Playlist
Show Playlist
Hide Playlist
Hyperprolactinemia
-
Slides AnteriorPituirary EndocrinePathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
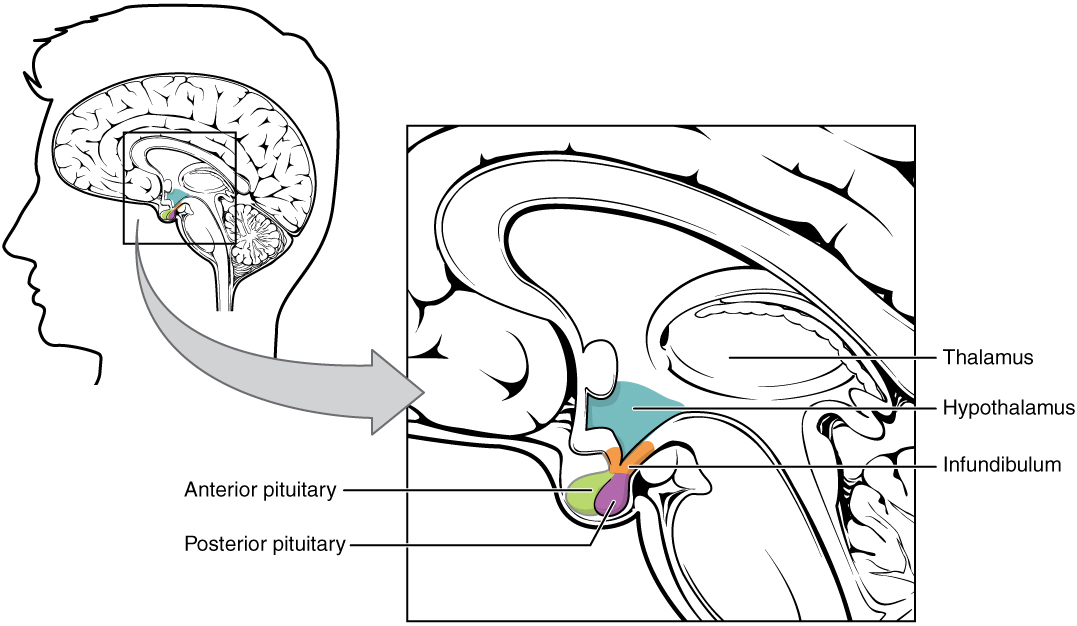
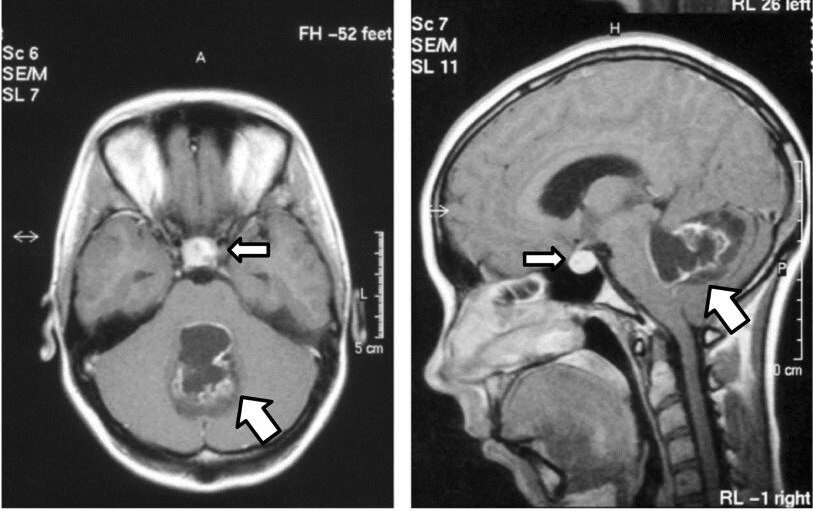
00:00 Let's talk about hyperprolactinemia and the different reasons as to why you might then develop this. 00:06 A functioning lactotrophic, remember that lactotrophic refers to something that promotes or stimulates the production of milk, like prolactin. hyperprolactinemia due to over expression, here you go. 00:17 If you haven't memorized already, we have a pituitary tumor transforming Gene PTTG. 00:24 Do not forget this why? Because a prolactinemia of all of the hormones that come out of a functioning adenoma and the anterior pituitary. 00:35 Prolactin is number 1, PTTG. 00:38 Another reason or another cause of hyperprolactinemia yet once again is primary hypothyroidism. 00:44 And the question that I get often times from students is well, why could this not be second or hypothyroidism? Well, technically perhaps, so you think if it was secondary hypothyroidism it means it my anterior pituitary decrease TSH. 01:04 And you would have increased TRH. 01:07 Thus increasing prolactin, one would think that there would be hyperprolactinemia. 01:11 However in primary hypothyroidism you have combined concerted effort but to your agent TSH. 01:20 Remember all these cells with an anterior pituitary mixed up and so therefore there's enough influence on that lactotroph to release prolactin. 01:31 Primary hypothyroidism. 01:35 What else may cause hyperprolactinemia? Whatever made them cause decrease dopamine influence on your lactotroph. 01:43 How? Damage to your dopaminergic neurons. 01:47 Drugs antipsychotics. 01:49 Remember schizophrenia means too much dopamine antipsychotics is the dopamine antagonists may result in hyperprolactinemia. 01:57 Look for galactorrhea in a female. 02:00 The stock section that we talked about earlier if the stock has been severed or lesion or you have a non-functioning at adenoma compressing the stock, you're not going to deliver dopamine effectively. 02:12 You will result in hyperprolactinemia or benign. 02:17 You might have a craniopharyngioma sometimes refer to in your cellar as being like crank oil and consistency. 02:25 May result in once again increased release or lack of release of dopamine or delivery. 02:32 Thus increased prolactin metastatic breast cancer. 02:36 Big one here. 02:37 In which once again, you're causing decreased deliver a dopamine thus what's my topic for this section hyperprolactinemia. 02:47 Do not forget about malignant metastatic breast cancer. 02:53 Genetics. we have something called PRLR mutation with the amino acid histidine to arginine at codon 18:8 or 188. 03:06 Whatever you want to think of it as PRL are as important histidine to Arginine. 03:13 Loss of Janus kinase to signal transduction and therefore resulting in you probably want to memorize, STAT5. 03:22 So up until this point you've probably have learned about Jack to stat. 03:28 Jack to stat is dealing with what we talked about earlier with WBC pathology, and we talked about myeloproliferative disorders. 03:38 Such as polycythemia Vera such as essential thrombocythemia. 03:44 Now this is Jack to STAT5. 03:48 Genes and genetics are huge in pathology nowadays. 03:54 What else may cause hyperprolactinemia but this time physiologically, how about nipple stimulation? Sure. 04:01 Stress exercise hyperprolactinemia estrogen binds the ER which in turn binds to irresponse elements. 04:12 What the heck does this mean? Okay, we walk you through this pregnancy. 04:19 Think about a pregnant lady. 04:20 How often is she running milk and down her nipple and very often at all. 04:26 My point is this, that estrogen may then block then release of milk from the breast this is during pregnancy. 04:38 What happens is that postpartum of a sudden estrogen levels drop the blockage on The receptors for prolactin has been lifted and therefore now the infant and the child newborn is ready to then breastfeed. 04:55 Decrease prolactin clearance includes chronic kidney injury or perhaps even a macro prolactin. 05:03 Chest wall trauma. 05:04 So there's a lot of things about the chest region that we've talked about in terms of interesting things. 05:10 Remember chest and ADH we dealt with quite a bit. 05:14 That we remember SATH. 05:16 We talk about lung cancer small cell of the lung. 05:20 We talked about chest trauma and I walk you through thoracic disease or excuse me, thoracic surgery. 05:28 And a lot of interesting things about the chest wall. 05:30 That seems to have a pretty direct effect on what's happening with hormonal levels. 05:35 Fascinating Here the serum prolactin concentration is much higher and most patients who have a lactotroph macroadenoma then in patients with any other cause of hyperprolactinemia. 05:51 So what this graph is then showing you? In great detail is the fact that hyperprolactinemia is my topic and of all the various causes of hyperprolactinemia that we walk through the highest levels of prolactin could be found in those patients that tend to have a macro adenoma. 06:17 The symptoms of hyperprolactinemia, premenopausal woman. 06:22 This would be where there would be headache, impaired vision, and amenorrhea, infertility, menstrual cycle dysfunction, there would be no ovulation and ambition of LH and FSH. 06:36 Why? Remember prolactin inhibits GnRH? No LH and FSH therefore you would not have or she would not have menses. 06:50 Amenorrhea secondary to hyperprolactinemia show a lower spine and forearm bone density. 07:00 Lumbar and forearm there seems to be an influence. 07:03 Once again we talked about this earlier with prolactin when compared to normal population with Menses. 07:10 So there's something here in terms of the balance of estrogen that has been lost with prolactin look for lower bone density in the spine lower spine, especially in the forearm and with all this prolactin you will for sure have galactorrhea. 07:28 So even though might seem as though that the female is fertile. 07:34 She's not she's amenorrhea, to amenorrhea-galactorrhic. 07:41 This is called hypogonadotropic hypogonadism. 07:46 Was that even mean? Watch. 07:51 If it's a male or female. 07:53 The gonad would be testes ovary respectively. 08:00 That is not functioning. 08:02 Why? There was no disease in the ovaries and testes were there and hyperprolactinemia. 08:10 No. 08:12 So that high level prolactin is not affecting the gonad directly but it's affecting whom? The hypothalamus. 08:22 Thus the anterior pituitary. 08:25 That axis of the hypothalamus and the pituitary is called it's called gonadotropic. 08:33 In hyperprolactinemia, how much GnRH and how much LH and FSH do you have? Not much. 08:42 So my hypogonadism is caused by hypogonadotropic. 08:49 Thus we call this hypogonadotropic hypogonadism the board's love this kind of questions. 08:56 They love this type of concept in which you have to constantly think through what's occurring. 09:03 This is a secondary hypogonadism. 09:08 Secondary hypogonadism not primary. 09:12 Erectile dysfunction, decreased libido, infertility, rarely galactorrhea. 09:18 This is a male on the right, and this the Greek symbol for a male. 09:22 Notice here we are not putting in amenorrhea since we're from to a male. 09:28 The previous section was the Greek symbol for a female. 09:35 The topic is hyperprolactinemia and let me assure you you don't need a microscope to see the flow chart. 09:41 I am going to walk you through this in great detail amplifying the left branch of the flowchart the middle branch in the right branch. 09:51 Now these are all different causes or manners in which you may have increased prolactin activity and what your steps of management would be. 10:02 For example, you want to check to see as to whether or not there's a pregnancy going on with the lady. 10:09 You might want to check for beta HCG. 10:11 Later on there will be other organs that will take a look at and those also will include the thyroid gland and to pituitary and so forth. 10:19 And as I said, our first order business now is going to go right through the middle to make sure that we clear this once and for all as to why we can say that there is hyperprolactinemia. 10:32 In terms of how the patients behaving, in a patient that has primary hypothyroidism. 10:39 Now if that is news to you, it shouldn't be or about time you practice. 10:43 It won't be because we have cleared it here and you'll know exactly why your patient is presenting a such. 10:49 Again, So we'll take a look at this right side of the branch and on the right side the branch of the algorithm will be focusing on the middle branch. 11:00 And the middle branch it is referring to thyroid disease and how this is associated with heightened levels of prolactin activity. 11:09 The patient comes in and has secondary amenorrhea. 11:13 The reason that's important for us is because if you're suspecting hyperprolactinemia you do know that prolactin has what kind of effect on the GnRH from the anterior pituitary, Excuse me from the hypothalamus. 11:25 Inhibitory good. 11:27 So anytime that you have increased levels of prolactin then generate just dropped. 11:31 Obviously LH and FSH will be dropped from the anterior pituitary. 11:35 What a secondary amenorrhea approximately three months in a lady's reproductive life span. 11:41 She may not be having menses. 11:44 Now you're thinking pregnancy being one of the most common causes of secondary memory amenorrhea. 11:50 Come back to see that the pregnancy test and beta HCG is negative. 11:55 Next you're going to check for TSH and prolactin levels. 12:00 Fascinating watch this. 12:03 They find that the TSH levels are high. 12:07 And you find that the patient is suffering from right a cardiac constipation, lack of menses. 12:12 Amenorrhea secondary type. 12:15 And also has let's say cold intolerance and gaining quite of bit of weight. 12:21 That definitely sounds like what kind of hypothyroidism? Primary secondary tertiary, especially if I give you elevated levels of TSH, please. 12:30 Good primary, correct! And in primary hypothyroidism, you have the symptoms that I just gave you and you find elevated levels of TSH. 12:40 Not only would you find elevated levels of TSH now this is where you want to pay attention here by chemically so that you understand the pathology and the patient walking through the door. 12:49 Not only would you find elevated levels of TSH but you would also find elevated levels of TRH. 12:54 Thyroid releasing hormone. 12:56 I've only mentioned here TSH because that is the best screening test for thyroid disease. 13:03 But to understand the full scope of what's going on here is that in the patient to as hypothyroidism and has hyperprolactin type of activity or item prolactin activity amazingly listen, please. 13:16 That increase in TRH from the hypothalamus it will then act upon the anterior pituitary, and not only could have been cause hyperplasia of the paratroops. 13:27 It could potentially cause well increase activity lactatrops. 13:32 But that will have nothing to do with prolactinoma, be careful there. 13:36 Well TSH is increased and it is technically the TRH, which made them cause hyperplasia of the lactotroph the TRH really increases the activity of serum prolactin giving you the increased prolactin type of activity in your patient, and your patient is walking through the door and she might be lets say 32 years of age reproductive life span, and she might be complaining of no menses or let's say two months. 14:08 Now you check her beta-HCG negative. 14:14 You check her TSH within normal limits. 14:19 She is 27 years of age. 14:22 She's not having menses. 14:25 Now what you going to do? Well, now you're thinking about prolactin. 14:29 If you're thinking about prolactin and you find that to be increased, now what I need you to do always in pathology is understand the concept first, then you memorize the value not the other way around because you'll be wasting precious time. 14:47 You're checking for secondary amenorrhea and beta-HCG is negative and you find your TSH to be within normal limits. 14:54 Now you find your prolactin to be elevated. 14:55 Now if you want memorize greater than 100 nanograms per milliliter. 15:02 So now, you know this prolactin that's to be elevated and then you do an MRI next up a management. 15:08 So I just walk you through three steps management for secondary amenorrhea and when you would perhaps even think about using prolactin or hyperprolactinemia in a case of a female who is not having menses. 15:23 First step, beta-HCG. Second step, TSH. 15:27 Third step, prolactin elevated, and next step of management. 15:33 MRI of the head, where you going to find perhaps he find a tumor you find a functioning tumor that is then causing perhaps what else maybe and maybe they'll be nice. 15:44 They usually are, trust me. 15:47 And I'll give you visual disturbances maybe headache but it isn't it interesting that sometimes we read a stem of a question and this the critical information goes right by you goes over your head and then you start figuring things out and you go back to stem and oh my goodness. 16:01 You know, you start seeing the light. 16:04 So the more that you're exposed to your clinical presentations the more you'll know just what to look for and what to pick out of the stems of your question. 16:12 This is the evolution of your boards as I clear. 16:16 It is very much a thinking exam. 16:20 That's why things have dropped down to 44 questions per block now. 16:25 Was 52 once upon a time then 46, now it's 44, evolution of the exam. 16:31 You need be able to think through I'm helping you to do that. 16:34 Let's continue. 16:36 Now if that doesn't happen, then you consider other causes but for right now that's good enough somewhere along the line of what I walk you through, you would find the answer the pitfalls, the hook effect and macro prolactin and what that means following is the following every. 16:52 Once in a while now always ask yourself this question, this adenoma that I'm finding this adenoma that I'm finding within the within the pituitary. 17:03 Is a functioning or non-functioning adenoma? Always ask yourself that question. 17:08 So evaluation of prolactin and you find that to be greater than 20 nanograms and at that point, maybe two macro prolactin history of pregnancy, meds, headaches, renal disease will be all part of course your hyperprolactinemia workup. 17:25 MRI the pituitary me revealed adenoma that we talked about. 17:28 Large non secretin adenoma can elevate prolactin via stock compression, we talked about that earlier. 17:34 Therefore inhibiting the release or delivery of dopamine to the end to pituitary. 17:39 And so therefore you might find elevated levels of prolactin. 17:42 So when you say non-functioning remember, non-functioning meaning that you might disrupt or inhibit the release of many other enter pituitary hormones, but you might cause inhibition of dopamine delivery and therefore increased levels of prolactin. 18:01 Hyperprolactinemia, first line. 18:03 Well, if there's too much prolactin and you want to try to slow it down, you've ordered drugs such as bromocriptine or cabergoline. 18:11 This is a dopamine agonist. 18:13 And so therefore you are exogenously mimicking the action of endogenous dopamine. 18:20 Indications, inhibition of prolactin secretion and amenorrhea galactorrea, prolactin secreting tumors correction of female infertility secondary to hyperprolactinemia. 18:30 So these are indications in which you're thinking about giving your dopamine and a lot of these already talked about. 18:38 If the medications do not work, then you start getting into transsphenoidal surgery, post-operative radiation therapy to prevent regrowth residual but we got a couple of things here. 18:51 Transsphenoidal bulking of lactatroph adenoma that are resitant to cabergoline and recur after surgery, now the only problem is this That anytime that you're even thinking about giving a patient exposing a patient to radiation, initially there might be a hyper functioning of that particular organ. 19:11 But if radiation is given abundantly or the tissue so sensitive that the radiation kills off the tissue excessively, you might and look for this often times go from hyper to hypo, we can say the same thing about graves disease of the thyroid. 19:29 That's something that you have seen over and over again. 19:32 You have heard of radio blade of therapy, upon treatment with radiation, you are destroying excess of thyroid tissue going from graves disease to hypothyroidism, the same kind of issue might be taking place in other organs including the anterior pituitary. 19:52 In order we talked about drugs transfer auto, last resort, maybe post-operative radiation.
About the Lecture
The lecture Hyperprolactinemia by Carlo Raj, MD is from the course Pituitary Gland Disorders.
Included Quiz Questions
Overexpression of pituitary tumor transforming gene is more closely associated with which of the following?
- Prolactinoma
- Primary hyperthyroidism
- Sheehan's syndrome
- Non-functioning lactotrophic adenoma
- Lymphocytic hypophysitis
All EXCEPT which of the following can cause decreased dopaminergic inhibition of prolactin secretion?
- Primary hyperthyroidism
- Damage to hypothalamic dopaminergic neurons
- Selective serotonin reuptake inhibitors
- Severed pituitary stalk
- Craniopharyngioma
Serum prolactin levels are highest in patients with which of the following?
- Lactotroph macroadenoma
- Metastatic breast cancer
- Prolactin receptor mutation
- Chronic kidney disease
- Primary hyperthyroidism
Premenopausal women with hyperprolactinemia will show all EXCEPT which of the following symptoms?
- Increased ovulation
- Amenorrhea
- Infertility
- Decreased bone density in the lumbar spine
- Galactorrhea
In the treatment of hyperprolactinemia, bromocriptine acts as which of the following?
- A dopamine agonist
- A dopamine antagonist
- A prolactin receptor agonist
- A prolactin receptor antagonist
- Bromocriptine is not used in the treatment of hyperprolactinemia.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Great walk through, the concepts are easy to understand and apply.