Playlist
Show Playlist
Hide Playlist
Mayer-Rokitansky-Kuster-Hauser Syndrome and MDA
-
Slides Mullerian Anomalies.pdf
-
Download Lecture Overview
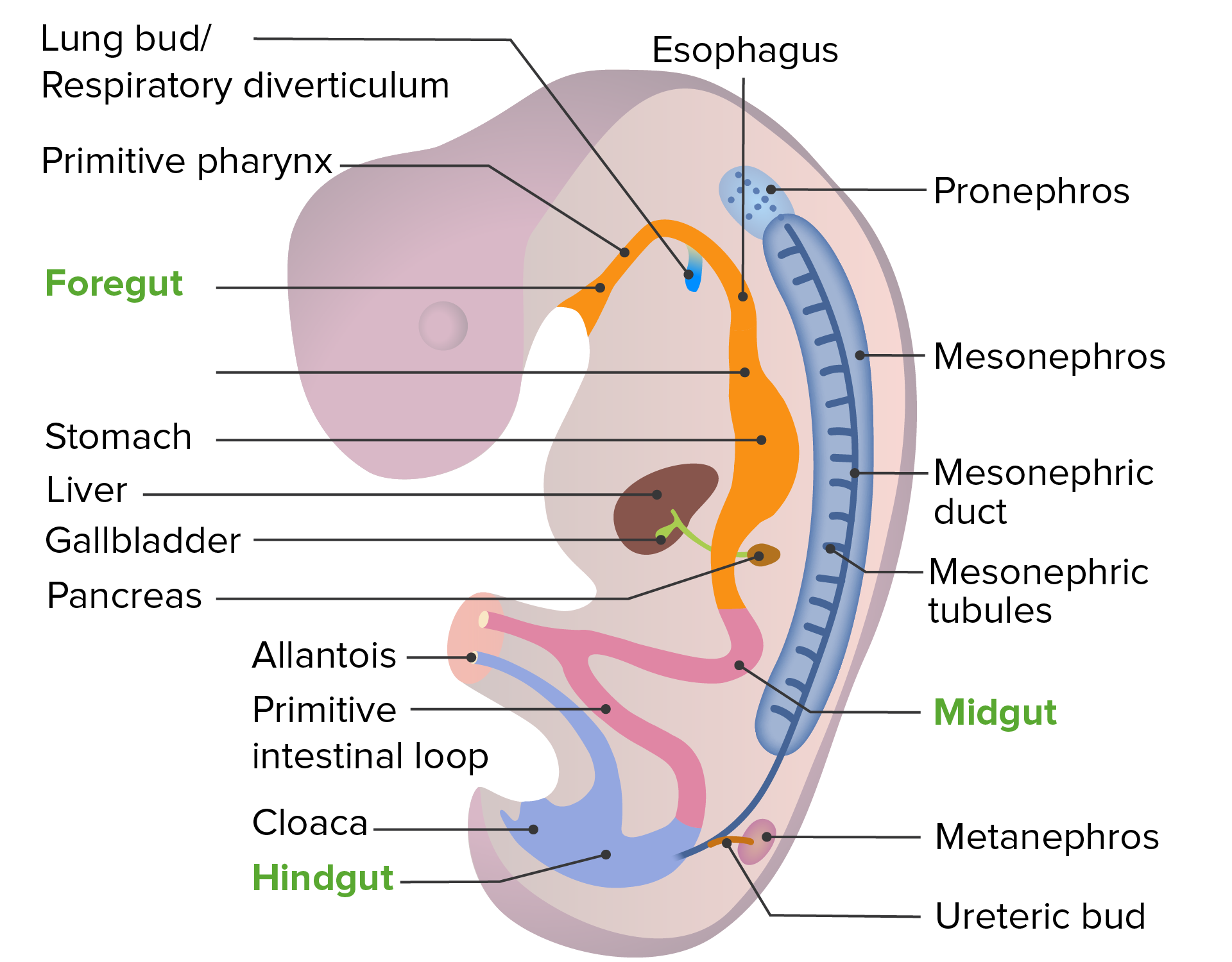
00:00 Let's now talk about a very rare syndrome called Mayer-Rokitansky-Kuster-Hauser syndrome. Here in this syndrome, this is a subclass of Mullerian agenesis. The incidence is low. In Finland, we know that the incidence is 1 in 5000. The cause is unknown; however, we think there might be a mutation in the gene for AMH. This causes excessive AMH activity in a female causing the paramesonephros or the Mullerian duct to regress. There is an increased prevalence of GALT mutation which is associated with galactosemia. This is reviewed in another lecture set entitled Primary Ovarian Insufficiency. WNT4 is another gene that potentially can be abnormal in these patients causing their uterine ducts not to form properly. Now I'd like to talk about Mayer-Rokitansky-Kuster-Hauser syndrome. There are 2 different types. There is symmetrical muscular rudimentary uteri. This patient usually has normal fallopian tubes. Let's now talk about type B. This patient has asymmetrical rudimentary uteri and/or absent hypoplastic fallopian tubes. Can this patient carry a pregnancy? I'll let you think about that. The answer is no. If she does have any rudimentary uteri, sometimes she can become pregnant in those rudimentary uteri and it's usually an ectopic because the uterus can't support the growth and you actually have a rupture of these rudiments. Let's talk about the reproductive outcomes in general though. You can have infertility not because there is something wrong with the ovaries but just the fact that you can't become pregnant very easily if you don't have a uterus. You can have recurrent pregnancy loss and again usually that's more than 2 losses lifetime but some definitions do say 3. Major anomalies are 3x more likely to be present in women who have RPL or recurrent pregnancy loss and you can have in general poor pregnancy outcomes including preterm birth less than 37 weeks, infant mortality, and low birth weight. Again, 25% of women who have Mullerian duct anomalies have preterm labor, breech presentations where the baby is foot first instead of head first and increased risk of intervention and perinatal mortality. 02:38 Let's now talk about the GYN outcomes with Mullerian duct anomalies. These patients can have dysmenorrhea or painful menses. They can also have dyspareunia which is painful intercourse. 02:52 Amenorrhea can also occur if there is abnormal rudiment development. Also, they can have endometriosis usually due to retrograde menstruation that occurs over a long period of time. 03:05 Let's now discuss the embryology of the paramesonephros or the Mullerian ducts. If you are male you will have Sertoli cells and Leydig cells in the testes. The Sertoli cells will secrete anti-Mullerian hormone which inhibits Mullerian duct development in the 46,XY male. However, if Sertoli cells are actually destroyed or you have gonadal dysgenesis, this will not occur and you can have 46,XY individuals who have patent Mullerian ducts. Please review gonadal dysgenesis for more information. 03:41 There are other genetic causes that we think of when we discuss Mullerian dysgenesis or abnormalities. 03:48 WNT4 is one as a gene that can cause these abnormalities, WNT7A, LHX1, and PBX1. I doubt you'll have any questions on this on the exam but this is just for your information. Let's do our checklist now. For diagnosis of Mullerian duct anomalies, it's usually done with an HSG, laparoscopy, or hysteroscopy. However, they can be found incidentally during the MRI for other causes. 04:18 Sonohysterograms and MRI are now the standard for diagnosis and a 3D ultrasound is a good alternative. Let's now review how we manage Mullerian duct anomalies. If a patient has a uterine septum and it's associated with recurrent pregnancy loss or obstetric complications or prematurity, we usually remove the septum by incision. This is typically performed by a reproductive specialist such as a reproductive endocrinologist and infertility specialist. Usually, if we find this incidentally, we don't remove it but we counsel the patient that it is possible that she could have poor obstetric outcomes and we inform her and then she can decide what she would like to do. Whatever the indication is, a hysteroscopic approach toward resection is important. There is really no reason to do an open procedure for these Mullerian duct anomalies. Thank you for listening and good luck on your exam.
About the Lecture
The lecture Mayer-Rokitansky-Kuster-Hauser Syndrome and MDA by Lynae Brayboy, MD is from the course Abnormal Menstruation. It contains the following chapters:
- Mayer-Rokitansky-Kuster-Hauser Syndrome
- Reproductive and Gynecologic Outcomes with MDA
Included Quiz Questions
Which of the following is NOT useful in diagnosing Müllerian dysgenesis?
- Ovarian biopsy
- Hysterosalpingogram
- Laparoscopy
- Hysteroscopy
- MRI
Which of the following is FALSE regarding Mayer - Rokitansky -Kuster -Hauser syndrome?
- Type A Mayer - Rokitansky - Kuster - Hauser syndrome has asymmetric rudimentary uteri and absent or hypoplastic fallopian tubes.
- Mayer - Rokitansky - Kuster - Hauser syndrome has increased AMH activity.
- Mayer - Rokitansky -Kuster -Hauser syndrome has increased GALT mutation.
- Mayer - Rokitansky -Kuster -Hauser syndrome is associated with galactosemia.
- Mayer - Rokitansky - Kuster - Hauser syndrome has a defective Wnt 4 gene.
Which of the following is NOT a common gynecological problem of Müllerian duct Anomalies (MDA)?
- Menorrhagia
- Dyspareunia
- Amenorrhea
- Dysmenorrhoea
- Endometriosis
Which of the following is NOT a reproductive outcome of Müllerian duct abnormalities?
- Molar pregnancy
- Infertility
- Recurrent pregnancy loss
- Preterm labor
- Breech presentation
Which of the following genes are NOT involved in Müllerian duct abnormalities?
- FAP
- Wnt 4
- Wnt 7A
- LHX1
- PBX1
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |