Playlist
Show Playlist
Hide Playlist
Leukemia Cutis: Pathophysiology
-
Reference List Pathology.pdf
-
Slides Leukemia Cutis Pathophysiology.pdf
-
Download Lecture Overview
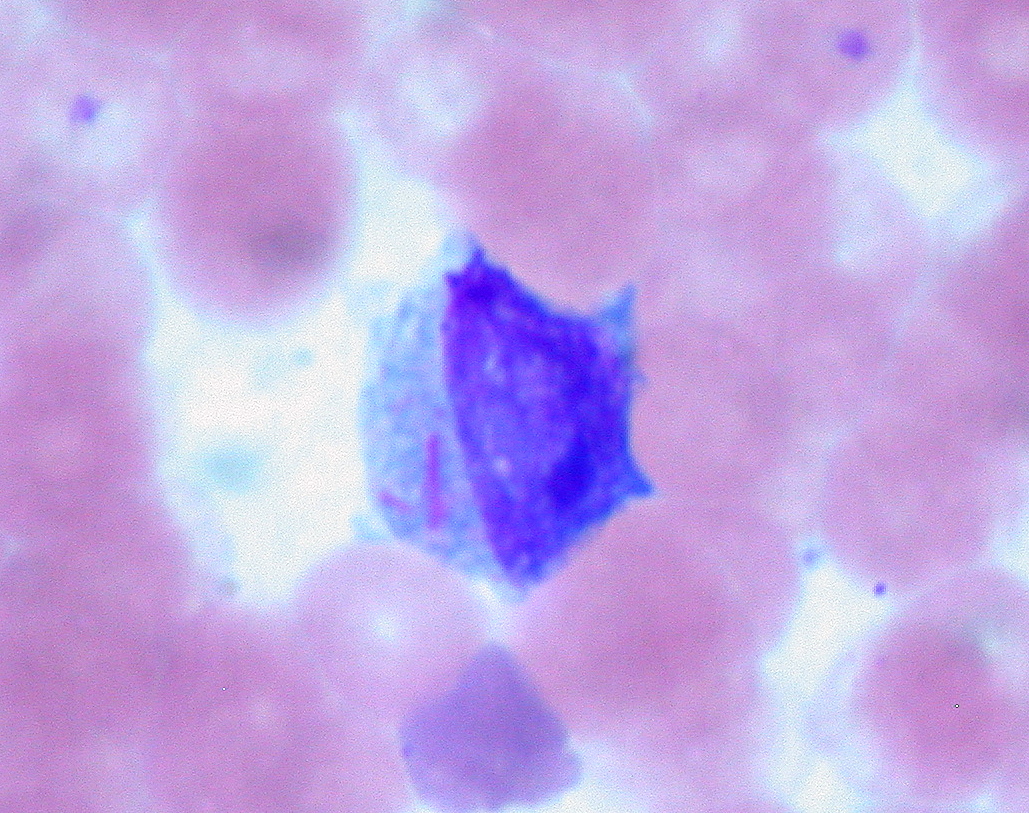
00:01 Welcome. In this talk, we're going to look at a cutaneous manifestation of a systemic disease that is to say leukemia. 00:08 So a malignant accumulation of white blood cells derived from the marrow. Leukemia cutis, as I just said, is involvement of the skin by leukemic infiltrates. 00:20 The epidemiology is that it's fairly uncommon. 00:24 About 3% of leukemic patients will have the cutaneous manifestation. And virtually every case, this is not how we make the diagnosis, but rather we knew they had leukemia and now they also have skin lesions. There are higher risk in the pediatric leukemias. 00:46 But and most common in the adult population is going to be AML and CLL, so acute myelogenous leukemia and chronic lymphocytic leukemia. 00:55 So with regard to the pathophysiology of leukemia I'm not going to go into that. 00:59 I would refer you to excellent talks that are in the Hematopathology section of the Lecturio lectures. Suffice it to say that there are genetic and environmental risk factors for leukemia not otherwise specified. And it's really additional changes that make us have leukemia cutis. It's not a special form of leukemia. 01:23 It is just a leukemia that also happens to have the ability to go to skin. So there are known genetic abnormalities in leukemia. 01:31 There are various environmental risk factors benzene and ionizing radiation, certain viral infections, etc.. 01:38 But now why do they go to the skin? And that's because in a subset of patients, like 3%, the leukemic cells have developed additional kind of mutations or expression of genes that give them a tropism for the skin vasculature. They like to go to the skin vessels, and there may be a unique expression of certain integrins or adhesion molecules. There may be certain expression of chemokines or their receptors that are mediating why the leukemic cells migrate to the skin. 02:13 It can present in a variety of ways. 02:16 So papules or nodules, you typically get enough of an infiltrated leukemic cells to actually be able to feel them on the surface, they may be substantially large. 02:25 So you get plaques. It's rare that you get a lot of inflammation associated with them, but they can be any color. 02:33 These papules and nodules red, brown, yellow, blue depending on the vasculature, depending on the nature of the granules within the individual leukemic cells, those sorts of things. 02:46 Pretty much every part of the body is affected relatively equally, and you may get oral mucosal gingival hyperplasia with accumulation of leukemic cells within the oral mucosa. 03:00 The diagnosis it's a physical exam but really it's more of they have leukemia. Or we can prove they have leukemia through complete blood count, peripheral smear, bone marrow biopsy, et cetera and then we can do a biopsy to rule out other things and demonstrate the leukemic infiltrates on the biopsy. We can do histopathology, demonstrating all kinds of leukemic cells. And on that, we can also specifically do immunophenotyping to see what kind of leukemic cells if there's anything uniquely interesting about them. 03:34 Specific cytogenetics, flow cytometry, and other studies in general, those will have already been done on peripheral blood or on bone marrow, so we wouldn't really do it again on skin biopsy. 03:46 And we would just focus on the histopathology demonstrating leukemic infiltrate. 03:50 How do we manage this? Well, in fact we need to treat the leukemia. 03:53 So you would do the typical aggressive systemic chemotherapy targeting that. You can also do radiation. 04:01 Um, if if the lesions on the skin are particularly otherwise difficult to treat. What you can't really do is say puva therapy. So you wouldn't do kind of topical antineoplastic drugs followed by ultraviolet radiation. 04:17 Yeah. You might transiently kill the population of cells, but you would they would just going to they would just come back from the bone marrow and repopulate the skin. So it's really you need to go after the primary leukemia. With that we've discussed leukemia cutis, an interesting but overall kind of rare manifestation of systemic leukemia.
About the Lecture
The lecture Leukemia Cutis: Pathophysiology by Richard Mitchell, MD, PhD is from the course Tumors of Cutaneous Lymphoid Cells.
Included Quiz Questions
What percentage of leukemia patients typically develop leukemia cutis?
- Approximately 3%
- Approximately 15%
- Approximately 25%
- Approximately 40%
- Approximately 50%
What mechanism explains the specific targeting of leukemic cells to the skin in leukemia cutis?
- Expression of specific integrins and chemokine receptors with skin tropism
- Direct invasion of leukemic blasts from bone marrow into dermal tissues
- Random distribution and nonspecific accumulation of circulating leukemic cells
- Transformation of resident epidermal and dermal cells into malignant phenotypes
- Secondary infection and inflammatory response within cutaneous tissue layers
Which oral manifestation is commonly associated with leukemia cutis?
- Gingival hyperplasia
- Tongue ulceration
- Palatal erosions
- Tooth decay
- Lip fissures
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |