Playlist
Show Playlist
Hide Playlist
Inotropy: Definition, Regulation and Effects – Cardiac Mechanics
-
Slides Physiology-Cardiac-Mechanics.pdf
-
Download Lecture Overview
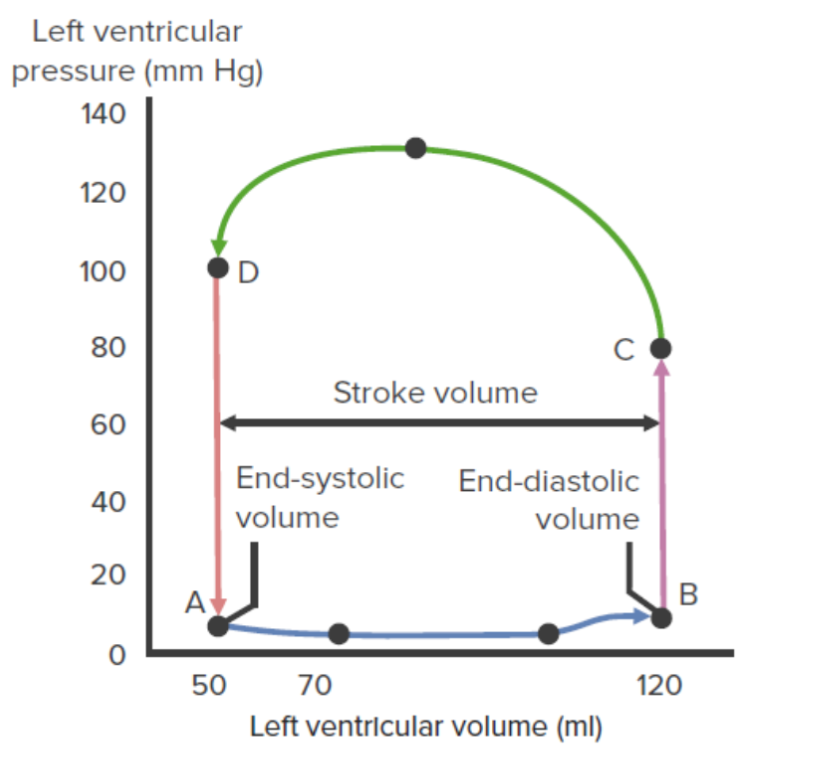
00:01 Inotropy is going to be the force at which a contraction occurs. 00:06 This is a length independent activation, meaning that it doesn't matter how much stretch the cardiac myocyte is under. 00:13 It’s how much force it's going to be able to contract. 00:17 In this case, it depends upon the preload, but it is independent of preload in many ways. 00:24 The stroke volume will increase, as you increase the force of contraction or inotropy. 00:34 So, what are the big factors that affect inotropy? There are four. 00:38 The first of which is sympathetic activation. 00:43 The more of a fight or flight response you have, the greater the contraction of each individual heartbeat. 00:51 You notice, or remember from previous lectures, that you also increase the beat frequency. 00:57 But in this case, you increase the strength of the contraction. 01:01 Circulating catecholamines is the second reason. 01:04 And again, a catecholamine is a blood-borne either epinephrine or norepinephrine. 01:10 It’s usually produced from the adrenal medulla and that will be traveling around to the circulation, bind to the beta-1 adrenergic receptors to increase ventricular inotropy. 01:22 The other two factors: One is an increase in heart rate. 01:26 And this is something called a Bowditch effect. 01:28 These particular effects, as the heart beats more and more frequently, it gets a little bit stronger in its contraction. 01:36 And this process, we’ll get into a little bit more with skeletal muscle, but in this case, know that the principle is the same. 01:44 The last thing that affects inotropy is going to be the afterload. 01:50 You have to overcome a certain afterload to be able to push out a particular amount of blood. 01:58 And if afterload increases, inotropy will increase to overcome that afterload because, remember, you have these interrelated effects. 02:12 So, let’s look at – I mean, inotropy affects ventricular function. 02:16 So, this curve, / we’ve seen a couple of times now, we're just going to talk you through how it affects inotropy. 02:23 We have left ventricular and diastolic pressure here on the x-axis and we have stroke volume here on the y-axis. 02:30 If we have an increase in inotropy, that is going to allow us to contract harder. 02:37 A decrease in inotropy, you contract less hard. 02:42 So, let's go through first an increase in inotropy. 02:45 So, that is going from A to C. 02:49 In this case, you can see that the whole curve shifts up to a new level. 02:53 Therefore, at a lower end-diastolic pressure, you can generate more stroke volume because you are contracting harder. 03:03 When you go from A to B, you’re contracting less hard. 03:08 Therefore, even at a higher left ventricular end-diastolic pressure, you’re not going to be able to garner as much stroke volume. 03:15 This increase in inotropy also involves an increase in ejection velocity. 03:21 In this man, it’s a nice thing to have happened because sometimes when you have a decrease in left ventricular end-systolic volume, there is also a need to be able to push that blood out very rapidly. 03:33 Another way to quantify this increase in inotropy is the development of pressure. 03:40 The faster you can develop pressure, the more inotropy you have. 03:45 So, oftentimes, that is another way we look at inotropy. 03:49 And we quantify by this dP/dT. 03:54 dP is a change in pressure over dT, which is a change in time. 04:00 The last way that we quantify that – we do this in the clinic quite a bit. 04:05 If you look at someone's ejection fraction – and ejection fraction is, per amount of stroke volume, what was the end-diastolic volume? If ejection fractions increase, that is an increase in inotropy. 04:21 If ejection fractions decrease, it is an index of a decrease in inotropy. 04:28 So, let's think about what causes a muscle contraction in a cardiac myocyte. 04:34 In this case, we have the release of norepinephrine from sympathetic nerve terminals. 04:40 It will bind to beta-1 adrenergic receptors, which increase cAMP. 04:46 cAMP will do two things for us. 04:49 The first is, it allows for calcium to enter via L-type calcium channels. 04:57 This calcium that enters also opens up calcium channels that are on the sarcoplasmic reticulum. 05:03 And this will release even more calcium. 05:06 So, this brings up an interesting concept, and that is cardiac myocytes use calcium-induced calcium release. 05:16 The calcium induced is the calcium going from outside the cell inside the cell, and then the calcium release is from the sarcoplasmic reticulum into the cytosol. 05:28 Calcium induce, calcium release. 05:31 The other thing that cAMP does is it phosphorylates a special protein called phospholamban. 05:38 Phospholamban will help facilitate the calcium ATPase or the calcium pump to pump more calcium back into the SR or sarcoplasmic reticulum. 05:50 That allows for the next contraction to be even greater. 05:54 So, we have multiple processes engaged by the sympathetic nervous system to cause this effect to happen. 06:02 The big point to remember here is the amount of calcium in the cytosol is very important. 06:08 The more calcium you have in the cytosol, the greater the strength of contraction or the more inotropy. 06:15 The less calcium you have, the lower the inotropy. 06:18 So, strength of contraction is always variable on the amount of calcium you have present. 06:25 The more calcium, the greater the contraction. 06:27 Less calcium, the less contraction. 06:30 That's why sympathetic stimulation releases calcium. 06:33 Why? To get an increased strength of contraction. 06:37 So, now, let's look at inotropy on everybody's favorite pressure-volume loops. 06:42 If we put our parameters out for our maximal and minimal, we put in our normal pressure-volume loop where we get ventricular filling, isovolumic contraction, ejection and isovolumic relaxation. 06:57 Here, let's first take an increase in inotropy. 07:03 An increased inotropy is an increased strength of contraction. 07:07 You notice this is the first time that we've altered a pressure-volume curve, in which we’ve altered that maximal value. 07:14 We’ve moved it upwards and a little bit to the left. 07:19 This upward shift allows us to use a new maximum curve to work on. 07:25 The end result is that you will have a lower end-systolic volume and a greater stroke volume. 07:33 If you have a decrease in inotropy, that is a lower strength of contraction, you’ll see that that line will shift downwards and to the right. 07:44 That means that per stroke, you won't get as much stroke volume per stroke. 07:53 Interestingly, when you're measuring this, it looks like the end-systolic volume is elevated, but this is simply an artifact of not pushing out as much blood per stroke.
About the Lecture
The lecture Inotropy: Definition, Regulation and Effects – Cardiac Mechanics by Thad Wilson, PhD is from the course Cardiac Physiology.
Included Quiz Questions
Which of the following effects on ventricular function happen with a decrease in inotropy?
- Decreases stroke volume
- Increases stroke volume
- Increase dP/dt
- Increase EF
- Decrease preload
Which of the following factors will increase ventricular inotropy?
- An increase in sympathetic nervous system stimulation
- A decrease in circulating catecholamines
- A decrease in heart rate
- A decrease in afterload
- Parasympathetic nervous system stimulation
Which of the following ions contributes most to the myocyte strength of contraction?
- Calcium
- Sodium
- Potassium
- Chloride
- Magnesium
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
The explanation is short and simple. Very easy to understand, it allows me the time to think about what is happening.