Playlist
Show Playlist
Hide Playlist
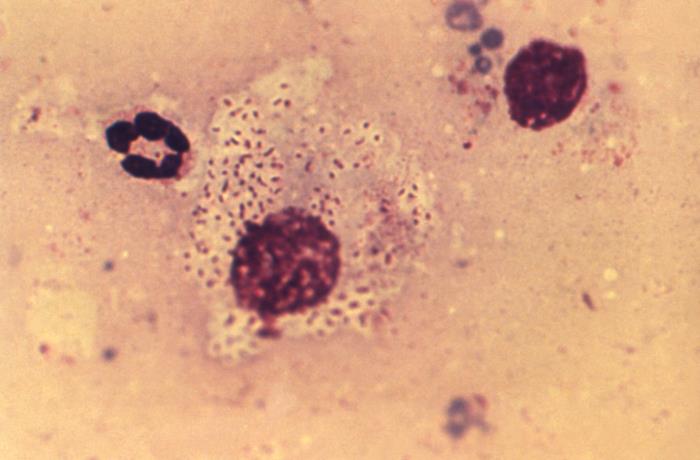
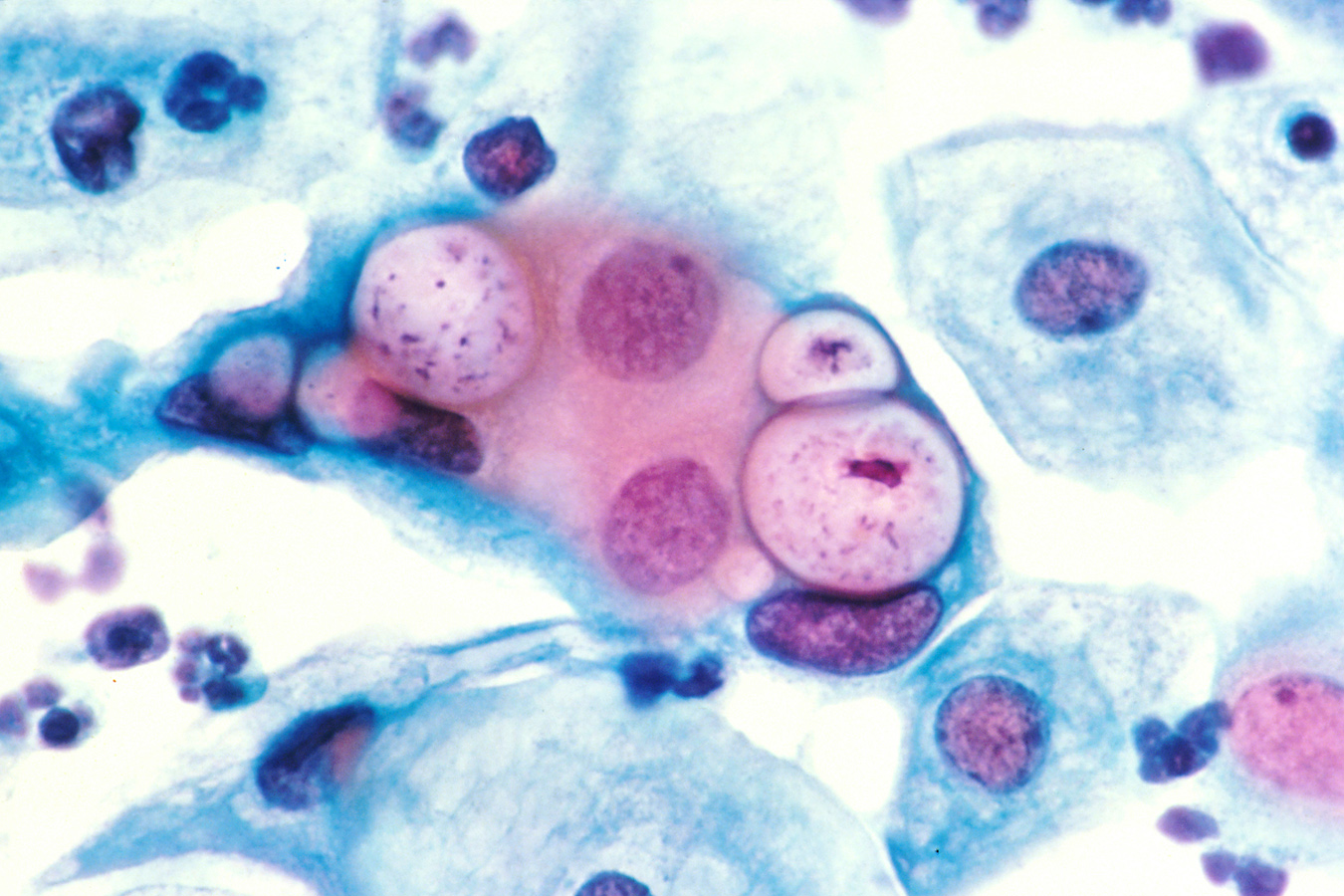
Lymphogranuloma Venereum (LGV): Signs/Symptoms, Diagnosis & Management
-
Slides LymphogranulomaVenereum InfectiousDiseases.pdf
-
Reference List Infectious Diseases.pdf
-
Download Lecture Overview
00:01 Generally, LGV as we call it, is divided and classified according to stages – stage 1 through 3. 00:14 Stage 1 has an incubation period of from 3 to 30 days after contact with the infected individual. 00:24 The patient develops a primary lesion, which is a papule on the genital mucosa somewhere. 00:32 Usually, the patient doesn’t even recognize or have any recollection of ever having had such a lesion. 00:41 It’s generally on the external genitalia or vagina and, emphasized, usually asymptomatic. 00:49 And being asymptomatic, it’s going to heal rapidly and without any scar. 00:54 But the story has not been completely told because now we enter stage 2 because these organisms have a proclivity to spread to the regional lymph nodes. 01:08 Days to weeks after this primary lesion develops, the patient gets a very impressive lymphadenopathy. 01:20 In men, that would be the inguinal area, which drains the penile area. 01:26 In women, 20 to 30 percent of the time, it’s the inguinal nodes, but occasionally it’s the iliac and obturator nodes in the pelvis, which drain the upper vagina and cervix. 01:41 The patient may have a systemic illness along with this – with fever, headache, myalgias, and backache is common in women from inflamed pelvic nodes. 01:57 So anyway, you start out with tender nodes. 02:01 The nodes swell up into an inflammatory mass, and then the nodes abscess. 02:09 And sometimes, they will coalesce these abscesses and produce something that many people would call bubo, which is essentially a swollen node with pus in it, and this bubo may spontaneously rupture. 02:29 The result may be a loculated abscess, fistulous tracts, and sinus tracts, and the classic manifestation is what we call the “groove sign”. 02:45 There’s nothing to the groove sign except that you have swollen lymph nodes above the inguinal ligament and swollen lymph nodes below the inguinal ligament. 02:56 And so, it makes the inguinal region looks like it has a groove from swollen nodes on either side Stage 2 can also be manifested, especially with men who have sex with men, or in women who permit anal intercourse, a granuloma that’s inflammation of the bowel wall with strictures, rectovaginal fistulas, perirectal abscesses, and anal fistulas. 03:23 One thing to remind the learner about is that Crohn’s disease can look pretty much like this. 03:32 So I think you could see why anyone who has Crohn’s disease, very careful history about sexual practices should be undertaken because LGV can mimic Crohn’s disease, and, of course, the treatment would be drastically different for the two diseases. 03:52 This is not very common, but at least a good physician should think about this. 03:59 And then stage 3, and I will have to admit that I have not seen patients with this form. 04:08 But untreated, patients can get tremendous blockage of lymphatics – because remember, this is a lymphatic disease. 04:18 And with blockage of the lymphatics, you get something like elephantiasis of the genital area, and that resembles the parasitic form of elephantiasis, which happens to the extremities. 04:35 And I also have not seen esthiomene, which comes from the Greek meaning “eating away”. 04:43 But what esthiomene is, it’s a hypertrophic, granulomatous enlargement of the genital area, and on top of that, ulcers. 04:53 The external genitalia are involved, and this includes the vulva, the scrotum, and the penis -- very disfiguring and very troubling. 05:02 So how do we make the diagnosis? Well, it would be definite if we have a positive nucleic acid amplification test for one of the serovars of Chlamydia trachomatis. 05:19 And you can get this from a vaginal swab, you can get it in men from a first-catch urine, rectal swab, or a rectal lymph node culture. 05:33 It would be considered probable if you don’t have proof from nucleic acid amplification test, but you have a classic clinical picture of lymphogranuloma venereum. 05:48 As far as the management of this condition, the drug of choice for Chlamydia trachomatis is doxycycline for 21 days. 06:00 If you remember, this is a slow process – slow to grow and slow to die. 06:07 So we generally treat this for 21 days. 06:10 That should cause rapid resolution of the systemic complaints, but it may not have that much effect on the resolution of these swollen fluctuant nodes. 06:24 You actually may need to have incision and drainage of those. 06:30 Alternative treatment includes erythromycin or azithromycin, or the fluoroquinolone levofloxacin, and obviously, examination and treatment of sexual partners. 06:43 This concludes my discussion of lymphogranuloma venereum.
About the Lecture
The lecture Lymphogranuloma Venereum (LGV): Signs/Symptoms, Diagnosis & Management by John Fisher, MD is from the course Genital and Sexually Transmitted Infections. It contains the following chapters:
- Lymphogranuloma Venereum – Signs/Symptoms
- Clinical Stage 2
- Clinical Stage 3
- Lymphogranuloma Venereum – Diagnosis
- Lymphogranuloma Venereum – Management
Included Quiz Questions
The classic “groove sign” caused by inflammation of superficial and deep inguinal lymph nodes is characteristic of infection with which of the following pathogens?
- Chlamydia trachomatis
- Treponema pallidum
- Klebsiella granulomatis
- Herpes simplex virus
- Haemophilus ducreyi
What is the approximate incubation period for Chlamydia trachomatis causing lymphogranuloma venereum?
- 3 - 30 days
- 3 months
- 1-3 days
- 3-6 months
- More than 6 months
Genital elephantiasis is observed in which stage of lymphogranuloma venereum?
- Stage 3
- Stage 2
- Stage 0
- Stage 1
- None of the above
Which of the following lymph nodes is most commonly involved in women with lymphogranuloma venereum? Select all that apply
- Iliac
- Hilar
- Periaortic
- Axillary
- Inguinal
What is the most appropriate antibiotic treatment for lymphogranuloma venereum proctocolitis?
- Three weeks of oral doxycycline
- A single dose of ceftriaxone
- A single dose of azithromycin
- Ten days of levofloxacin
- Antibiotic therapy is not indicated in lymphogranuloma venereum proctocolitis.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |