Playlist
Show Playlist
Hide Playlist
Hypertrophic Obstructive Cardiomyopathy – Systolic Murmurs
-
Reference List Physical Examination.pdf
-
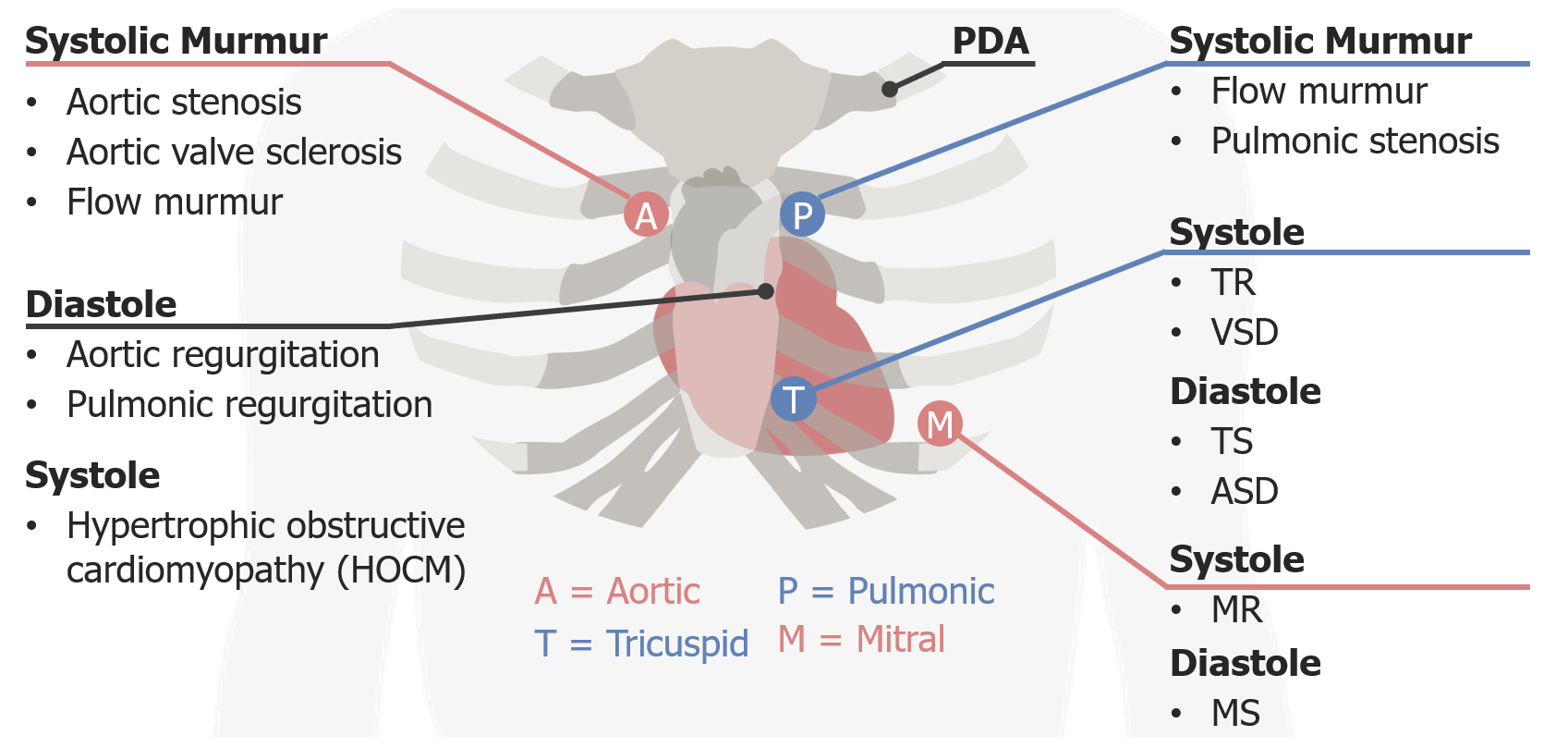
Download Lecture Overview
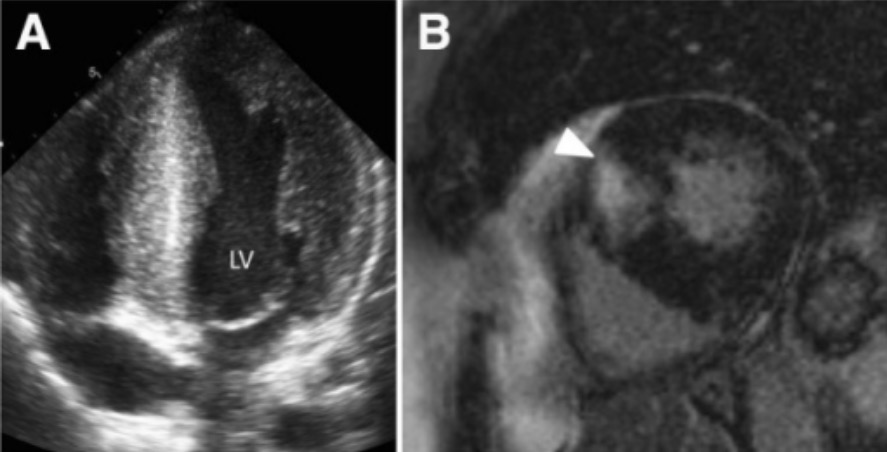
00:01 Alright, so the next murmur we're going to talk about is an extremely important pathologic problem in the heart which is HOCM, hypertrophic obstructive cardiomyopathy. 00:11 This is not a terribly common murmur but it's one which is really important to catch particularly since it ca present with sudden cardiac death in young athletes, not to mention to older people as well depending upon the subtype of HOCM that a patient may have. 00:27 This is, as I've suggested, a systolic murmur and in some ways it mirrors some of the features of other systolic murmurs with one important caveat which we'll get to in a moment. 00:38 So HOCM is best heard at the left lower sternal border kind of over the tricuspid area. 00:43 It is a harsh sound similar to the sound we might hear [making a sound] in the back of the throat with aortic stenosis murmur, and the intensity of it can be wide ranging. 00:56 Some people with severe HOCM actually don't even have a murmur, but nonetheless, the severity or intensity can be -- can correlate with the severity of disease. 01:06 The pitch is also fairly low as I've alluded to and the timing can be very variable. 01:10 The most important distinguishing feature of HOCM and this is definitely a board's review type question, is what happens to this murmur with Valsalva? Almost every murmur in the body with one other exception, that is mitral valve prolapse, which we're not going into right now, will decrease in intensity when you perform the Valsalva maneuver. 01:31 This is the one murmur where if you perform the Valsalva maneuver, and the murmur is louder, the likelihood ratio in support of this being HOCM is very high. 01:41 So, what's a Valsalva maneuver? Let's demonstrate that now. 01:45 So the Valsalva maneuver is when you asked your patient to basically bear down, almost as if they're having a bowel movement and by exerting that abdominal pressure, you're basically having the patient squeeze their upper chest against a closed glottis, so they're contracting all those muscles of respiration as if they're trying to forcefully exude air but since they have a closed glottis, all they're doing is dramatically increasing intrathoracic pressure. 02:13 I said before, that when you take a breath, you're decreasing intrathoracic pressure cuz you're creating a vacuum. 02:19 This is a the opposite, you're dramatically increasing intrathoracic pressure and by doing so, you are preventing blood return to the heart, you're telling the IVC and the SVC to not deliver blood to the right side of the heart when you perform this maneuver. 02:36 As such, you're decreasing blood to the right side of the heart, eventually, that means less blood to the pulmonary vascular bed and then to the left side of the heart, so you're decreasing preload, decreasing venous return. 02:49 So as I suggested before for most murmurs, if you decrease the amount of blood running to the heart that should decrease most murmurs, right? Less blood means less turbulent flow. 02:58 But with HOCM, what's happening in HOCM is that the stenosis, the source of murmur is underneath the aortic valve down here, there's extra tissue in the either intraventricular septum or elsewhere in the left ventricular, that as the walls of the left ventricle gets smaller with decrease preload, that stenotic area has now been brought closer together which tightens the area through which blood needs to get out, so when you have the large heart, a dilated heart with lots of blood going in there, those walls which were closing in are now separated, the murmur will be less, but as you do Valsalva, you're slowly decreasing the walls of that heart with each contraction and now, that turbulent flow around that bend in the intraventricular septum, if you will, is now creating a louder murmur. 03:47 So, let's do Valsalva in our patient and see what we find. 03:52 So what I'm going to have you do Shaun, as I want you to simply bear down as if you're holding, as if you're having a bowel movement and you're just basically holding your breath throughout this whole time, and go ahead. Great. 04:17 One quick tip by the way, for the events practitioner, anytime you have a patient hold their breath, hold your breath as well. I did that while he was holding his breath. 04:29 I didn't take a deep breath, but I held my breath, cuz otherwise you'll forget your patient is holding their breath, they'll turn blue in the face and pass out on you especially if they're prone to following orders. 04:38 So just a little trick to remember to do that all the time. 04:41 So, in this case, if I'd heard that murmur louder or if a murmur had been brought out during Valsalva, I would have been concerned about HOCM and that has a very significant implication for this patient.
About the Lecture
The lecture Hypertrophic Obstructive Cardiomyopathy – Systolic Murmurs by Stephen Holt, MD, MS is from the course Examination of Cardiovascular and Respiratory System.
Included Quiz Questions
Which features are the MOST accurate descriptions of the murmur associated with hypertrophic obstructive cardiomyopathy?
- Located at the left lower sternal border, heard during systole, increase in intensity with Valsalva maneuver
- Located at the right upper sternal border, heard during systole, may radiate to the right carotid area
- Located at the left lower sternal border, heard during diastole, may radiate to the apex
- Located at the apex of the heart, heard during diastole, may radiate to the right carotid area
- Located at the left lower sternal border, heard during systole, decrease in intensity with Valsalva maneuver
How does the Valsalva maneuver increase the intensity of the murmur that is heard on an exam?
- It decreases preload.
- It increases preload.
- It increases afterload.
- It decreases afterload.
- It increases contractility.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
The use of tips for practicing, diagrams alongside the lecture and having a patient present made this interesting and easy to remember.
1 customer review without text
1 user review without text