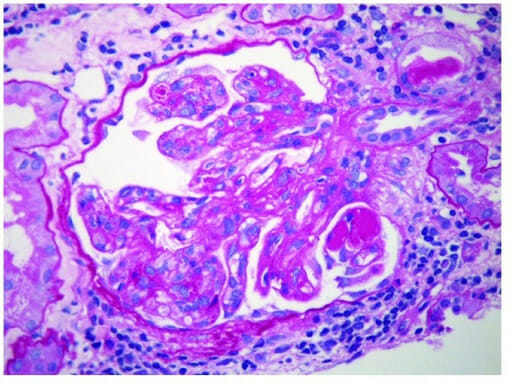
00:00 We’ll go to our third type of nephrotic syndrome. 00:04 Our first minimal change, second, FSGS, let’s talk about Membranous as the name implies, it will be the membrane that will be affected and depending as to which demographics you’re dealing with, well, some would say that this is the most common that’s found in adults, but be careful here, whereas in other demographics in populations and such would say that FSGS is in adults. 00:26 Well, both are true. You have to know both. 00:28 If you’re dealing with Hispanic population and you’re dealing with African-American population, then, you’re looking at in adults, you’re looking at FSGS being quite common and we talked about HIV patients. 00:41 If it is an adult 40 year old approximately Caucasian male, then you’re thinking at membranous. 00:48 Now, once you get your patient down and in this patient is a Caucasian male, approximately 40’s coming in, and they’re presenting with what? A generalize edema, you’ll have greater than 3.5 grams of protein that’s being lost, you have lipoid accumulation, and you know this is membranous maybe may not have hypertension. 01:06 High incidence in teenagers, young adults. 01:09 There is going to be complete thickening of the membrane. 01:14 Membrane, what you do not see here is proliferative, is that clear? At some point, when we get into MPGN, completely different diagnosis. 01:24 Students tend to get that confused. 01:27 Don’t do that anymore. 01:28 So in H&E, you’ll find the entire glomerulus membrane which is now then become thickened. 01:33 Electron microscopy is important for you to understand. 01:37 Okay, now, let’s say that you have the membrane that’s being involved, okay, great. 01:43 And at the same time, you also find that on the side of the podocyte, where are you? You’re inside. Underneath that podocyte, you end up finding deposit, what kind of deposit would you call this? Subepithelial type of deposit. 01:58 That you’ll have to memorize please. 02:00 And granular deposition, sure, why? And by the way, on what kind of biopsy pattern? Good, Immunofluorescence. 02:07 And here, you’ll find IgG or C3 and it will be what kind of deposit? Here, if you take a look at the left light microscopy, you’ll find the entire glomerulus has been involved and you find thickening of that membrane, point number one. 02:25 Point number two, the figure on the right with electron microscopy, first and foremost, is the membrane involved? Yes, it is. 02:34 Who is your patient? Most likely a 40-year-old Caucasian male adult, obviously. 02:39 And that deposit which is a dark deposit, well, that membrane looks messed up. 02:44 What side of this? It looks like it’s the foot process right and above, so underneath the foot process is a subepithelial deposit. 02:56 That is the dome in between the immuno-complexes or the domes would be the intervening basement membrane. 03:05 There is no proliferation here. 03:08 Here, on immunofluorescence, this is a picture in which we’re seeing our granular pattern. 03:14 The cartoon then represents membrane involvement and also, you have issues with subepithelial. 03:21 Would you perhaps find foot process being effaced or fused, what is this? Nephrotic syndrome. 03:28 What does that mean to you? Cytokines. 03:31 So therefore, what kind of effect may cytokines have on your podocyte? Fusion, so as a general rule, fusion of your foot processes could be found in all nephrotic syndromes, membranous, thickened membrane, spiked appearance will be the membrane and the dome in fact would be the subepithelial deposit. 03:51 Under membranous, important associations, you wanna keep in mind. 03:54 Usually primary, could be secondary. 03:56 Now, secondary, be careful. 03:58 Drugs, by drugs, I don’t mean heroine. 04:01 If it was heroine, you were thinking about FSGS, if it was HIV, you were thinking about FSGS. 04:07 The drugs here, may be chelators, Penicillamine. 04:11 May be antihypertensives, -prils, or anti-inflammatory, prescription drugs. 04:18 Malignancies are a big one: lung, colon, melanoma, membranous. 04:22 SLE, stop here for one second. Do not breeze past this. 04:27 SLE and its prototype that we have discussed is which one? Type IV classification. 04:36 One, two, three, four, give me a nephritic/nephrotic mixed picture that has four letters in it. 04:44 DPGN, what kind of deposit there? Subendothelial, you’ve heard of the wired loop. 04:49 This is 10% of the time with SLE could have membranous. 04:54 I told you we would come back and then, we’d discuss this, well, here we go. 04:58 So if you find an SLE patient, double stranded DNA, and subepithelial, this is membranous, is that clear? Infection, big time, hepatitis B, hepatitis C, be careful though, this is membranous. 05:10 The reason I say be careful is because with the hepatitis C virus, oftentimes associated with a clinical manifestation called cryoglobulinemia, and that cryoglobulinemia may actually may give you a picture of what’s called MPGN. 05:26 We’ll talk more about that later but I want you to give yourself some important secondary causes, Prognosis, often progresses General supportive measures for all patients in BP control, diatary sodium restriction, treatment of hyperlipidemia, minimisation of proteinuria with ACE inhibitors, and diuretics to control edema patient with mild to moderate disease might undergo spontaneous remission somina suppressive therapy should be reserved for those at the highest risk for developing progressive kidney failure This patients treated with rituximab or cyclophosphamide combined with glucocorticoids
About the Lecture
The lecture Membranous Nephropathy by Carlo Raj, MD is from the course Glomerulonephritis.
Included Quiz Questions
Which of the following conditions is most commonly seen in African Americans?
- Focal segmental glomerulonephritis
- Membranous nephropathy
- Membranoproliferative glomerulonephritis
- Minimal change disease
- Lipoid nephrosis
Which of the following is correct regarding the electron microscopic findings seen in membranous nephropathy?
- Immunoglobulin-containing deposits along the basement membrane with spike and dome appearance.
- Immunoglobulin-containing deposits along the endothelial membrane with spike and dome appearance.
- Immunoglobulin-containing deposits along the capillaries with spike and dome appearance.
- Immunoglobulin-containing deposits along the mesangium with spike and dome appearance.
Which of the following is found in post-streptococcal glomerulonephritis?
- Subepithelial deposits
- Subendothelial deposits
- Mesangial deposits
- Membranous deposits
- Subepithelial and membranous deposits
Which of the following statements is incorrect regarding focal segmental glomerulosclerosis?
- Most commonly seen in Caucasian adults.
- Only 15-20% of patients respond to corticosteroids.
- Most commonly seen in Hispanics and African American adults.
- It is often the primary glomerular disease in the elderly.
- It is associated with HIV.
Which of the following is NOT a feature of the biopsy of membranous nephropathy?
- Hypercellularity of the mesangium on light microscopy
- Thickened glomerular basement membrane on light microscopy
- Subepithelial deposits on electron microscopy
- Effacement of the podocytes on electron microscopy
- Granular pattern on immunofluorescence
Which of the following statements is incorrect regarding membranous nephropathy?
- It has a low incidence in young adults.
- It is the most common cause of nephrotic syndromes in Caucasian adults.
- H&E shows diffuse thickening of the glomerular capillary wall.
- It is seen in 10% of SLE patients.
Which of the following features is found in membranous nephropathy?
- Membranous and subepithelial deposits
- Membranous and subendothelial deposits
- Subepithelial and subendothelial deposits
- Membranous deposits only
- Subepithelial deposits only
Which of the following leads to the formation of varicocele in a patient with membranous nephropathy?
- Left renal vein thrombosis
- End stage renal disease
- Right renal vein thrombosis
- Renal artery thrombosis
- Lymphadenopathy
Which of the following infections is not commonly associated with membranous nephropathy?
- Rheumatic fever
- HBV
- HCV
- Syphilis
Which of the following is a characteristic feature of membranous nephropathy?
- Granular immunofluorescence pattern
- Linear immunofluorescence pattern
- Subendothelial immune complex deposition
- Mesangial immune complex deposition
- Anti-basement membrane antibodies
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |