Playlist
Show Playlist
Hide Playlist
Leiomyoma vs. Leiomyosarcoma
-
Slides Uterus Female Repro.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
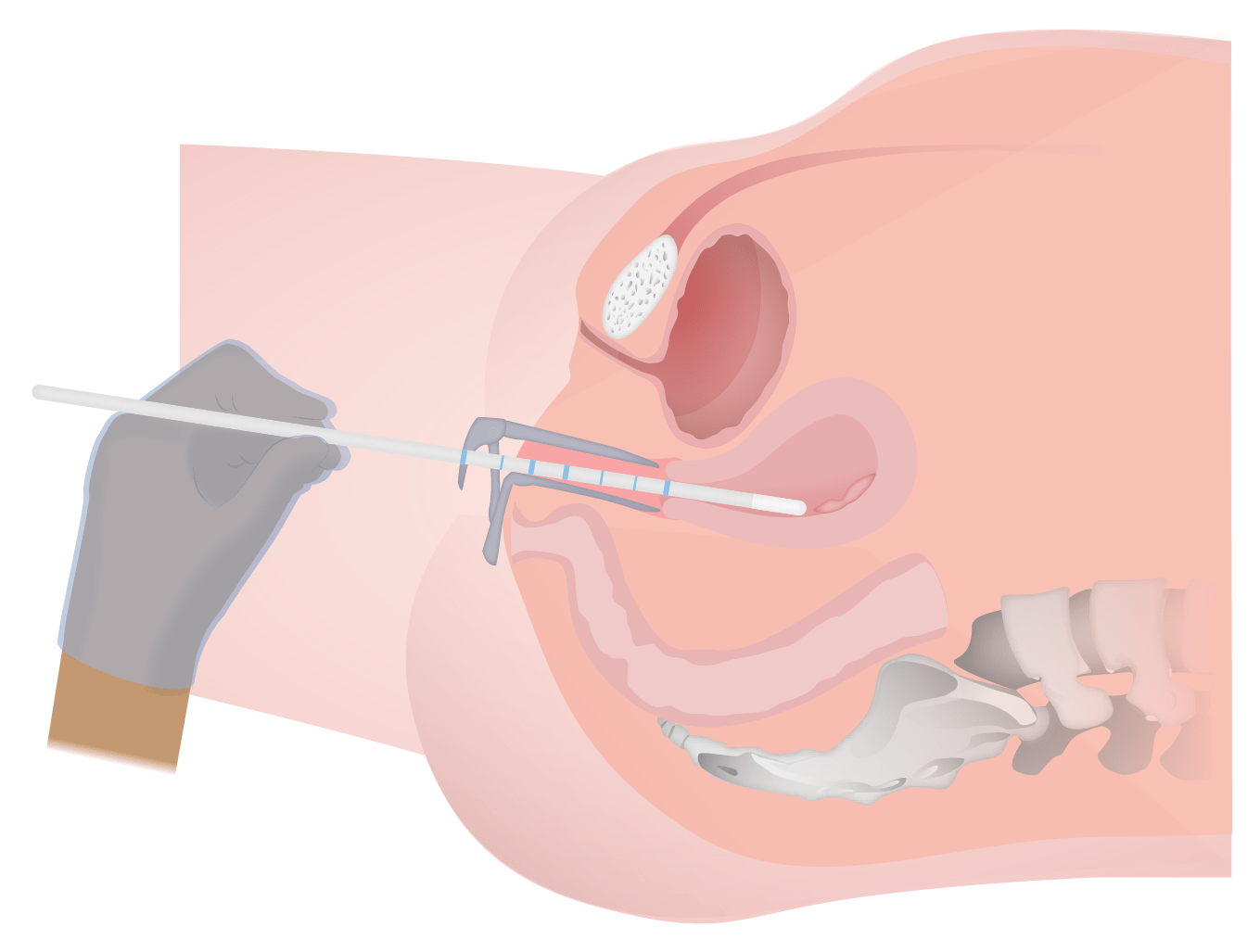
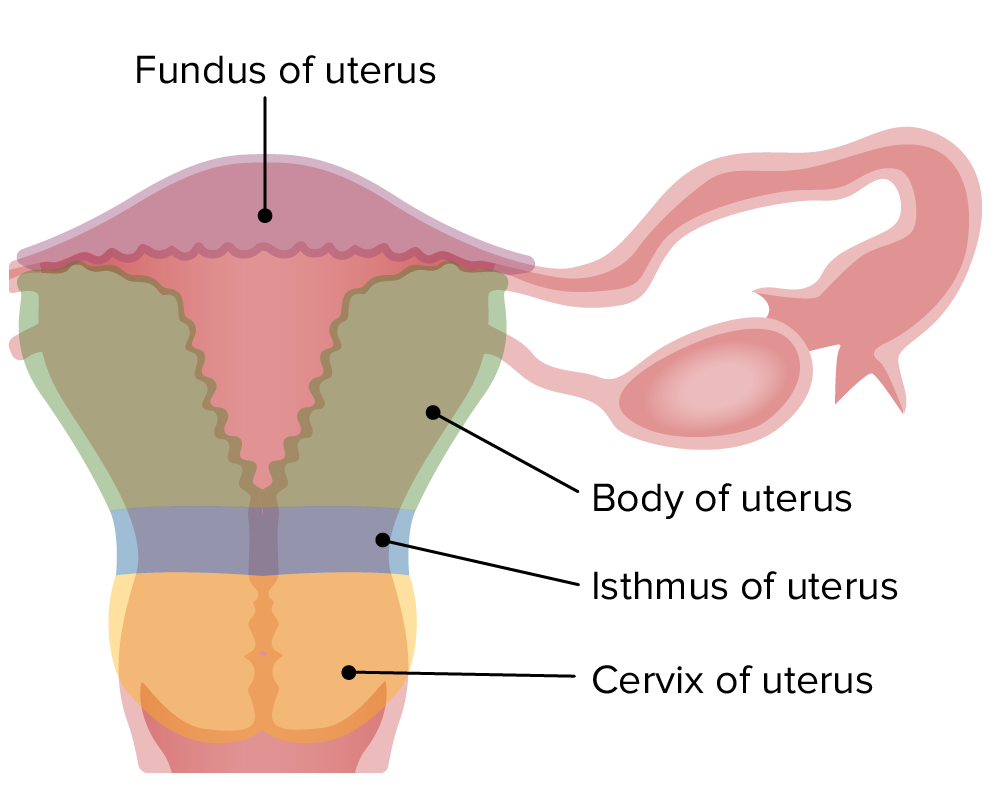
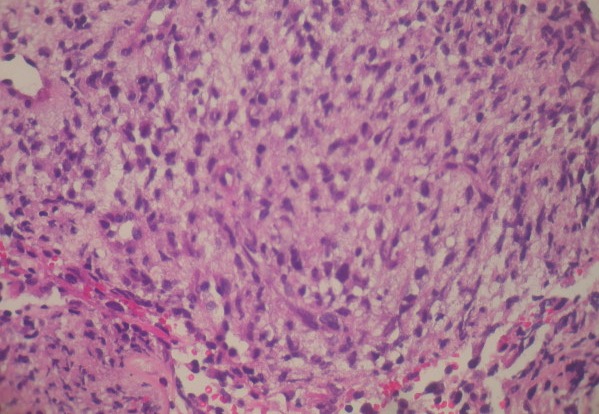
00:01 Another benign condition, apart from the endometrial polyp, would be something called a leiomyoma. 00:08 A leiomyoma is a smooth muscle tumor that is of absolutely benign nature that occurs in a reproductive age of a female, usually young African American, but very much could be a Caucasian lady as well. 00:20 The most common tumor in women is estrogen responsive. 00:24 What does that mean to you? It means that every time that she’s having her menstrual cycle and/or she is pregnant. 00:32 And if she’s pregnant, there’s obviously increased estrogen and you’ll find the size of the tumor that then increases. 00:38 That becomes important. 00:40 Leiomyoma, a fibroid. 00:42 It presents with abnormal bleeding and what may then happen with the fibroid is the fact that it might then cause compression of the adjacent structures. 00:50 You want to keep in mind, bladder and may result in infertility, which is unfortunate for a young lady. 00:57 A leiomyoma. 00:59 There are different locations of leiomyoma. 01:01 You can have something called pedunculated and that would be on the superficial side, pedunculated. 01:06 Or you could have one that’s subserosal, meaning to say right underneath the serosa of your uterus. 01:13 You can have one that is intramural, meaning the wall. 01:17 And you can have ones that are submucosal. 01:21 Leiomyoma. 01:23 Look at this. 01:24 Well circumscribed, white tumor, bulging into endometrial cavity. 01:30 That’s what this looks like with the leiomyoma. 01:36 Next topic is the leiomyosarcoma. 01:38 What does this mean to you? This did not come from leiomyoma. 01:43 It arose, as you shall see, de novo. 01:47 For the most part, as far as you’re concerned, it never comes from a leiomyoma. 01:51 It’s a malignant tumor of smooth muscle that will then invade the uterine wall. 01:56 Arises de novo. 01:57 What does that mean? It did not come from leiomyoma. 02:01 It started of its own. 02:04 Clinical features here, the peak incidence will be between 40 to 60 years of age. 02:11 Leiomyoma versus a leiomyosarcoma. 02:14 On your left, you end up finding a picture in which it’s well-encapsulated and well-differentiated. 02:19 Where on the right you end up finding leiomyosarcoma, where it’s completely increased proliferation and you cannot make out a darn thing. 02:28 Remember please that one leiomyoma did not give rise to leiomyosarcoma. 02:33 Leiomyosarcoma obviously is the malignant smooth muscle tumor that will then invade the leiomyoma. 02:40 Let me repeat once again, you can have that’s pedunculated or it should be in the surface of the uterus. 02:46 You can have one that is subserosal, which is just underneath the serosa. 02:50 You can have one that’s in the mall – wall, excuse me, that is called intramural and then you can have one that’s submucosal, meaning to say it’s closer to the uterine cavity. 03:00 Different locations of leiomyoma: From the surface of the uterus, all the way through the wall and into the cavity. 03:07 Leiomyoma is definitely something that you very much need to know, a very common cause in a young lady who is going to be suffering from dysfunctional uterine bleeding and lots of pain, lots of pain. 03:18 Well-encapsulated.
About the Lecture
The lecture Leiomyoma vs. Leiomyosarcoma by Carlo Raj, MD is from the course Uterine and Fallopian Tube Disease.
Included Quiz Questions
Which statement about leiomyomas is NOT true?
- It has a high potential for malignant transformation.
- It is a benign tumor.
- It is estrogen responsive.
- It is a tumor of smooth muscle of the uterus.
- The size and location of the tumor within the myometrium are variable.
Which of the following can be a presenting complaint if a woman has a small fibroid located right underneath the peritoneum covering the fundus of the uterus?
- Compression of the urinary bladder leading to increased frequency of urination
- Compression of the rectum leading to constipation and hemorrhoids
- Severe, recurrent pelvic pain
- Compression of the fallopian tube opening leading to ectopic pregnancy
- Compression of uterine arteries leading to myometrial ischemia
What is the relationship between leiomyoma and estrogen levels?
- Leiomyoma increases in size when there is a high level of estrogen (e.g. in pregnancy) and decreases in size after menopause.
- Leiomyoma transforms into leiomyosarcoma when the amount of estrogen in the bloodstream increases.
- Leiomyoma can form only when there is very high level of estrogen in the bloodstream (e.g. with an estrogen-secreting ovarian tumor).
- High levels of estrogen can cause involution of leiomyoma.
- Low levels of estrogen cause increase in the size of leiomyoma, whereas high levels produce the opposite effect.
What are the main differences in the gross and microscopic appearance of leiomyoma and leiomyosarcoma?
- Leiomyomas are well-circumscribed grossly and well-differentiated microscopically, whereas leiomyosarcomas are the opposite in both respects.
- Leiomyomas are small grossly and have fewer smooth muscle cells; a leiomyosarcoma is huge and consequently has many tightly packed smooth muscle cells.
- Leiomyomas occur only right below the endometrium, whereas leiomyosarcomas occur under the peritoneal lining, but microscopically they are the same.
- Leiomyomas are white grossly and are microscopically composed of white smooth muscle cells with abundant collagen stroma. Leimyosarcomas are red grossly and have many blood vessels microscopically.
- Leiomyomas and leiomyosarcomas cannot be differentiated on microscopy. Special staining techniques and electron microscopy are required for diagnosis.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I like that the video was short and high yield. Thank you :)