Playlist
Show Playlist
Hide Playlist
Hypersensitivity Pneumonitis
-
Slides 06 ILD InterstitialLungDisease RespiratoryAdvanced.pdf
-
Download Lecture Overview
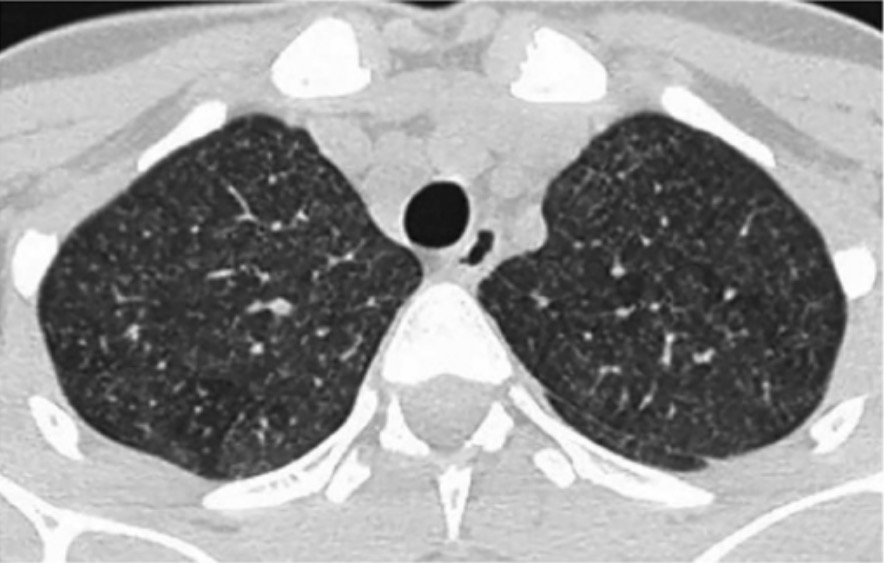
00:01 Now, to pulmonary fibrosis. 00:05 The other major non-sarcoid cause of interstitial lung disease are hypersensitivity pneumonitis. 00:10 This is an interstitial lung disease caused by an immunological reaction to an inhaled antigen. It is an allergy. And the antigen that causes it, depends usually on either your occupation or your hobby. The commonest examples are Bird fancier's lung which tends to affect people who keep parrots or may have used to be called Pigeon fancier's lung as well because those who kept pigeons for racing would also get this disease; and farmer's lung where up to 5% of farmers develop an antibody response to moulds and unusual bacteria that can live in a mouldy hay. And some of those patients will develop a hypersensitivity pneumonitis as well. There's a very large range of funny diseases which are hypersensitivity pneumonitis, mushroom pickers lung, cotton pickers lung, hot tub disease, snuff takers lung, etc etc. There is an ILD reaction to the inhaled antigen. It causes a cell mediated hypersensitivity reaction forming small granulomas which are not terribly well defined, a mononuclear infiltrate, and that will lead to eventually fibrosis around the small airways. There are two clinical presentations for hypersensitivity pneumonitis, broadly speaking. One is that there's an acute presentation where the patient will present with what seems to be actually a chest infection. They're breathless, they've got cough, they have fever, and they have crackles, and that occurs in a few hours of exposure to the antigen to which they're allergic. And when you take them away from their antigen, actually, the disease settles very quickly within a couple of days by itself. 01:49 If you have repeated episodes of acute hypersensitivity pneumonitis, then that might lead to chronic hypersensitivity pneumonitis. And chronic hypersensitivity pneumonitis presents more like pulmonary fibrosis with chronic dyspnoea, generally progressive over time, cough. 02:05 But in addition, they may get some systemic mild symptoms such as fatigue and weight loss. 02:11 You don't actually have to have acute preceding episodes of acute hypersensitivity pneumonitis to develop chronic hypersensitivity pneumonitis. Most patients, in fact, with chronic disease, seem to have no clear evidence of acute episodes previously. 02:24 The thing about hypersensitivity pneumonitis is that to identify it, you really need to think about it and ask the patient carefully about potential occupational and social circumstances that might lead them to having hypersensitivity pneumonitis such as, do they keep budgerigars, do they keep birds, and so on and so on to try and identify the potential possibility of a hypersensitivity pneumonitis. Diagnosis falls or lies with pulmonary fibrosis with chest X-ray, lung function, and CT scan, but there are some differences that you get with hypersensitivity pneumonitis compared to pulmonary fibrosis which allow you to differentiate these patients. For example, acute hypersensitivity pneumonitis would present with patchy diffuse infiltrates that actually often mistaken for pneumonia. 03:11 Chronic hypersensitivity pneumonitis cause reticulonodular shadowing but with an upper lobe predominance, which is unlike fibrosis which normally is a lower lobe predominance. 03:22 Lung function again shows restrictive changes of an impaired transfer factor, but in fact with hypersensitivity pneumonitis, it is often a mixed restrictive obstructive picture, not a pure restrictive picture which is what you get with pulmonary fibrosis. 03:34 When you do the CT scan, again, there's an upper lobe distribution. There's more ground glass that you normally get with pulmonary fibrosis, and you get some very specific changes of centrilobular nodules that's seen by this CT scan shown here on the right with some cyst formations, and mosaicism which is an evidence that there are small airways in infiltration and that is why you get a mixed restrictive obstructive defect, is that the disease doesn't just affect the alveoli but it also affects the small airways leading to some partial airways obstruction. Any invasive test such as bronchoscopy might reveal a lymphocytosis that we mentioned before. Transbronchial biopsies can identify the poorly formed granulomas, and then a blood test should be positive for the precipitin that causes the disease. So the avian precipitins should be present in somebody with Bird fancier's lung. Treatment of hypersensitivity pneumonitis, well, obviously, you need to stop the patient being exposed to the antigen. Now, that requires you having to identify the antigen and know what is causing it. And that is not always the case. In fact, it quite a significant minority of patient's with hypersensitivity pneumonitis, the antigen causing it has not been identified. 04:45 In addition, it is actually sometimes quite hard to convince patients to get rid of a favorite pet. If they got a parrot that is causing hypersensitivity pneumonitis, turning that they have to get rid of the parrot is quite tricky. Anti-inflammatory such as systemic corticosteroids are also probably quite useful in the hypersensitivity pneumonitis although there are not any particularly good data from clinical trials.
About the Lecture
The lecture Hypersensitivity Pneumonitis by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Interstitial Lung Disease (ILD).
Included Quiz Questions
Which of the following is suggestive of a diagnosis of pulmonary fibrosis over that of hypersensitivity pneumonitis?
- History of rheumatoid arthritis
- Upper-lobe rather than lower-lobe disease
- Positive avian precipitins blood test
- Centrilobular nodules on CT scan of the thorax
Which of the following occupations is NOT a commonly associated with hypersensitivity pneumonitis?
- Healthcare
- Bird breeding
- Agriculture
- Mushroom picking
- Feather quilt making
Which of the following describes the pathophysiology of hypersensitivity pneumonitis?
- Cell-mediated hypersensitivity to inhaled antigen
- Anaphylactic reaction
- Cytokine storm
- Endotoxin-mediated septic shock
- Idiopathic fibrosis
Which of the following is NOT an expected chronic histopathological feature of hypersensitivity pneumonitis?
- Neutrophils
- Poorly formed granulomas
- Mononuclear inflammatory infiltrate
- Peribronchial fibrosis
Which portions of the lungs are commonly involved in hypersensitivity pneumonitis?
- Upper lobes
- Lower lobes
- Middle lobes
- Basal subpleural area
- Pleura
Which of the following is NOT a CT finding of hypersensitivity pneumonitis?
- Bullae
- Ground-glass consolidation
- Centrilobular nodules
- Centrilobular cysts
- Mosaicism
What findings are seen on a bronchoalveolar lavage of patients with chronic hypersensitivity pneumonitis?
- Increase in lymphocytosis
- Increase in neutrophils
- Increase in macrophages
- Increase in mast cells
- Decrease in neutrophils
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |