Playlist
Show Playlist
Hide Playlist
Malaria in Children
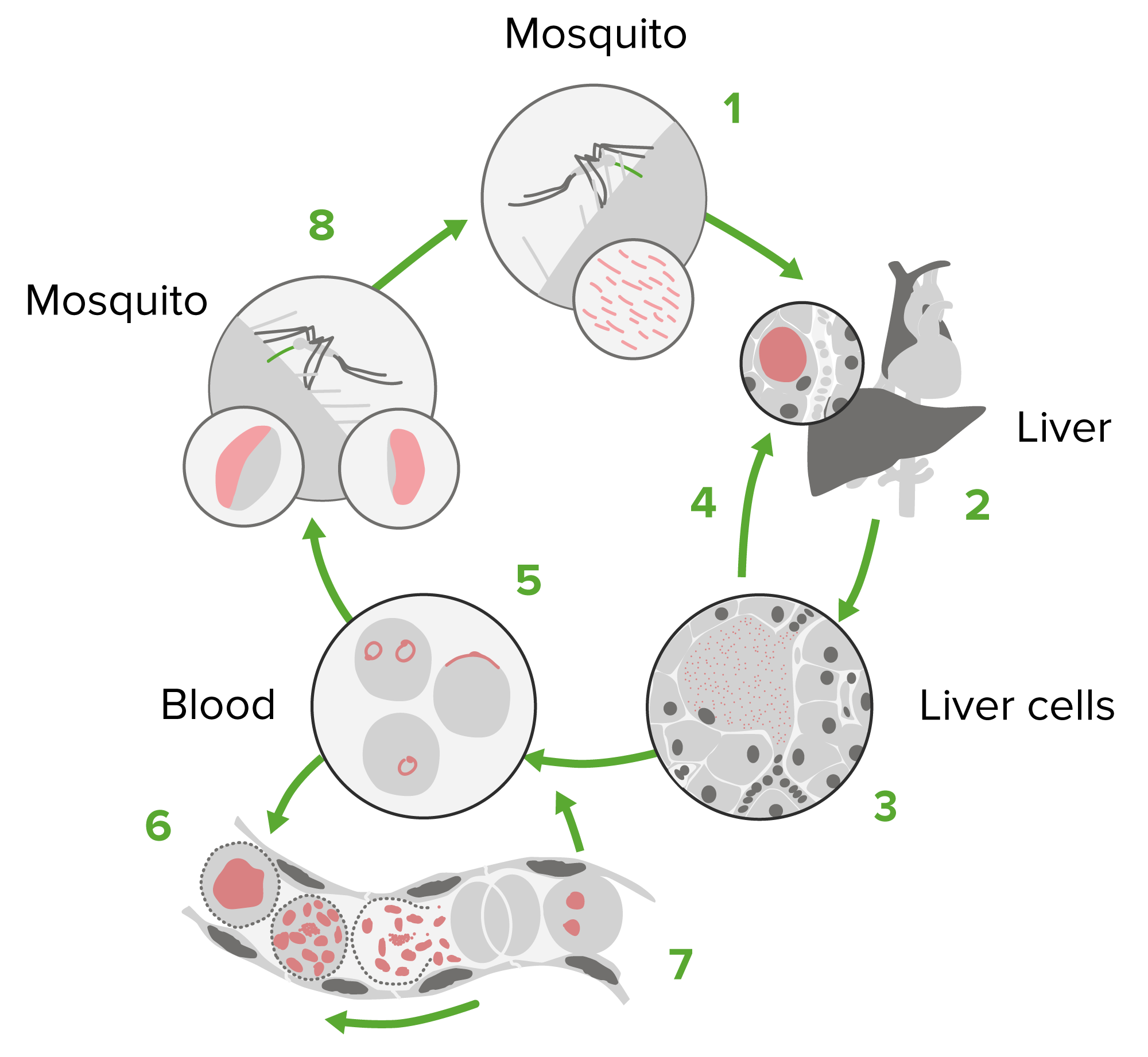
00:00 In this lecture, we're going to discuss malaria. Malaria is a disease that is spread by the Anopheles mosquito. This was largely eliminated from the United States in the early 1950’s. 00:14 It used to go all the way up to as far north as Rhode Islands, but now it's mostly gone. Nonetheless, it is prevalent throughout other countries in the world and is one of the greatest killers of children worldwide especially P. falciparum in Africa. There are more than 100 species of Plasmodium plasmodium that can infect humans, and it is not necessary to remember all these different species but there are a few that are key to understand because they are somewhat different in terms of how they come on. So, P. vivax is clearly different because the liver dormant stage can relapse up to 2 years after the bite. In other words, a patient can have a period of 2 years years when they are relatively asymptomatic before developing symptoms of malaria. P. ovale, that relapse can be even 4 years after the bite. P. falciparum is a major cause of death in sub Southern Africa, and what's key to remember is that there is increased severity to this one, especially in pregnant women. 01:21 The side effect profile is unpleasant at times. 01:26 Likewise, P. malariae has a longer incubation period and is more likely to cause, for example, nephrotic syndrome. So, there are slight differences to these but mostly they’re fairly similar. Let's go to the life cycle of malaria. Basically, the Anopheles mosquito bites the person. The Plasmodium then go as sporozoites down into the liver, and we have the liver stage of the disease. This organism replicates in the liver then and ruptures from the liver into the blood stage of the disease in which the organism is infecting serially red blood cells. Lastly, we have the gametocyte stage which is when now the organism can go back into the next mosquito and be shed to someone else. So, understanding malaria is important and we should understand the incubation period. Typically, the time between being bitten and developing symptoms is 7 to 30 days. Falciparum is often a little bit shorter. A long incubation period can confuse physicians and immigrants and travelers who, the patient is now back, has been home for a period of time and then suddenly develops fever. Just remember this incubation period. 02:48 Now, the patient develops symptoms of uncomplicated malaria. This basically is an attack, a fever, which will typically last 6 to 10 hours and occur every 2 to 3 days. The stages can be named as the cold stage which will last about 15 to 60 minutes when the patient feels cold followed by the hot stage when the patient is overtly febrile between 2 and 6 hours, and then the sweating stage which is 2 to 4 hours after that. This will recur over and over and over again. 03:21 Also, symptoms may include headaches, nausea, vomiting, body aches, and generalized malaise. 03:29 The physical findings can be including fever and perspiration as we’ve discussed but patients may also have weakness, they often have hepatosplenomegaly, they may have jaundice from the increased red blood cell breakdown and they may have tachypnea. Children tend to get tachypnea often with fever. It is sort of like an inflammatory response. More severely, malaria can present with really large problems. One of those is cerebral malaria, which is overtly dangerous. These patients can have altered mental status and be very, very sick. Patients may develop severe anemia and that anemia can be so low they may require transfusions. They may develop hemoglobinuria, a darkening red-brown color to the urine that is obvious to the patient. In severe cases, they can go into ARDS or acute respiratory distress syndrome and may develop frank DIC or disseminated intravascular coagulation. Keep in mind, patients may just go into distributive shock and have hypotension requiring either fluid resuscitation or dopamine, and patients can go into acute renal failure. So, the clinical presentation is different a little bit in that P. vivax and P. ovale typically may present with relapses months or years later because of a persistence of the liver stage. So, these 2 ones can happen years after already returning back from an endemic area. 05:10 Patients with cerebral malaria are at risk for chronic brain problems and we have to keep an eye out for those and don’t forget that chronic or repeated P. malariae may be associated with nephrotic syndrome. So, how do we diagnose malaria? It can be difficult especially in non-endemic areas where we aren’t used to seeing this. I've even seen a handful of cases of children who presented who had never actually traveled out the US but were one of the very rare cases of transmission of the infection between 2 people in a susceptible place where the mosquitoes could spread but this was within the United States. Malaria smear is generally how we start off, and we do something called a thick and thin smear. When you do this, you are looking at a thick area for lots of cells to see if you see any of these malaria organisms and then you do the thin smear to zoom in and see exactly what it looks like, which can help you speciate. So, a malarial smear can show organisms, but it also might be negative. If we are really suspecting it, we sometimes do repeated malarial smears across several days to really prove to ourselves that the patient does not have the disease. But if we see an organism in these red blood cells, as you can see on this slide there is many, then we have made the diagnosis. There is rapid diagnostic testing available but it is still largely experimental. PCR testing is also available but it's only slightly better than the smear so people really haven't jumped to that. Also, in some centers, drug-resistant testing is available because drug-resistant malaria is becoming rapidly a worldwide calamity. So, speaking of drugs, let’s look at all the drugs we have available to us for the treatment of malaria. We have mefloquine, we have atovaquone-proguanil, we have Coartem, we have quinidine, we have quinine, we have chloroquine, and these are all the quinolones. 07:25 Doxycycline can be used sometimes in combination with a quinine, same thing with clindamycin, and there is artesunate, which is not licensed for use in the US although it is available through CDC hotline if you are in a situation where you have a resistant organism and you need that drug. And last, primaquine, which is really for relapse prevention because it is directed mostly against the liver form. So, there are lots of drugs available for this disease. Generally, we would like to prophylax people before they travel to an endemic area. I’d just like to take a moment to plug a website from the CDC for travelers internationally outside of the United States. You go to the CDC website, you can plug in the country and it will tell you what you need to watch out for if you’re traveling to that country. It‘s remarkably useful. In many countries, especially in equatorial areas around the world, we would recommend prophylaxis for people who are traveling to that endemic area. Sometimes, certain prophylaxis is required in certain areas but let’s go to the general prophylaxis regimens. The first is Malarone. Malarone is given daily, it's very well tolerated but we can’t give that for newborns. Another opportunity for a daily prophylaxis is doxycycline. 08:47 Mefloquine is a convenient and easy one or so as chloroquine because these are used weekly, but they are not for use in resistant areas. Chloroquine is useful, again, weekly administration, you need to start 1 to 2 weeks prior to traveling. So, if we see a patient who has malaria, we usually are required to call an infectious disease consult to help us understand what is the best regimen for that patient. The drugs of treatment depend on the location where the parasite was encountered and global resistant patterns. I should point out that the most important thing here is that this killer is potentially going to be curbed in the future through vaccine use. So, there is active vaccine research going on. So far, we haven't had much luck, but we're all keeping our fingers crossed. So, that's a quick review of Malaria in Children. 09:41 Thanks for your time.
About the Lecture
The lecture Malaria in Children by Brian Alverson, MD is from the course Pediatric Infectious Diseases. It contains the following chapters:
- Pathology of Malaria
- Clinical Presentation of Malaria
- Management of Malaria
Included Quiz Questions
What is the test of choice for malaria in the US?
- Thick and thin blood smears
- PCR of blood sample
- ELISA for malaria titers
- CSF malaria PCR
- Blood cultures
Which of the following diseases is spread by the female anopheles mosquito?
- Malaria
- Lyme disease
- Sleeping sickness
- Plague
- Scarlet fever
Which of the following is NOT a complication of malaria?
- Conjunctivitis
- DIC
- Hemoglobinuria
- ARDS
- Acute renal failure
Which of the following is NOT a common symptom seen with malaria?
- Sandpaper rash
- Fever
- Hepatosplenomegaly
- Jaundice
- Tachypnea with fever
Pregnant women particularly susceptible to which of the following species of plasmodium?
- Plasmodium falciparum
- Plasmodium knowlesi
- Plasmodium vivax
- Plasmodium ovale
- Plasmodium malariae
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I particularly liked the part about treatment in children and contraindications.