Playlist
Show Playlist
Hide Playlist
Hypertrophic Cardiomyopathy – Cardiomyopathy
-
Slides 05 Cardiology Alpert.pdf
-
Reference List Cardiology.pdf
-
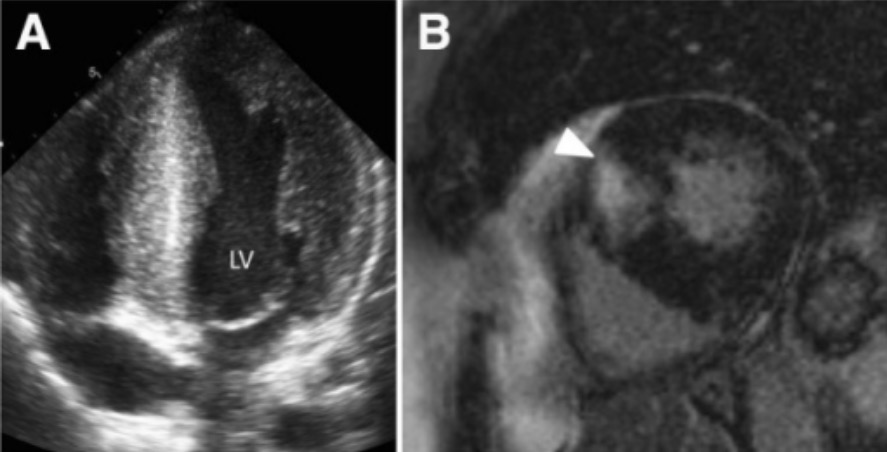
Download Lecture Overview
00:00 Hypertrophic cardiomyopathy is the other very common form of cardiomyopathy in the population. 00:06 It occurs in about a hundred out of a hundred thousand people, and as I've said before, most of these individuals have the disease in a completely benign form. 00:16 They live long lives and they have no problems. 00:19 The disease is genetic. It's an autosomal dominant inheritance and there have now been discovered more than 1,000 different mutations that lead to hypertrophic cardiomyopathy. 00:30 What happens is that the heart muscle cells developed in an abnormal fashion so that instead of being lined up and parallel, they are in a random order and they pull against each other in abnormal fashion so that there is a mark tendency for individual cells to hypertrophy. 00:50 That is to increase in size and volume, and this of course, then results eventually in a marked increase in size and volume of the left ventricle. 00:58 There are a variety of different forms of hypertrophic cardiomyopathy, the commonest one involves marked hypertrophy of the septum, but there can be forms in which the apex is hypertrophied, the base is hypertrophied, and even sometimes the hypertrophy extends into the right ventricle. 01:16 When the disease was first described in the 1960s, it was thought to be a horrible thing. Why? Because we only saw patients who were hospitalized with complications. 01:25 Well, about 20 years ago, the Italians did a whole community survey where they went into a community and they did echocardiograms on everybody in the community. 01:34 And what they discovered was large numbers of patients with hypertrophic cardiomyopathy who were living normal life expectancies who got to old age and in fact, I've seen patients well into their 90s with hypertrophic cardiomyopathy. 01:49 It turns out, the vast majority of patients with hypertrophic cardiomyopathy do just fine. 01:55 However, there is a small subgroup that has malignant ventricular arrhythmias and as I said before, the commonest cause of death in young athletes who are involved in sports, particularly in high competition sports. 02:12 Basketball, football, soccer, and so forth. 02:14 These individuals can develop malignant arrhythmias and have cardiac arrest on the playing field. 02:21 Again, a genetic disease, quite common, but in the main quite benign. 02:29 And here, you see some statistics or for how common in the population. 02:33 Not that common, certainly nowhere near as common as coronary artery disease, but nevertheless, more common, a little more common than the dilated cardiomyopathy, at least in some series. 02:47 Although in other series, the two are almost equivalent. 02:51 So, let's take a look, again, at the genetic underlying factor. 02:58 I think I told you already, it has to do with abnormalities in the DNA that lead to abnormalities in the contraction machinery of the heart, and that there's a thousand different mutations that lead to this disease, and there's a variety of forms. And we'll take a little look at that. 03:15 All right, so here's a diagram. 03:17 Again, the same one you saw for the dilated cardiomyopathy. 03:21 On the left-hand side, you see the normal ventricular structure. 03:26 Normal left ventricle, normal right ventricle. 03:28 Now, look over to the right and you see a typical abnormality and diagram of a hypertrophic myopathy. 03:35 The septum is much thicker than normal and the free wall is much thicker than normal, and you'll notice that the cavity size is markedly reduced. 03:45 Now, there are a number of things that can occur in the patient with hypertrophic myopathy. 03:55 Sometimes, the bulging septum, you can see it here in this diagram, actually gets in the way of the left ventricular outflow track and actually impairs blood, leaving the heart just as if they were aortic stenosis. 04:09 In fact, this when it was first described, was called subaortic stenosis. 04:14 That is stenosis that's below the aortic valve. 04:18 That's one form of sept -- so called septal hypertrophic cardiomyopathy. 04:24 But as I've said before, you can have a hypertrophy in other parts of the left ventricle and on occasion, even the right ventricle is involved. 04:33 The thickened heart muscle has impaired relaxation, so the diastolic filling pressures of the ventricle is -- are increased and this often results in increase in lung pressures that can lead to edema in the lung, and increased pulmonary pressures and then even some difficulty for the right ventricle. 04:54 And as I said, the form with the big, thickened septum can often be obstructive to the outflow tract of the left ventricle, and can actually function like aortic stenosis below the aortic valve. 05:09 The symptoms are variable. Most patients have no symptoms and they may be discovered routinely because they have an abnormal electrocardiogram, somebody gets an echo and says, "Oh, you know, you have a hypertrophic myopathy." We then go through the family and find a number of family members. 05:26 The vast majority are asymptomatic and lead normal lives, need no therapy, other than being regularly watched by their doctor. 05:35 I follow a number of people in my clinic, including one of the former hire officers of the University of Arizona who's now in his 60s and he was found out by accident to have hypertrophic cardiomyopathy when a cardiogram was abnormal. 05:49 He hikes vigorously, he's had absolutely no problems despite his hypertrophic cardiomyopathy, and I've seen people in their 90s with it who are also asymptomatic. 05:59 The individuals who are symptomatic often complain of shortness of breath with exertion, they may actually even develop angina, or the most worrisome symptoms is fainting, syncope, with exertion. 06:12 That's the patient that's high risk for sudden death. 06:15 Again, in this case, the syncope is, as my professor had said, aboarded sudden death. 06:22 There are number of signs when you examine the patient. 06:25 Very often, they have a systolic murmur that sounds a little bit like aortic stenosis, but it gets louder when the patient stands up or when the patient does the Valsalva maneuver, that's the same maneuver where you grunt like this as you're moving your bowels. 06:38 Each of those shrinks the left ventricular cavity a bit and causes obstruction to the outflow tract and the murmur gets louder. 06:47 So, you have the patient stand, the murmur gets louder, you have the patient lie down, and the murmur gets softer cuz the ventricle gets a little more blood and dilates up a little bit. There may be a very muscular apex beat that you feel on the chest wall and there may be evidence of arrhythmias, abnormalities, in the regularity of the heartbeat. 07:12 The treatment is usually non vaso dilating beta blockers like metoprolol, succinate or natal all in fairly high doses. 07:19 We typically start at 25mg daily and increase as tolerated. 07:23 This decreases some of the hyper contractile components of this disease. 07:27 For patients who can't tolerate beta blockers or have inadequate response. 07:31 Calcium channel blockers like verapamil are used as an alternative, starting at 120 to 180mg daily. 07:39 When the patients are thought to be of high risk, they will often have an implantable defibrillator or pacemaker that can detect an abnormal malignant heart rhythm and shock the heart, or they may undergo surgical therapy, in which a portion of the thickened septum is removed, often with considerable improvement. 07:54 While medications haven't been proven to prevent sudden death. 07:58 Surgical may ectomy may provide some protection against sudden cardiac death. 08:02 However, in patients who are high risk for sudden death, for example, the people I mentioned before who faint, we put in a defibrillator for patients with persistent symptoms. 08:12 Despite beta blockers or calcium channel blockers disappear. 08:15 Amide is an effective option. 08:17 It's a negative in a tropic agent that reduces contractility and outflow obstruction. 08:22 It must always be used in combination with beta blockers or calcium channel blockers, but never alone. 08:28 Typical starting dose is 300mg daily, with ECG monitoring for QT prolongation. About two-thirds of patients experience symptom improvement, though anticholinergic side effects limit tolerability in about 10%. 08:42 And I'll show you a slide of the defibrillator, the implantable defibrillator, that's put into patients we think are high risk for sudden death or who have been resuscitated from sudden death. 08:52 There is one therapy where alcohol is injected down a branch of one of the coronary arteries, killing some of the heart muscle. 09:00 This procedure, called alcohol septal ablation, is performed during cardiac catheterization and creates a controlled myocardial infarction in the basal septum. 09:09 It's less invasive than surgery and results in symptom reduction in approximately 90% of patients, compared to 95% with surgical Mei ectomy. 09:19 A significant recent advancement is Marva Compton, a first in class cardiac myosin inhibitor approved in 2022. 09:25 It's specifically for adults with symptomatic New York Heart Association class 2 to 3 obstructive hypertrophic cardiomyopathy with left ventricular ejection fraction greater than or equal to 55%. 09:38 Clinical trials show it improves exercise capacity, reduces outflow gradients, and may reduce the need for invasive procedures. 09:45 However, it requires regular e chocardiographic monitoring and is contraindicated in pregnancy. 09:51 And I'm gonna show you some diagrams of this. 09:54 This slide just, again, points out the surgical interventions and the possibility of implanting a defibrillator in patients who have malignant arrhythmias, and of course, we also pay attention to things like minerals in the blood, potassium, and so forth, even when patients have been operated on, they often end up still requiring drugs when they're symptomatic. 10:19 Most of the asymptomatic patients with hypertrophic cardiomyopathy require no therapy other than monitoring them to make sure that they're not getting worse in any way. 10:32 Here's just a little diagram to show you the alcohol septal ablation. 10:37 You see on the left part of the diagram, shows you the thickened left ventricle, shows you the left anterior descending coronary artery, a catheter is placed down on a branch, and you can see on the right hand side, some injection of alcohol and that heart muscle dies. 10:52 It is, by the way, quite painful when we inject the alcohol. 10:55 So the patients need to have significant drugs on board, morphine and so forth to dull the pain. 11:00 This technique, alcohol septal ablation, has evolved to become a viable alternative to surgical ectomy for appropriately selected patients. 11:09 Current data shows similar long term mortality between the two procedures. 11:14 Surgical myectomy is typically preferred for younger patients, those with very thick septa or those needing concomitant cardiac surgery, while alcohol septal ablation may be more appropriate for older patients or those with significant comorbidities. 11:27 These procedures are not done by all cardiac specialists since they're not done that often. 11:32 Most are performed in specialized centers where surgeons and interventional cardiologists become very expert at doing them. 11:39 So, if you need that operation, of course you wanna go to somebody who's doing this all the time, not somebody who just does one on occasion.
About the Lecture
The lecture Hypertrophic Cardiomyopathy – Cardiomyopathy by Joseph Alpert, MD is from the course Cardiac Diseases.
Included Quiz Questions
Which of the following is the typical location of hypertrophy in hypertrophic cardiomyopathy?
- Interventricular septum
- Lateral wall of the left ventricle
- Ventricular apex
- Outflow tract of the right ventricle
- Atria
Which of the following is not a characteristic finding in hypertrophic cardiomyopathy?
- Larger size of the left ventricular chamber
- Obstruction to blood flow from the heart
- Impaired relaxation
- Rapid, forceful contraction of left ventricle
- Increased pulmonary pressure
Which of the following maneuvers would increase the murmur of hypertrophic cardiomyopathy?
- Standing
- Squatting
- Lying supine
- Lying in the left lateral position
- Hand-grip
Which of the following is the first-line agent in reducing obstruction in hypertrophic cardiomyopathy?
- Metoprolol
- Digoxin
- Furosemide
- Lisinopril
- Amlodipine
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
excellent lectures. Easily understable and very efficent for university exams