Playlist
Show Playlist
Hide Playlist
Left-sided and Right-sided Heart Failure
-
Slides Heart Failure.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
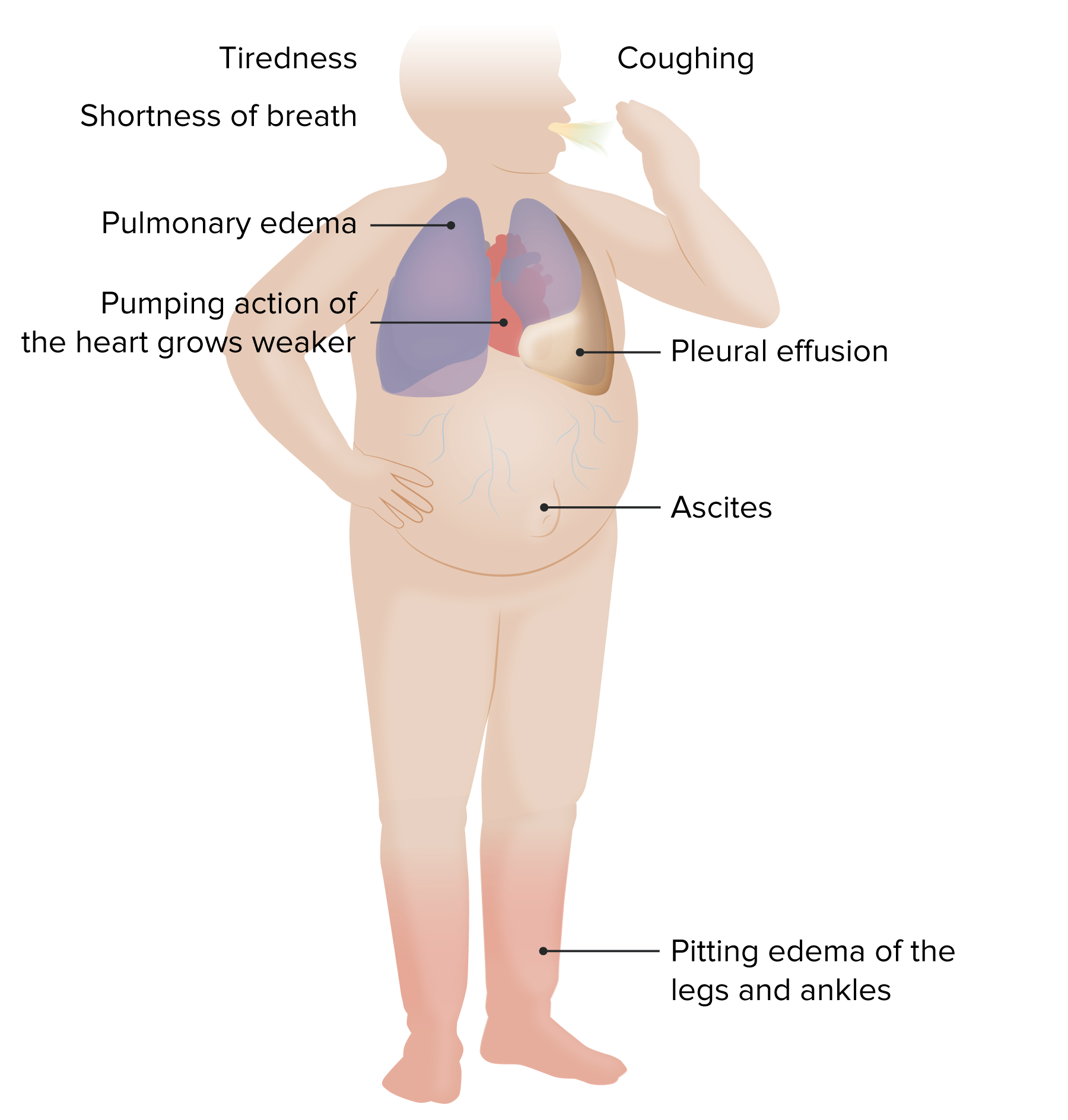
00:00 为了 正确谈论心力衰竭, 我们首先必须了解一些 正常的心脏功能。 这里的想法不一定是 给你所有的细微差别。 这就是你未来从事心脏病学事业的目的。 而是要掌握 基本的基本概念 我们将从心腔和瓣膜的粗略视图开始。 图像左侧为蓝色 以反映右心室的缺氧血液 。 血液从身体返回 到右心房, 通过三尖瓣 进入右心室 并从肺动脉瓣流出 到达肺部。 图像右侧呈粉红色 以反映左心室的含氧血液 。 血液从肺部通过 肺静脉返回到左心房。 通过二尖瓣 进入左心室。 然后从主动脉进入身体。 好的,现在让我们开始吧。 当心房收缩时,血液 被推过三尖瓣 和二尖瓣,以填充心室,心室正在放松 以便它们能够填充和容纳 进入的血液。 一旦心室最大程度地充满, 它们就会收缩 以将其内容物推出。 二尖瓣的三尖瓣关闭, 因此没有反流回流 而肺动脉瓣 和主动脉瓣被心室压力激增 强行打开。 这是一件美妙的事情 发生的频率大约为 每分钟收缩 60 到 80 次或更多, 这意味着在一年内收缩超过 4000 万次 平均而言 一生中收缩 25 亿次。 每次收缩大约挤出 50 cc 血液, 普通人的心脏在其一生中将泵出约 100 万桶血液 或足以填满三艘超级油轮。 让我们在这里惊叹一下。 好的,就说这么多。 现在让我们讨论一下收缩的阶段 这样我们就可以更好地理解一些心力衰竭的模式。 心室挤压阶段 称为收缩期。 心室扩张充盈阶段称为舒张期。 充盈高峰时心室内的血量称为舒张末期容积 而收缩期结束时心室内剩余的血量 称为收缩末期容积。 值得注意的是, 心脏不会在任何一次收缩中挤出其全部 舒张末期容积 。 收缩期间排出的量称为 射血分数或 E-f。 该容量通常介于舒张末期容量的 50 至 75% 之间 因为心脏总是在心室内留有少量储备血液 每次正常收缩后 收缩期收缩是一个重要点 因为它为身体提供了一种潜在地提高心输出量的方法 通过一种机制 而不仅仅是增加心率。 即通过更有力地挤压 而射血分数的正常范围为 50% 至 75%。 如果 40% 到 50% 被认为是 灌注 外周器官的临界值,如果低于 40% 通常是不够的。 因此 这导致心力衰竭 其定义为心脏无法泵出足够的血液 来满足身体的需求。 这通常也被称为 充血性心力衰竭 或 CHF 因为随着前向流量减少, 血液回流到 衰竭心室后面的组织中。 左心衰竭时,血容量 和压力会回流到肺部, 导致肺水肿和呼吸困难 或气短 右心衰竭时, 血液会回流到外周 组织,导致全身水肿。 有一条真理是,右心衰竭最常见的原因是左心衰竭,导致右侧压力和容量超负荷。 话虽如此,有些疾病,如肺动脉高压,会导致 单独的右心衰竭,而没有任何左心室衰竭。 好的,现在你 还需要知道并非所有的心力衰竭都是一样的。 也许最容易理解的 是真心实意的治疗 降低射血分数 或减半参考值。 如果心脏受损,比如心肌梗塞, 如右图所示, 能够挤压血液的肌肉质量会减少 射血分数会下降。 简而言之,就是系统功能障碍。 虽然现在人们更喜欢用 F Rev 来表达, 导致半数心力衰竭的最常见原因 射血分数降低 是缺血性心脏病。 但另一个重要原因是扩张型心肌病 遗传、毒性或传染病。 总体而言,二尖瓣关闭不全通常是 心力衰竭的次要后果 射血分数降低 因为左心室扩张 试图增加心输出量。 这样一来,系绳会打开瓣膜 并阻止其关闭。 这枚硬币的另一面就是心力衰竭。 射血分数保留 或 PEMF 减半。 在这种情况下,您可以认为 心脏变得僵硬 这是由于间质纤维化 或其他沉积物 这将阻止舒张期间完全充盈。 我们试图用这些间质沉积物来表示 心室壁看起来很奇怪, 即使心脏收缩可能相对正常。 毕竟,它的射血分数是保留的。 它不能很好地放松和填充。 结果是心输出量减少。 同样,一种简写方式是舒张功能障碍, 尽管我的心脏病学同事 向我保证,最好的说法是 这是半 PEMF 心力衰竭 ,射血分数保留。 各种损伤 都可能导致半 PEMF。 其中许多与间质纤维化增加有关。 这些包括衰老、高血压、 主动脉瓣狭窄和糖尿病。 心脏淀粉样蛋白沉积是另一种经典的 导致心力衰竭 射血分数保留的方式。 因此,总结一下, 心力衰竭是一种血液泵入不足的疾病 无法维持外周组织的需求。 它并不总是与射血分数降低有关。 舒张不足和舒张充盈不足也可能是原因。 左心衰竭的症状总体上是咳嗽。这是因为水 积聚在肺泡内,感觉就像溺水一样,所以你会咳嗽,并且会呼吸困难,因为你得不到足够的氧气 当肺泡一半充满水而不是空气时。这实际上没有区别 无论是舒张功能障碍还是收缩功能障碍。这些将是患者要报告的主要 体征或症状。对于 慢性疾病,我们可能 进展超出此范围。因此,他们将出现端坐呼吸。他们将 重新分布 外周水肿,特别是在右心衰竭中。 这将导致液体 当他们仰卧时,这些液体会积聚在肺部。 患者还可能出现 阵发性夜间呼吸困难,睡眠期间外周 水肿导致液体大量重新分布,从而引发严重的呼吸短促症状。患者会 描述他们醒来后,气喘吁吁,不得不 走到窗前, 打开窗户。这就是阵发性夜间呼吸困难或静息呼吸困难。所以这些都是心力衰竭的迹象 。收缩功能障碍或舒张功能障碍,几乎都是 重叠。因此,您可能会出现呼吸困难、烦躁,也就是心律失常。 由于大脑灌注不足,您可能会注意力不集中。 由于肾脏灌注不足,您可能会出现肾功能不全。 由于肾素血管紧张素 醛固酮系统的激活,您将出现 水肿。因此,就右心衰竭而言,正如我已经提到的,左心 心脏病是最常见的原因,但也有其他原因导致原发性孤立性 右心衰竭,其中包括原发性肺部疾病, 因此要么是肺纤维化 要么是原发性肺动脉高压,甚至严重的肺气肿。 由于肺部血流受限,右心室承受更大的压力,负荷过大,随着时间的推移,右心室可能会衰竭。由于原发性肺部过程导致的右心衰竭称为肺心病。Cor 表示心脏,pulmonale 表示肺。您还可能出现复发性肺栓塞。因此,这还不足以杀死你 但反复发作的低水平 血栓形成通常来自腿部深静脉进入 肺部,可以再次阻塞 肺循环并导致肺动脉压力升高,从而导致右心室衰竭 另一个重要原因是,特别是现在肥胖症的流行,阻塞性睡眠呼吸暂停是一种在世界各地,特别是发达国家普遍存在的疾病,它不仅会导致打鼾,还会在睡眠期间造成相对缺氧。所有这些肥胖的组织都会压迫上呼吸道,可能会导致肺部供氧不足。肺部处理任何特定部位的氧合减少的方式是减少该区域的血液供应。 如果你的某个局部区域没有得到良好的氧合,你就不会想把血液送到那里。 但是,如果整个肺部得不到良好的供氧,现在我们将 挤压肺血管系统的所有血管,我们将 由于慢性复发性夜间阻塞性睡眠呼吸暂停,导致右侧心力衰竭。
About the Lecture
The lecture Left-sided and Right-sided Heart Failure by Richard Mitchell, MD, PhD is from the course Heart Failure.
Included Quiz Questions
What causes edema on physical examination in a patient with heart failure?
- Renin-angiotensin-aldosterone system activation
- Hypoxic encephalopathy
- Increased renal perfusion
- Increased cerebral perfusion
- Neurohumoral inactivation
What is the MAIN symptom patients have with both systolic and diastolic heart failure?
- Dyspnea
- Irritability
- Edema
- Renal insufficiency
- Cough
Which of the following is a cause of right-sided heart failure more so than left-sided heart failure?
- Pulmonary hypertension
- Systemic hypertension
- Anterior wall myocardial infarction
- Anemia
- Hyperthyroidism
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
It is very nice lecture Ilike your way of teatching ??