Playlist
Show Playlist
Hide Playlist
Hypertrophic Obstructive Cardiomyopathy
-
Slides ValvularHeart DiseaseDynamicAuscultation CardiovascularPathology.pdf
-
Download Lecture Overview
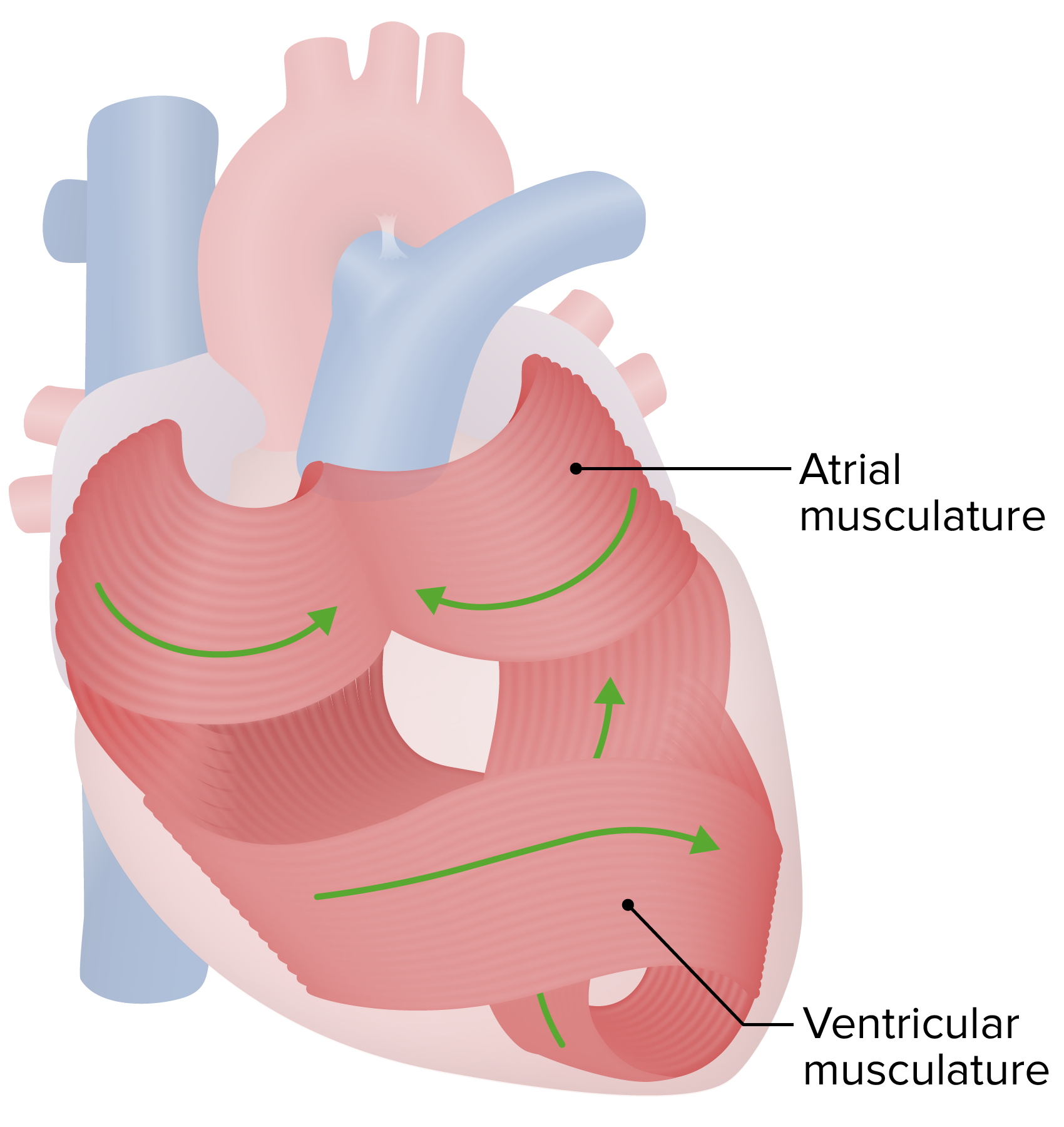
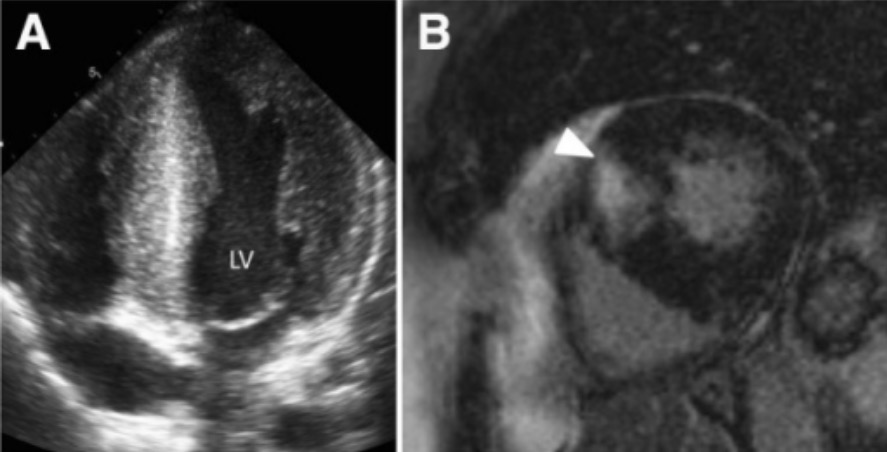
00:01 Let us get into an important topic called hypertrophic obstructive cardiomyopathy. First we will walk through the pathophys and then we will take a look at various maneuvers once again in which you will clearly be able to see as to how these maneuvers are going to affect that particular pathology. In hypertrophic obstructive, now there is hypertrophic cardiomyopathy, in general, okay. That is a general type of cardiomyopathy. HCM along with RCM, NDCM. 00:32 Theoe are all different types of cardiomyopathies. The one that we will focus upon is hypertrophic cardiomyopathy, specifically the obstructive type. What does that even mean? This is the one in which the outflow tract from the left ventricle, going into the aorta. Do you see the arch of aorta there in dark green? And there is your left ventricle and that's a chamber and it's the fact that you have blood? That is then or should be ejected from your left ventricle into the aorta, correct? Well, I want you to pay attention to the intraventricular septum and the outflow tract would be the exactly as it would imply the outflow of blood from your left ventricle into the aorta. And the intraventricular septum that you are seeing there and only exclusively on the left side, you have asymmetrical hypertrophy of the left side of the intraventricular septum. So lie down there, listen to what I just said and make sense of this picture. That intraventricular septum that you are seeing there with the aysmmetrical hypertrophy, moving into the chamber of the left ventricle is causing obstruction of the outflow. May I ask you a question? Who is this patient? Inspiration, leaning back, ouch, I have chest pain. But what then causes your chest pain to be relieved? Hey doc, leaning forward. Expiration, what does that mean to you? Pericarditis. What do I bring this up? Why was there increased pain upon leaning back and inspiration? Inspiration increases the amount of blood and with leaning back, pericarditis is my diagnosis in which the space between the pericardial cavity is then going to cause friction and hence the pain. 02:24 Why do I bring that up? Because the two layers here that you want to be able to keep seperate so that the intensity of the murmur is going to be decreased would be that outflow tract. So if you are able to keep the left sided asymmetrical hypertrophy, away from the wall of the aortic valve, then guess what? You are able to decrease the intensity of the murmur. Who is this patient? Unfortunately it is a patient in which we are seeing for all intended purposes, perfectly normal. In fact, perhaps even too normal in terms of being maybe a star athelete. So there is nothing in terms of obesity, in terms of maybe lack of proper nutrition and such, that would have contribute to the issue. Genetically speaking, autosomal dominant, one of the major contractile fiber is beta-myosin, which is then affected in this patient, resulting in asymmetrical hypertrophy and obstruction of the outflow. And so therefore, the closure that the outflow tract gets the worse off is the intensity of the murmur and the fact that the patient is going to have such little cardiac output. Next time that he or she goes for an exertional type of activity, collapses onto the floor, never to get up ever again. Sad. So your next question is what kind of maneuvers are you going to perform or are you going to see? What kind of drugs might you want to give in which what do you want to do here with obstruction? You want to relieve the murmur by increasing space of the outflow tract. How would you go by doing that? How about increase the amount of blood in the outflow tract? About increase the amount of preload in your left ventricle so that you keep the areas seperate and apart. And by doing so, would you be able to alleviate the symptoms of the patient and perhaps even save your patient? Oh! My goodness yes and so, therefore, what kind of drugs might you be thinking about? What kind of drug might you want to give so that you would be keeping more blood in your heart please, a negative or positive inotropic agent? A negative inotropic agent such as a beta-blocker, such as a calcium-channel blocker. By doing so, you then create negative inotrophy, increased preload and seperation of your outflow tract. Quite different isn't it, when compared to aortic stenosis and such. It is still systolic murmur. This is hypertrophic obstructive. Where would you hear this? We've talked about this earlier as well. Hypertrophic obstructive. Take a look at the arch of the aorta. Normally where would you hear the aortic valve? Second intercostal space right parasternum and then the outflow tract will be towards the apex. It would be approximately third intercostal in left parasternal. Is that clear? So systolic murmur. Both aortic stenosis and hypertrophic obstructive, but the locations are different based on the anatomy that you are seeing here. Let us continue. 05:42 Physical examination, a systolic ejection murmur, heard where? Over the aortic area similar to aortic stenosis, but the outflow tract, so you could technically and will technically hear on the left parasternal. Murmur, now be careful, take your time. You want that seperation of the outflow tract. Correct? Are you with me? If you want the seperation of the outflow tract you want less or more blood in your heart? You want there to be more blood in your heart so you have more seperation at the outflow tract. When you do a Valsalva maneuver, phase II is what? I assume you know that this is we're referring to, then there is decreased venous return to the left side. There is going to be less blood in your heart. Pay attention. 06:28 One, there is less blood in your blood. Tell me about the outflow tract. It is closer together. 06:34 What then happens to the intensity of the murmur? It will worsen. What do you think when you are standing up? Same concept. Standing up, the blood is in your legs. Therefore, you have decreased return to the heart, thus worsening of HOCM, hypertrophic obstructive cardiomyopathy. Versus, what if you squat quickly? You increase your venous return, quickly squatting. 06:57 Remember this is not a tet spell. Rapid squatting increases the amount of blood to your heart and so, therefore, you are thinking about your outflow tract, which is now more seperated. 07:09 What if you do a handgrip? If you do a handgrip, what is interesting? It is that you will be referring to what? More of an influence on your afterload resulting in its increase thus there is going to be more blood left where? In your left ventricle. Is that clear? So, therefore, what happens to seperation? It is increased. What happens to intensity of the murmur? It diminishes. If you have understood all this, you are in great shape with HOCM. 07:33 Now as we progress, we are going to put all the murmurs together with all the different maneuvers. You probably want to keep coming back to this lecture series so that you see as to how well you have understood this material and then it becomes part of your unconcsious reflex. The physical examination, double beat bifid or spike and dome carotid pulse, hypertrophic obstructive. It differs from aortic stenosis, which has what is known as what? Slow and delayed up in the carotid. Remember that is called pulsus parvus et tardus. Delayed and it is going to be slowed with aortic stenosis. 08:09 Whereas it is bifid kind of like a double beat when you have hypertrophic obstructive. Not the same thing.
About the Lecture
The lecture Hypertrophic Obstructive Cardiomyopathy by Carlo Raj, MD is from the course Valvular Heart Disease: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following would increase the intensity of the murmur in hypertrophic obstructive cardiomyopathy?
- Valsalva maneuver
- Increased preload
- Increased afterload
- Handgrip
- Squatting
Which of the following is NOTtrue regarding hypertrophic obstructive cardiomyopathy?
- It presents with pulsus parvus et tardus.
- It is the result of an autosomal dominant gene.
- It is due to an outflow tract obstruction.
- There is asymmetrical hypertrophy of the left interventricular septum.
- It presents with a systolic ejection murmur.
Which of the following genes could be affected in hypertrophic obstructive cardiomyopathy?
- Beta myosin gene
- Alpha myosin light-chain gene
- PKD1 gene
- CFTR gene
- PKD2 gene
Which of the following is the best area to auscultate for the murmur of hypertrophic obstructive cardiomyopathy?
- 3rd intercostal space, left parasternal border
- 2nd intercostal space, right parasternal border
- 2nd intercostal space, left parasternal border
- 5th intercostal space, midclavicular line
- 3rd intercostal space, right parasternal border
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |