Playlist
Show Playlist
Hide Playlist
Membranous Nephropathy – Nephrotic Syndrome
-
Slides Nephrotic Syndromes.pdf
-
Reference List Nephrology.pdf
-
Download Lecture Overview
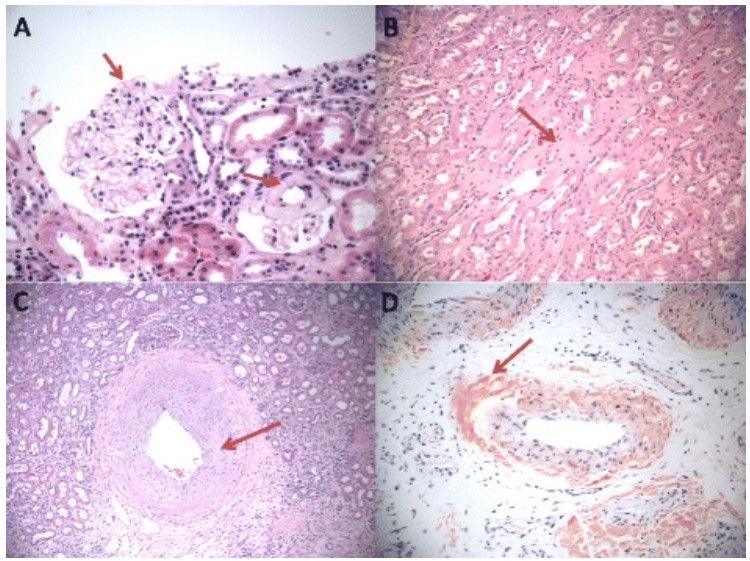
00:01 So let's talk a little bit more about membranous. 00:04 It's the second most common form of nephrotic syndrome seen in adults. 00:08 FSGS or focal segmental glomerulosclerosis is actually most common. 00:13 Membranous occurs in all ethnic groups, but it's most common in men over the age of 40 years. 00:19 When we think about the etiology or causes of membranous about 70% of cases will have what we call the primary form of membranous. 00:27 We're going to talk about that just in a few moments. 00:29 Secondary forms of membranous include things like infections (Hepatitis B to a lesser extent hepatitis C), syphilis. 00:39 And we also have malignancy associated that would be lung, breast, gastrointestinal cancers, which are most common and then finally drug associated membranous nephropathy which would be drugs like gold penicillamine which we used to use from rheumatoid arthritis and NSAIDs, and the last category is autoimmune, and that would include lupus. 01:03 So let's talk about primary membranous nephropathy. 01:06 So when we think about the primary form, it's really an autoimmune disease mediated by IGG antibodies that are directed to an antigen, a self antigen which is the m-type phospholipase A2 receptor. 01:19 So this is a schematic that actually diagrams exactly what I'm talking about. 01:23 So in patients who have membranous remember we talked about patients with glomerular disease have a genetic predisposition some kind of environmental trigger and a tendency towards autoimmunity. 01:33 So what this environmental trigger is? We don't know but in the case of membranous what happens is that self protein now becomes antigenic. 01:41 If you look at my diagram over here what you can see at the bottom of the slide is the lining of the capillary lumen. 01:47 The blue area is going to be our glomerular basement membrane. 01:50 The pink is our podocytes, and those little end pieces are podocyte foot processes that are actually attaching to the underlying basement membrane. 02:00 The little red circles represent the antigen mPLA2 to that's our phospholipase A2, antigen which is now recognized as foreign. 02:08 Now what happens when we recognize as foreign, we or our patient who has this disease are going to generate IGG antibodies anti-PLA to our antibodies against that antigen. 02:20 Once those antibodies are generated, they are then going to bind to that antigen and what happens when we have antigen and antibody binding to each other they form an immune complex. 02:31 When immune complex is form we then get activation of complement. 02:36 When complement is activated. 02:38 Remember the ultimate pathway for complement is going to be turning on that membrane attack complex and when that membrane attack complex gets turned on, then we ultimately have protease that are released that ultimately degrade that podocytes so we have necrosis apoptosis and we have actin cytoskeleton rearrangement of this foot processes. 02:59 And our ultimate, the conclusion will be that our patients will have high grade proteinuria. 03:07 So how do our patients actually present or what happens they present with nephrotic syndrome, some clues that are going to be helpful in terms of the diagnosis is that they will have nephrotic range proteinuria meaning that they have greater than 3.5 grams per 24 hour period of time. 03:25 Remember in our example, our gentleman had nine grams. 03:28 Our patients are hypoalbuminemia, but often times below 2 grams per deciliter just like in our example. 03:35 Our patient had a serum albumin of 1.9 grams per deciliter again, because they have high grade proteinuria they're losing that albumin through their urine. 03:42 They have edema, they're often edematous in volume overloaded. 03:46 And they have hyperlipidemia and can have lipiduria. 03:50 And if you're lucky enough to look at that urine underneath a microscope, you may see those old fat bodies or fatty casts. 03:56 Otherwise the sediment is relatively bland. 03:57 We're not going to see any other cellular casts. 04:01 When we do serological tests looking at their blood their serum complements are normal. 04:05 And that may be a little counterintuitive because I just talked about how when an antigen and an antibody binding together that actually stimulates the classical pathway of complement activation. 04:15 But remember where this is happening, this is on the sub epithelial side, so we don't see it in a systemic fashion and we're not going to be seeing serum compliments getting used up. 04:25 So if we're thinking about primary membranous, we can actually measure those PLA to our antibodies and their positive and about 70 to 80 percent of people who have primary membranous. 04:36 There's also another antigen that's involved. 04:39 That's thrombosed fondant type one domain containing 7A (THSD7A) and these are positive in about 10% of people who have primary membranous. 04:49 So about fifty percent of those patients who are PLA2R negative are actually going to be positive for THSD7A. 04:57 So we also want to rule out secondary causes of membranous. 05:01 So our patients may have Hepatitis B or C. 05:04 So it's important to check those hepatitis serologies, or they may have an autoimmune form like lupus. 05:11 So it's important to look at anti-nuclear antibodies ANA and double-stranded DNA which measures lupus activities. 05:19 And then of course, the definitive diagnosis is going to be with a renal biopsy. 05:25 So before we looking pathologically what happens in our patients with membranous, it's important to review the normal glomerular histology. 05:32 This is a beautiful image of a glomerulus and what you can see here and what I want to point out are these beautiful capillary loops here. 05:39 Look how open they are and how delicate and perfect they are. 05:42 So the cells that are going to be located here are glomerular epithelial cells, the podocytes and our endothelial cells which line that capillary lumen. 05:51 And then in the areas in between kind of the stock of that glomerulus these are masangial cells and they produce matrix in their cells that reside there as well. 06:02 Okay, so when we have a patient who's presenting with membranous, what do we see on our biopsy? Well, we're going to take one of those cores of biopsy and we're going to look at light microscopy. 06:12 There's a couple of different stains that we can do by light microscopy. 06:15 But one of the better stains to look at which will bring out basement membranes is the Jones silver stain and on Silver stain what we can really appreciate here is that there is the spike and dome or spike appearance that you can see, so it's illustrated over here with our arrow. 06:31 Is that that capillary loop has a spiky appearance because of the fact that you have these immune complexes that don't take up stain. 06:39 And they're sitting there in the sub epithelial space. 06:41 Remember the podocytes are injured because of that immune complex. 06:45 So they're cranking out a lot of basement membrane and when they do that that kind of gets extruded in between those actual immune complexes therefore giving it kind of a spiky or spike and dome appearance. 06:56 So very pathognomonic if you hear that you really need to be thinking about membranous and it's something that will probably come up on your board test. 07:05 We also want to take one of those cores that we get from our biopsy and we want to look at the immunofluorescence. 07:10 So here on our frozen section looking at immunofluorescence. 07:13 We see our heavy chain IGG. 07:16 Remember our patients are making those IGG antibodies that are directed at that antigen mPLA2R. 07:22 So we can see that on our immunofluorescence with variable amounts of C3 complement. 07:26 And what you would can appreciate on this particular slide here, is that you have almost like a powdered sugar to appearance where these immune the IGG is just kind of sprinkled on the outside or outer aspect of that capillary loop. 07:43 Finally, we have the electron microscopy and what's blown up here and what you can appreciate is kind of a loop or one of our loops of our capillary loop on the inside is the endothelium that kind of darkened area is their glomerular basement membrane. 07:57 And then on the outer area is where our podocytes foot processes are residing. 08:01 And what I'm calling your attention to with the arrows is that if you can appreciate kind of that darker area within that glomerular basement membrane, those are our sub epithelial deposits. 08:12 That is what we are seeing in membranous, so it's on the sub epithelial side meaning that it's just below the podocytes cell body, but it's just above that glomerular basement membrane. 08:21 We can also see because those podocytes are injured. 08:24 We're going to see actin cytoskeleton rearrangement and we see foot process effacement or we might actually see denuded areas of basement membrane where they've actually been picked off from the underlying basement membrane. 08:37 So we think about the course and how our patients do over time once they're diagnosed with membranous. 08:42 There's a couple of different ways that they can go. 08:44 So sometimes patients are lucky enough to have a spontaneous remission. 08:49 Probably occurs on the order of 5-30% at 5 years. 08:53 That means that when we're talking about a remission patients are able to achieve less than 200 milligrams of proteinuria per day. 09:00 We tend to see that in a younger population more females than males tend to enter a spontaneous remission. 09:05 We can also see a spontaneous partial remission. 09:07 That means that they're making less than 2 grams of proteinuria per day. 09:11 That probably occurs in about 25-40% of patients at five years. 09:15 But in about 14% of patients have five years if their untreated and we don't have any therapy for those patients about 41 percent of those patients are going to progress to end stage renal disease at 15 years. 09:28 So again, if that patient is sitting there in front of us, what's most critical is to figure out who is at risk for progression, for progressing, because those are the patients that we really want to target. 09:38 So things to think about are patients who are older age at the time that membranous is diagnosed. 09:45 Males more than females, so male gender just like we talked about in chronic kidney disease is one of those risk factors for progressing. 09:53 Having an increased serum creatinine at the time of diagnosis and if you think about what that means that just means that, that patient probably has had membranous for a longer period of time. 10:01 And they have not yet entered spontaneous remission, so we know already that they're at risk for progressing. 10:07 And patients who have high grade proteinuria at presentation. 10:11 So if they have greater than 8 grams of proteinuria and significant nephrotic syndrome then those patients really are at risk. 10:17 And finally, on biopsy, if I see the presence of tubulo interstitial fibrosist meaning that my tubules and interstitium are starting to be scarred, that absolutely is a risk factor for that patient progressing. 10:31 So that comes to thinking about treatment for our patient. 10:35 So all patients regardless of what's going on, or regardless of their risk profile should receive nonspecific therapy. 10:42 And this is what we outlined at the beginning of the talk. 10:45 Those patients should be on ACE inhibitors and ARB's for RAAS suppression. 10:49 They should be on a loop diuretic like bumetanide, or furosemide to mobilize the volume that they've accrued from that edema. 10:56 They should absolutely have a low sodium diet and their blood pressure needs to be controlled at less on 130/80, and treatment of their hyperlipidemia often with a Statin. 11:06 Now, we do have something beyond nonspecific therapy and that's immune targeted therapy. 11:12 But I'm not going to give that to everybody that really needs to be reserved for people who are at risk for progression or for people who have such severe nephrotic syndrome or complications of nephrotic syndrome that they can't be controlled with just nonspecific therapy alone. 11:27 So those therapies include things like cyclophosphamide and prednisone that we administer over a six-month period of time. 11:34 Cyclophosphamide is an alkylating agent, it's not something to be used lightly. 11:38 So I'm only going to choose and target that population who's really at risk from succumbing to their disease. 11:44 Cyclosporine which is a calcineurin inhibitor can also be used in patients who can't tolerate cyclophosphamide and we can use that in combination with low-dose prednisone as an alternative. 11:55 And finally, there's rituximab. 11:57 A monoclonal antibody to CD20 and that likely will replace the others as first-line therapy.
About the Lecture
The lecture Membranous Nephropathy – Nephrotic Syndrome by Amy Sussman, MD is from the course Nephrotic Syndrome.
Included Quiz Questions
Which of the following is involved in the pathogenesis of primary membranous nephropathy?
- Autoantibodies to phospholipase A2 receptors
- Autoantibodies to glutamic acid decarboxylase
- Autoantibodies to type IV collagen
- Autoantibodies to structures within the nucleus
- Mismatch repair deficiency
Which of the following is compatible with a diagnosis of membranous nephropathy?
- Normal complement levels
- Low C3 and C4 levels
- Low C4 levels only
- Granular casts on urinalysis
- Microproteinuria
Which of the following is true regarding the histopathology of membranous nephropathy?
- Light microscopy reveals a spike-and-dome pattern.
- Immunofluorescence microscopy reveals a linear pattern of immunoglobulin deposition.
- Immunofluorescence microscopy reveals characteristic pauci-immune staining.
- Electron microscopy reveals mesangial deposits.
Which of the following predicts the progression of membranous nephropathy to ESRD?
- Tubulointerstitial fibrosis
- A serum protein level of >8 mg
- Female sex
- Young age
- Low serum creatinine level
Which of the following is part of the immune-targeted treatment for membranous nephropathy?
- Rituximab
- Low-salt diet
- ACE inhibitors
- Statins
- Loop diuretics
Which of the following is true about membranous nephropathy?
- Spontaneous remission is defined as <200 mg of proteinuria per day.
- Light microscopy reveals duplication of the basement membrane.
- Hodgkin lymphoma is commonly associated with membranous nephropathy.
- Immunosuppressive therapy is the first-line treatment.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Thank you. well organized. risk of progression was a good add in.
Very clear and structured lecture! I enjoyed the explanation of the subepithelial deposition on the diagram.