Playlist
Show Playlist
Hide Playlist
Type IV Hypersensitivity Reaction: CD8+ Cytotoxic T Cells
-
Slides Immune-mediated Diseases Type IV.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
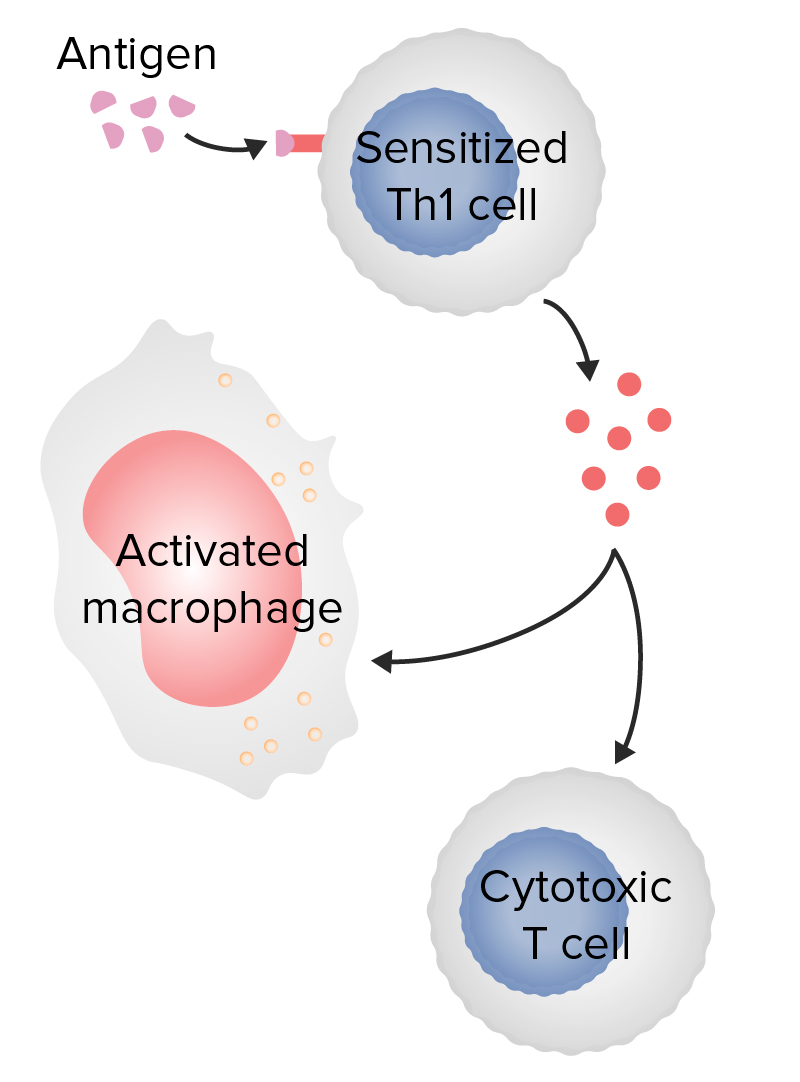
00:00 Hi and welcome back. Thus far, we've worked our way through type 1 hypersensitivity responses that's due to immunoglobulin E and mass cells. We've talked about type 2 which is antibody against fixed tissue antigen and type 3 which is immune complex-mediated disease. So those are all antibody-mediated disorders. Now, we're going to get into cell type cell-mediated disorders which is type 4 hypersensitivity. 00:28 So, they can be basically 2 flavors. We're going to talk about the effects related to cytotoxic T cells and effects secondary to helper T cells, driving a delayed type hypersensitivity. So this first one is easier to wrap our minds around. If we have cytotoxic T lymphocytes, again these are CD8+. They have that marker on their surface. 00:50 They are able to mind 2 newly synthesized intracellular proteins being expressed by MHC class 1 and when they recognize that, they will kill the cell that's expressing that. You get cell lysis and you get injury, pretty straightforward. So, what's an example of this in real life? Well, hepatitis B is a really good example. Here's our normal learner and you can see the hepatocytes, you can see the portal triad, central veins, but there's nothing going on here. However, if we now have hepatitis B infection, the virus has been able to get into the hepatocytes and is proliferating in that environment. It's making new hepatitis B antigens. The infected cell is sampling all the intracellular proteins including some of that virus, expresses that on its cell surface in association with MHC class I and low and behold cytotoxic T cells specific to that viral peptide and class I are able to recognize it and we get a chronic cytotoxic T cell mediated injury. That's the hepatitis. Actually, hepatitis is not directly a lytic infection for the most part. 02:11 The damage that occurs, the disease that occurs is because of the immune host recognizing the infected hepatocytes and clearing it. That's what it's supposed to do. 02:22 So if we're looking at this histologically, that's the top panel. If we're looking at it by immunohistochemistry, you can see that on the lower left hand panel we have cells, hepatocytes not yet killed that are expressing the hepatitis B surface antigen. That molecule will be processed and presented on the surface of the hepatocyte and then cytotoxic T lymphocytes, CD8+ T cells will come along on the lower right hand panel and kill them. And that whole process will stop once we've killed off every infected cell. Okay, these all make sense. It's a type 4 hypersensitivity response, cell-mediated. So, the circulating CTLs will kill the viral infected hepatocytes. 03:06 The amount of infiltrate will correlate with the amount of liver injury. So if you're measuring the normal liver enzymes that are present, if you have a big inflammatory response, we'll have a big leak of those proteins and that we can measure in the peripheral blood. And conversely, if it's a little tiny area of inflammation, we may not get much of a leak of those proteins. And once the T cells have done their job, then there are no more cells to kill because all the infected ones have been killed and we're done. After the virus is cleared, the infiltrate goes away and the liver that has been irreversibly killed by apoptosis regenerates. That's one of the nice things about liver. Most people who will get a hepatitis B infection will have a self-limited infection that runs its course over a couple or 3 weeks and then we've killed off all the infected cells and the liver comes back. Hurray. That's what's supposed to happen. But, if you are one of the 20% or so of people who will get a hepatitis B infection and not develop a sufficiently robust T cell response to clear the infection, you will have chronic hepatitis. So those T cells, for whatever reason, probably because of receptor recognition, etc. are less effective at killing. And so the virus continues to infect adjacent hepatocytes. We continue to have kind of a half-hearted attempt by the cytotoxic T lymphocytes to get rid of them and you have an ongoing hepatitis. So that's chronic active hepatitis. Carrier states can also occur. So about 10% of the population, roughly speaking, doesn't have the T cell repertoire necessary to recognize infected hepatocytes. So that carrier state happens when there's no immune response and you and the virus more or less live happily ever after together in that case. Now you can transmit virus, you are communicable but you don't have the disease because you don't have the T cells that can kill off the infected cells. And what's being shown in the lower right panel is just that a hepatitis B carrier they get so-called ground glass cytoplasm and sanded nuclei. That ground glass eosinophilic cytoplasm is because the cells basically become viral factories and they're just chockfull of all the little viral particles. 05:33 If you're constantly producing antibody to viral antigens and the viral antigens continue to be expressed, you form immune complexes and those immune complexes can deposit. So in fact, polyarteritis nodosa, which is what is being shown there with a necrotizing vasculitis, fibrinoid necrosis, atypical type 3 hypersensitivity response due to immune complex deposition. A significant number of patients with polyarteritis nodosa come from patients who have chronic hepatitis. So, immune complex disease can occur. Hopefully the virus is clear by the activities of the cytotoxic T lymphocytes. That's how you clear the primary infection. How do you prevent against a secondary infection? Because you have protective now antibodies that neutralize the virus. So the next time you see that hepatitis B virus, your immune cells, your antibodies will bind to the virus and clear it before it can ever access the liver so that you have protection against subsequent infection due to a B cell response. So, the virus will be cleared by a cytotoxic T cell response and protection is conferred by antibodies to the virus. Another disease that cytotoxic T lymphocyte mediated is myocarditis. This is an example of a lymphocytic myocarditis where there are a number of cytotoxic T cells that are directly killing the myocytes. So we will have apoptotic death of many of the myocytes. But, it's important point as shown in that first bullet. Although there is parenchymal cell killing in the setting, that's not only or even necessarily the major mode of injury. 07:28 So there will be similar recognition of MHC molecules on the endothelium. 07:35 So we will get endothelial cell damage. When that happens, you get thrombosis and with that you get ischemia or infarction. There will also be cytokines that are elaborated. So there are helper T cells in here, there are cytotoxic T cells that are in here, they are making a variety of cytokines including things like interferon gamma which will cause vascular leakiness. So the heart becomes boggy, it becomes edematous and we separate the individual myocytes so there isn't good connection cell to cell to cell. The production of the cytokines will also affect the ability of the heart to squeeze. So the heart normally has a fairly robust squeezing relaxation, squeezing relaxation. If I dump on to them or release from the inflammatory cells that are present, things like interferon gamma, we will cause those myocytes to contract less forcefully. So in particular, interferon gamma acting on a cardiac myocyte causes a production of nitric oxide thru nitric oxide synthase and that will cause relaxation of those cells. So instead of squeezing vigorously like a New Yorker walking on the street, they're squeezing kind of like a Californian on the beach and that's why you can get significant functional damage even in the setting of not so much individual cell death in myocarditis. So kind of an overview of the mechanisms of CTL-mediated pathology. Cytotoxic CD8+ T cells can kill their target directly. Okay, we've covered that. It's important to know that during this process these killer T cells are also elaborating cytokines that can recruit additional inflammatory cells or can have secondary effects directly on the tissue. But in general, with this form of hypersensitivity response type 4 due to CTLs, there's usually minimal bystander injury. This is pretty targeted. Yes, there can be the substantial amount of injury but there is not much bystander, there is not much collateral damage. So examples of this include hepatitis which we talked about, myocarditis, encephalitis due to certain viruses, and HIV AIDS is going to be because we have CTLs killing virally infected helper T cells.
About the Lecture
The lecture Type IV Hypersensitivity Reaction: CD8+ Cytotoxic T Cells by Richard Mitchell, MD, PhD is from the course Immune-mediated Diseases.
Included Quiz Questions
A type IV hypersensitivity reaction is primarily mediated by which of the following cells?
- T cells
- B cells
- NK cells
- Eosinophils
- Neutrophils
Which of the following is an example of a type IV hypersensitivity reaction?
- Myocarditis
- Myasthenia gravis
- Poststreptococcal glomerulonephritis
- Autoimmune hemolytic anemia
- Goodpasture disease
Which of the following is an example of a type IV hypersensitivity reaction?
- Hepatitis B
- Asthma
- Systemic lupus erythematosus
- Anaphylactic shock
- Acute rheumatic fever
Which of the following is an example of a type IV hypersensitivity reaction?
- HIV/AIDS
- Graves disease
- ANCA-associated vasculitis
- Pemphigus vulgaris
- Hay fever
Which of the following is an example of a type IV hypersensitivity reaction?
- Encephalitis due to certain viruses
- Serum sickness
- Rheumatoid arthritis
- Polyarteritis nodosa
- Food allergy
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |