Playlist
Show Playlist
Hide Playlist
Membranoproliferative Glomerulonephritis (MPGN) – Nephritic Syndrome
-
Slides Nephritic Syndrome.pdf
-
Reference List Nephrology.pdf
-
Download Lecture Overview
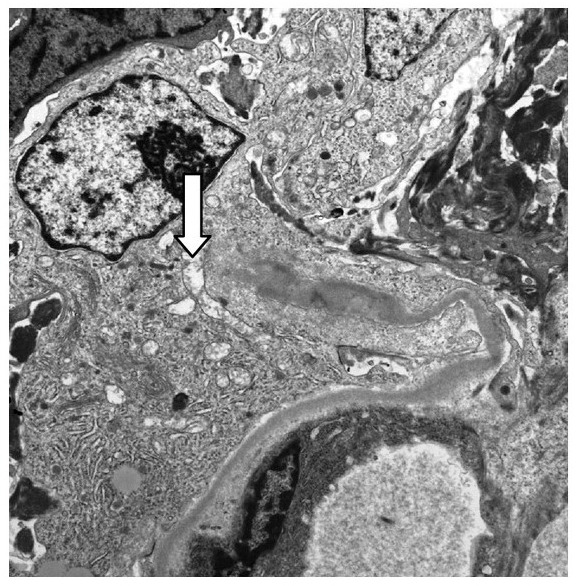
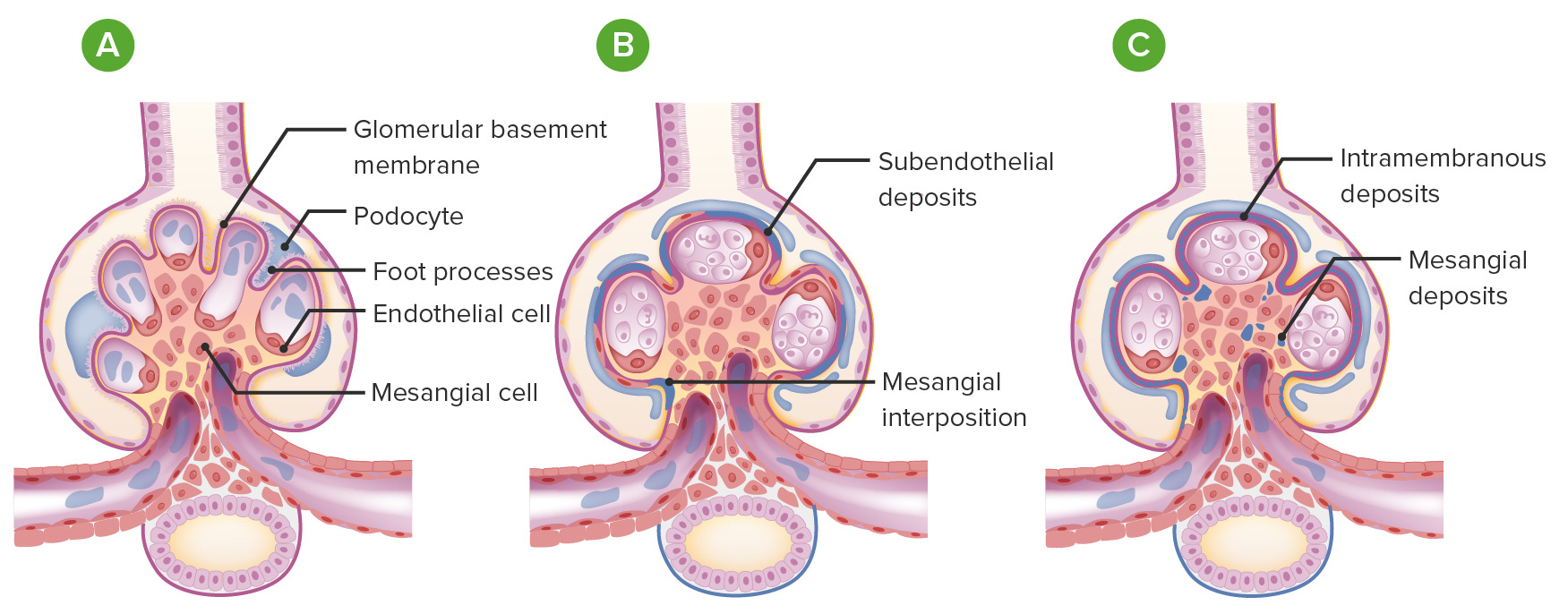
00:01 So, membranoproliferative glomerulonephritis, MPGN, can present, remember, with nephritic and nephrotic syndrome. 00:08 A little bit less common to see the nephrotic presentation alone. 00:12 We see that maybe about 10% of the time but we can also see features of both. 00:16 Now, we have a couple of different paradigms when we talk about MPGN. 00:21 The older paradigm which you may still see in some textbooks talks about subtyping MPGN based on its pathological classification. 00:29 So, we used to refer to Type I MPGN as being the classic type of MPGN in association with immune complex disease, Type II would be considered dense deposit disease, and Type III, very similar to Type I except there's subepithelial deposits in addition to the subendothelial deposits but clinically, there wasn't a big distinction between I and III. 00:51 Now, because that doesn't really make sense, we've actually changed our classification and we have a newer paradigm. 00:58 And what this paradigm really involves or invokes is that MPGN really is a pathological pattern of injury due to either immune complex-mediated diseases or complement-mediated injury. 01:12 And I think that's a much easier way to really understand what's happening in this particular glomerular disease. 01:19 So, let's talk about immune complex-mediated MPGN. 01:24 This can be due to things like infections. 01:28 Hepatitis C, by far and away, is one of the most common that we see in the United States in association with MPGN of the immune complex type. 01:38 There's other things to consider too. 01:40 Chronic bacterial infections, this can be subacute bacterial endocarditis or ventriculoatrial shunt infections. And finally, parasitic infections. 01:50 Again, if you're in the endemic region, things like schistosomiasis can also cause an immune complex mediated MPGN. 01:57 There's also autoimmune disorders. 01:59 Things like lupus, Sjogren's, rheumatoid arthritis, that can also cause an immune complex-mediate MPGN. 02:08 The dysproteinemias which are associated with monoclonal immunoglobulin deposition, so these are patients, remember, that may have things like multiple myeloma, CLL, and non-Hodgkin's lymphoma. 02:22 And what typically happens is monoclonal immunoglobulin-like chains are produced, they deposit, they lay down in the kidney, and they stimulate this MPGN pattern of injury. 02:34 And then finally, we have idiopathic. 02:36 And what that means is that we don't know what the cause is and it absolutely is a diagnosis of exclusion. 02:43 So, when we think about the pathogenesis of immune complex-mediated disease, it's exactly as we're talking about. It's an immune complex. 02:50 That means that the patient has an antigen, it could be either unknown in the case of idiopathic or it could be viral or bacterial. 02:59 They form an antibody directed at that antigen and it could be that these are either formed within the circulation so that you have deposition of these preformed circulating antigen antibody complex into the glomerular basement membrane, typically on that subendothelial site, that means that it's between those endothelial cells and the glomerular basement membrane, or you could have an actual antigen planted within that glomerular basement membrane insitu and then you form or the patient forms an antibody secondarily to it. 03:33 Once that forms, remember what happens. 03:36 Antigen antibody, we've got immune complex formation that is a potent stimulator or activator of complement by the classical pathway of complement activation and because of that, we see serologically in our patients, in their serum, they have a low C3, a low C4, and a low total complement. 03:55 That tells us complement, through the classical pathway of activation, is being stimulated. 04:00 So, let's just take a moment to remind ourselves of the complement pathway. 04:05 So, on the left, we see our classical pathway of complement and these, remember, are going to be activated by immune complexes, antigen and antibody. 04:16 When classical pathway is activated, we've got C1q and C4, that's why we see a low C4 in the serum. That activates C3 convertase. 04:27 That C3 convertase then activates C3 and C3 starts getting used up, and then activates C5 or the membrane attack complex, that is that C5b-9. 04:40 And when that happens, we've got focused target cell lysis. 04:45 Now, on the other side, we have the alternative pathway of complement activation. 04:49 This can be, perhaps, activated by bacteria or other factors. 04:53 Again, C3 convertase is activated and when that happens or when that is active, we are then going to have C3 activation. 05:05 Again, activating that C3a and C3b. We have opsonization of these immune complexes but again, we're going to have C5 stimulated, that membrane attack complex, and focused target cell lysis. 05:18 So, when we diagnose or we think about diagnosing the MPGN of the immune complex-mediated type, there's a couple of things that we wanna look for. 05:26 Number one, remember this is an acute nephritic syndrome. 05:29 We should see active sediment. 05:31 That means that that patient is gonna have those dysmorphic red blood cells, those red blood cell cast, microhematuria, on their urine analysis. 05:39 Remember, some of those patients can present nephrotically too. 05:42 This is one of those overlap syndromes where you can see patients with nephrotic range proteinuria and nephrotic syndrome. 05:48 Patients will have a low C3 and C4 in their serums. 05:54 So, low C3 complement low C4. Why is that? We just talked about this is the classical pathway of complement activation. 06:01 So, that makes sense. Now, if we're worried about an infection-associated MPGN and that is probably the most common cause in the United States, then we think about checking hepatitis C. We also want to check a rheumatoid factor. 06:16 That reason being, remember, rheumatoid factors are not just for rheumatoid arthritis. 06:20 These are IgM antibodies that are directed against the FC portion of IgGs. 06:26 So, nonrheumatic disorders characterized by chronic antigenic stimulation, that's what hepatitis C is doing. It can actually induce these rheumatoid factor productions. 06:36 So, it's not uncommon in the hep C-associated MPGN for us to see a positive rheumatoid factor which is our IgM and then our IgG directed against that HCV. 06:48 We also, if we're thinking about monoclonal immunoglobulin deposits, want to check for a serum protein electrophoresis. 06:57 We wanna see if those abnormal proteins are being generated in a monoclonal fashion within the bone marrow and if we do that, we wanna get that positive serum immunofixation or IFE. 07:08 We also can look for serum free light chains as well. 07:12 And it's important to note that this may not always be coming from the bone marrow. 07:16 Sometimes, you can get these monoclonal immunoglobulin light chain productions extramedullary, so they can be in lymph nodes as well. 07:23 Now, if we really wanna know what's going on with our patients with these glomelural disorders, we really need to do a renal biopsy. 07:30 And this is what our biopsy will show us. 07:34 So, on our first image over here, this is a light microscopy H and E of a patient who has MPGN of immune complex type. 07:42 And what we can see and what I want you to appreciate is how lobular in appearance that glomerulus looks. 07:50 It is hypercellular. Remember, these immune complexes and the subendothelial location are causing endothelial cell proliferation. 07:57 These guys become hypercellular and lobulated. 08:00 We can also do our Jones' silver stain and something that's really pathognomonic for having MPGN pattern of injury is having what we call a tram-tracking or double contouring of the basement membrane and that's what's illustrated right here in that arrow. 08:18 And it's interesting cuz think about what's happening. 08:20 Again, you've got those subendothelial immune complexes but they also secondarily injure potosites so we've got increase in glomerular basement membrane production. 08:29 So, you get a second layer of that GBM and that's what causes that double contouring or what we call that tram-tracking. 08:37 And sometimes you can see a mesangial cell that kind of scavenges an interpositions itself in between those 2 layers of basement membrane. 08:46 On immunofluorescence, we see IgM. 08:49 And I want you to notice where that's laying down. 08:52 Remember, I'm talking about subendothelial immune complexes so you can see how beautiful that immunofluorescence is. 08:58 It's just hugging that endothelium or that inner part of the capillary loops. 09:03 So, it's very smooth in appearance. 09:06 And then finally on electron microscopy, we can see those subendothelial complexes and that's really designated by that denser, kind of darker material that's in between the endothelial cell and the glomerular basement membrane. 09:21 So, how do our patients do over time? Well, for idiopathic MPGN, it's actually a prolonged course with a slow rate of disease progression. 09:30 So, typically about 30% will progress to end-stage renal disease within a 10 to 15-year period of time. 09:36 When it comes to treating our patients with idiopathic MPGN, there's really no good randomized control trial data out there. 09:44 So, we do treat our patients with glucocorticoids or steroids but it's not based on good evidence and that's simply because the disease entity really is relatively rare. 09:54 Patients often times, unfortunately, are not responsive to therapy. 09:58 There's limited data for other immuno therapies in this particular category and that includes cyclophosphamide, one of our alkylating agents, and mycophenolate mofetil which is an antimetabolite. 10:08 Again, these are case series and case studies but we don't have good randomized control trial in this particular population. 10:16 So, for an infection in autoimmune category, those patients do relatively well. 10:22 In particular, I'd like to mention hepatitis C. 10:25 Hepatitis C, because of our direct-acting antiviral therapy, has just exploded with being able to treat these patients so that as a nephrologist, I'm not seeing this disease entity anymore and I have to say, that is extremely gratifying. 10:41 Just within a 10-year period of time, seeing patients with MPGN in association with their hepatitis C to now where I rarely see a patient because we have therapies that are so effective in treating that particular patient population. 10:54 For patients who have autoimmune diseases, again, treating their underlying disease will help ameliorate what's going on from the renal manifestation. 11:03 Remember, MPGN is just a pattern of injury due to the underlying cause. 11:08 With a monoclonal immunoglobulin depositions, so, these are those dysproteinemic states that we talked about. 11:15 Things like plasma cell dyscrasias, some of the leukemias, the treatment is going to be really aimed at the underlying disease. 11:21 So, I wanna treat that plasma cell myeloma and I want to ensure that I have my hematology colleagues involved. 11:28 That may lead to some renal improvement in that particular patient population.
About the Lecture
The lecture Membranoproliferative Glomerulonephritis (MPGN) – Nephritic Syndrome by Amy Sussman, MD is from the course Nephritic Syndrome.
Included Quiz Questions
Which of the following statements is true regarding the alternative complement pathway?
- C3b is responsible for the opsonization of immune complexes.
- IgM and IgD bind complement proteins and activate them.
- C3 convertase activates the membrane attack complex for target cell lysis.
- Factor B is responsible for the activation of C4 convertase.
Which of the following is associated with MPGN?
- Low C3 and C4 levels
- Normal total complement levels
- Bland urinary sediments
- Suprapubic tenderness
- Decreased blood urea levels
Which of the following histopathologic changes is associated with MPGN?
- Tram tracking of the basement membrane
- Hypocellular and lobulated glomeruli
- Nodular glomerulosclerosis
- Spikes and domes in the basement membrane
Which of the following statements is true?
- Idiopathic MPGN has a slow rate of disease progression.
- Idiopathic MPGN is very responsive to glucocorticoids.
- Antiretroviral drugs do not improve the prognosis of HCV-associated MPGN.
- Liver and kidney transplantations are necessary for patients with HCV-associated MPGN.
Which of the following is associated with immune complex-mediated MPGN?
- Subacute bacterial endocarditis
- C3 dense deposit disease
- Obesity
- Pamidronate
What is the primary location of immune complex deposition in MPGN?
- Subendothelium
- Mesangium
- Subepithelium
- Basement membrane
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |