Playlist
Show Playlist
Hide Playlist
Intraocular Pressure – Physiology Review
-
Slides Optic Pathology Glaucoma.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
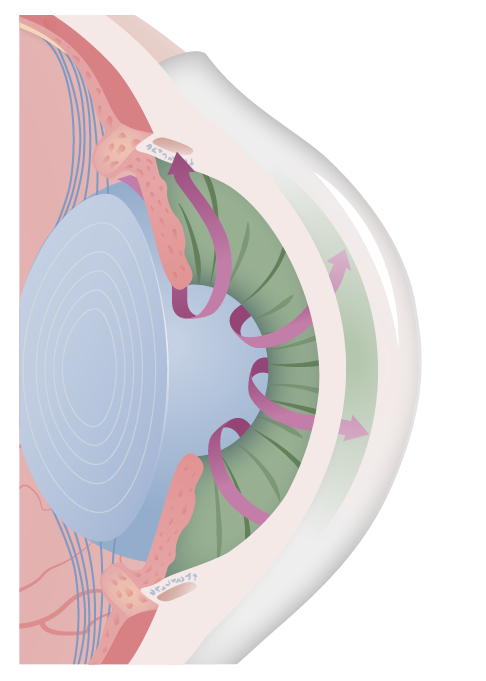
00:01 Welcome back. 00:03 As we go through our hit parade of diseases of the eye, we have been going from front to back. 00:09 We are now well into the anterior chamber and the uvea. 00:13 And glaucoma is a major disease that needs to be recognized. 00:18 This is something that can lead to blindness and if not appropriately identified a front, can have a lot of significant morbidity for the patient. 00:30 It may be asymptomatic as we'll talk about. 00:33 And so it's very important that we get regular screening for this to prevent the outcome of blindness. 00:40 So glaucoma. 00:43 Everything relevant to glaucoma pretty much starts right here. 00:46 So this is at the angle of the eye, what we're seeing in the little inset is the ciliary body and zonular fibers. 00:54 The ciliary body remember is part of the uvea. 00:58 Choroid, ciliary body and iris all constitute the uvea. 01:04 The ciliary body is also going to be a very important source of the fluid that will flow over the anterior chamber and lubricate the eye and provide nutrition to various elements of the eye. 01:16 This fluid produced by the ciliary body is what is going to accumulate or be at higher pressure and will be the cause of the glaucoma. 01:25 Ciliary body and besides making the fluid for the anterior chamber is also going to be the controller of the zonular fibers that will pull on the lens to stretch it or to relax it so that you can get appropriate refraction of light. 01:43 As indicated, changes in ciliary body production of aqueous humor or in the normal flow of that aqueous humor will lead to glaucoma. 01:54 And that's where we're going with this session. 01:57 Here's the general schematic. 01:58 So we've rotated the eye and the ciliary body is now down in the lower left and right hand corners. 02:05 What's up on top represents the cornea, you can see the beautifully green iris and you can see the pupil. 02:12 What happens is that the ciliary body makes the aqueous humor. 02:16 This is the clear fluid produced by the ciliary body and it comes out from the posterior chamber into the anterior chamber getting there via the open pupil. 02:26 Once it comes out through the pupil, then it flows out the canal of schlemm and a trabecular meshwork in order to get a circulation so that we don't accumulate excess fluids. 02:37 That's the normal kind of hydrodynamics of the aqueous humor. 02:42 The aqueous humors there, it preserves it maintains a certain intraocular pressure so that we have kind of the cornea situated above the rest of the eye. 02:54 It supplies nutrition and oxygen to the cornea and lens, very important because they are not vascularized and removes waste products from those same structures. 03:03 So it's doing an important circulatory function. 03:07 But we need to make sure that the pressure does not get too high. 03:11 In the same way that in our regular cardiovascular system, we don't want the pressure to get too high because there can be end organ damage. 03:18 Okay, same thing, just a different kind of fluid. 03:22 Again, things that will be important for thinking about is how do we control that intraocular pressure overall and parasympathetic stimulation will tend to reduce the intraocular pressure or IOP. 03:36 That will happen because parasympathetic stimulation will cause ciliary muscle contraction, so that you get miosis, that pupillary sphincter muscle contracts and you get that kind of closing like a diaphragm on a camera, and you get a smaller pupil. 03:52 When we do that, that actually reduces the angle improves the flow and reduces the intraocular pressure. 04:00 It will also open up the trabecular meshwork, the canal of schlemm. 04:04 Great name, I wish that you know I had discovered it so we can call it the canal of Mitchell but it's the canal of schlemm and that allows the flow out so we get good drainage. 04:14 That's your parasympathetic. 04:16 So conversely, if we look at what the sympathetic nervous system will do to it, it will tend to increase intraocular pressure, it will do so by causing relaxation of the ciliary muscles so that we end up with mydriasis that we are going to actually have increased activity of the dilator muscle and the pupils will get larger. 04:38 In doing so we close off the angle, we tend to increase the intraocular pressure. 04:42 Sympathetic stimulation also blocks the trabecular meshwork so that we will end up obviously with increased IOP. 04:49 Okay, so, this is what is going on. 04:52 Basically, when we're talking about glaucoma. 04:56 Now there are going to be various forms of glaucoma that have slightly different sort of mechanism. 05:01 But you can see if we block the flow, the x's there, block the flow of the aqueous fluid into the trabecular meshwork in the canal of schlemm then we will have obviously, no outflow from this chamber, from the anterior chamber, we're going to have increased pressure. 05:18 There are other mechanisms for this, but that's kind of a simplistic way of thinking about how this could happen. 05:24 Okay, normal pressure is between 8-21 mm Hg, significantly above that will then progressively lead to subsequent effects that we'll talk about. 05:35 So if we increase the pressure in the anterior chamber, this will eventually lead to increased pressure also within the vitreous chamber. 05:44 And when that happens, we will have optic neuropathy with atrophy of the optic nerve head is shown here, you can see the arrows pulsating out, the accumulating pressures. 05:55 There will be progressive visual field defects as we also compromised the optic or the neuronal outflow from the retina. 06:07 And this is typically but not always associated with elevated intraocular pressures. 06:12 We will talk about a normal pressure glaucoma that still leads to optic neuropathy but the pressures are within the normal range.
About the Lecture
The lecture Intraocular Pressure – Physiology Review by Richard Mitchell, MD, PhD is from the course Diseases of the Anterior Chamber and Uvea.
Included Quiz Questions
What can untreated glaucoma lead to?
- Blindness
- Photophobia
- Cataracts
- Blepharitis
- Strabismus
Involvement of what structure results in glaucoma?
- Ciliary body
- Choroid
- Iris
- Anterior chamber
- Pupil
What structure is associated with the drainage of the aqueous humor?
- Canal of Schlemm
- Superior lacrimal canaliculi
- Inferior lacrimal canaliculi
- Lacrimal duct
- Stensen's duct
What causes a decrease in the intraocular pressure?
- Miosis
- Mydriasis
- Mitosis
- Osmosis
- Meiosis
What is the normal range of IOP?
- 8–21 mm Hg
- 1–5 mm Hg
- 25–30 mm Hg
- 1–2 mm Hg
- 60–80 mm Hg
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |