Playlist
Show Playlist
Hide Playlist
Large Bowel Obstruction (LBO – Emergency Medicine)
-
Emergency Medicine Bord Bowel Obstruction.pdf
-
Download Lecture Overview
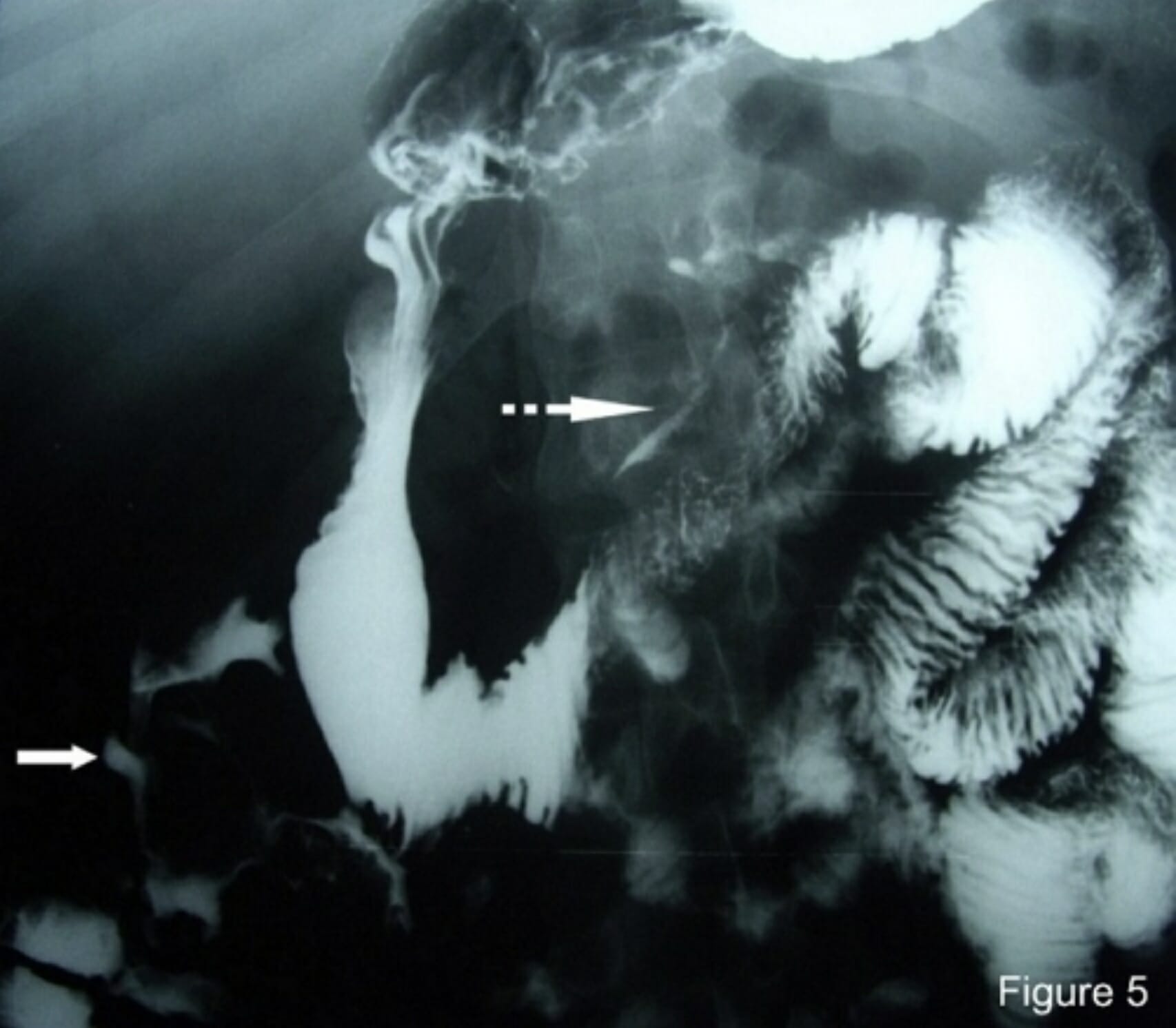
00:01 Now we’re gonna move on and we’re gonna talk about large bowel obstruction. 00:05 Large bowel obstruction is by far less common than small bowel obstruction. 00:10 A majority of it is due to colon cancer, so 50% of patients who have a large bowel obstruction will have associated colon cancer. 00:18 And 20% of patients with colon cancer will go on and get a large bowel obstruction. 00:24 So these two things do sometimes go hand-in-hand. 00:27 So when you’re diagnosing or thinking about a large bowel obstruction, definitely, you wanna make sure that you're thinking about concomitant or associated malignancy. 00:36 Why does this happens? Cancer is by far the most common cause but there’s other reasons that patients can have a large bowel obstruction. 00:47 One of them is a volvulus, possible diverticular disease or someone has severe diverticulosis that can cause an obstruction. 00:56 Strictures, mostly due to inflammatory bowel disease. 00:59 Patients with ulcerative colitis or Crohn’s can get strictures of the bowel wall due to recurrent inflammation in those areas. 01:08 And they can get blockages related to that. 01:11 Adhesions may also play a role here. 01:13 So prior surgeries which can predispose patient’s to adhesions. 01:17 So if you’ve ever had a surgery on your abdomen, you're predisposed to scar tissue there. 01:22 And then hernias, as well. 01:24 Now there is something called pseudo-obstruction and this is also known as Ogilvie’s syndrome. 01:31 This is when there is evidence of large bowel obstruction but there’s no obstructing lesion that can be found. 01:38 Patients who have Ogilvie’s oftentimes have lots of other medical problems. 01:43 Significant co-morbid conditions and is thought to be due to malfunction of the autonomic control of the bowels. 01:50 So the bowel just isn't moving around because something’s messed up with the autonomic control. 01:55 Normally, the autonomic system tells us to have peristalsis and to move things along in our intestines, but here, for whatever reason, it’s just not working appropriately. 02:06 So what's our physiology component here? So the bowel, basically, if there’s an obstruction can get dilated which can lead to increase pressure within the lumen of the bowel and that can leads to compromise blood flow to the bowel wall and whenever you have compromised blood flow to the bowel wall you can get swelling, and fluid into the lumen of the bowel. 02:28 What then in turn happens is that the arterial blood flow can lead to ischemia and gangrene and eventually perforation. 02:36 And these patients can potentially get very, very sick. 02:39 Similar thing can happen with small bowel obstruction as well, so it’s important to keep that in mind for both of those conditions. 02:47 What a patient present with? Very similar to things that patient’s with small bowel obstruction present with. 02:54 Abdominal pain, vomiting, obstipation—they’re not able to go to have a bowel movement, potentially, they may not be passing gas. 03:03 Fever may be present especially in the situation of perforation or rupture. 03:08 Symptoms may develop rapidly. 03:11 In the situation of a volvulus, that’s something that happens very acutely. 03:14 They also may happen gradually though. 03:17 So if it’s due to a malignancy, those symptoms may be gradually developing over a period of time. 03:23 Other things potentially to talk with your patient about would be symptoms that are associated with malignancy. 03:29 Have you had any weight loss? Have you had been very fatigued? Have you seen any blood in your stool? All of those things are associated with colon cancer. 03:37 So asking patients about that information as well, may be helpful. 03:42 On your physical exam, the belly may be distended. 03:47 So it may look bigger. 03:48 I sometimes will have to ask patient’s—does your abdomen look more swollen than it normally does? If people have a protuberant abdomen. 03:56 Diminished bowel sounds. 03:58 On the physical exam, you wanna go ahead and listen to the abdomen. 04:02 Listen for approximately 2 minutes to hear if you hear anything. 04:06 Vitals are vital. 04:08 Vital signs may reveal fever or an elevated heart rate. 04:11 Definitely hypotension, or a low blood pressure in situations of severe infection. 04:17 You may feel a palpable abdominal mass in situations where cancer is very advanced, and it’s also important to do a rectal examination to feel if you feel any masses, see if there’s any blood in the stool. 04:30 How do we diagnose large bowel obstruction? Very similarly to how we diagnose small bowel obstruction. 04:38 So labs, nonspecific stuff. 04:41 You can look for electrolyte abnormalities. 04:43 You wanna look for an elevated white blood cell count potentially, and you can also look for an elevated lactic acid level. 04:50 You know, that elevated lactic acid level should point you in the direction that someone is having ischemia, decreased blood flow to their intestines, possible perforation. 04:59 That is a serious complication that you wanna make sure you're thinking about, and a lactic acid level can help stir you in one direction or the other. 05:07 You also wanna get imaging. 05:09 Here our options are plain film X-ray. 05:12 The CT scan, or colonoscopy, or water soluble enema. 05:18 This is a classic picture for a plain film X-ray. 05:23 So there is distended bowel loops and here you could see that you don’t see those plicae circulares, which are those fine white lines that cross across the bowel. 05:31 Again, similar concept to small bowel obstruction. 05:35 If you see a bowel obstruction, that’s great. 05:37 You can look for perforation as well, by looking for that free air in the abdominal cavity. 05:43 But, if you don’t see an obstruction, you're not done. 05:46 Sometimes even if you do see an obstruction or most of the times when you do see an obstruction, you still need to move on and get that CAT scan. 05:53 So definitely this is again a good first test, it’s an adequate first test, but it’s definitely oftentimes not your last test that you're getting when you're thinking about these patients.
About the Lecture
The lecture Large Bowel Obstruction (LBO – Emergency Medicine) by Sharon Bord, MD is from the course Abdominal and Genitourinary Emergencies. It contains the following chapters:
- Large Bowel Obstruction
- LBO Examination
- LBO Diagnosis
Included Quiz Questions
What is the most common cause of large bowel obstruction?
- Malignancy
- Hernia
- Volvulus
- Ileus
- Intussusception
What is Ogilvie's syndrome?
- A pseudo-obstruction of the large bowel due to autonomic malfunction
- A bowel obstruction due to strangulation
- A bowel obstruction due to hernia
- A bowel obstruction due to volvulus
- A bowel obstruction due to intussusception
What is the appropriate duration of auscultation of the abdomen when you are listening for bowel sounds?
- 2 minutes
- 15 seconds
- 30 seconds
- 45 seconds
- 1 minute
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |