Playlist
Show Playlist
Hide Playlist
Hyperkalemia: Treatment
-
Emergency Medicine Bord Hyperkalemia.pdf
-
Download Lecture Overview
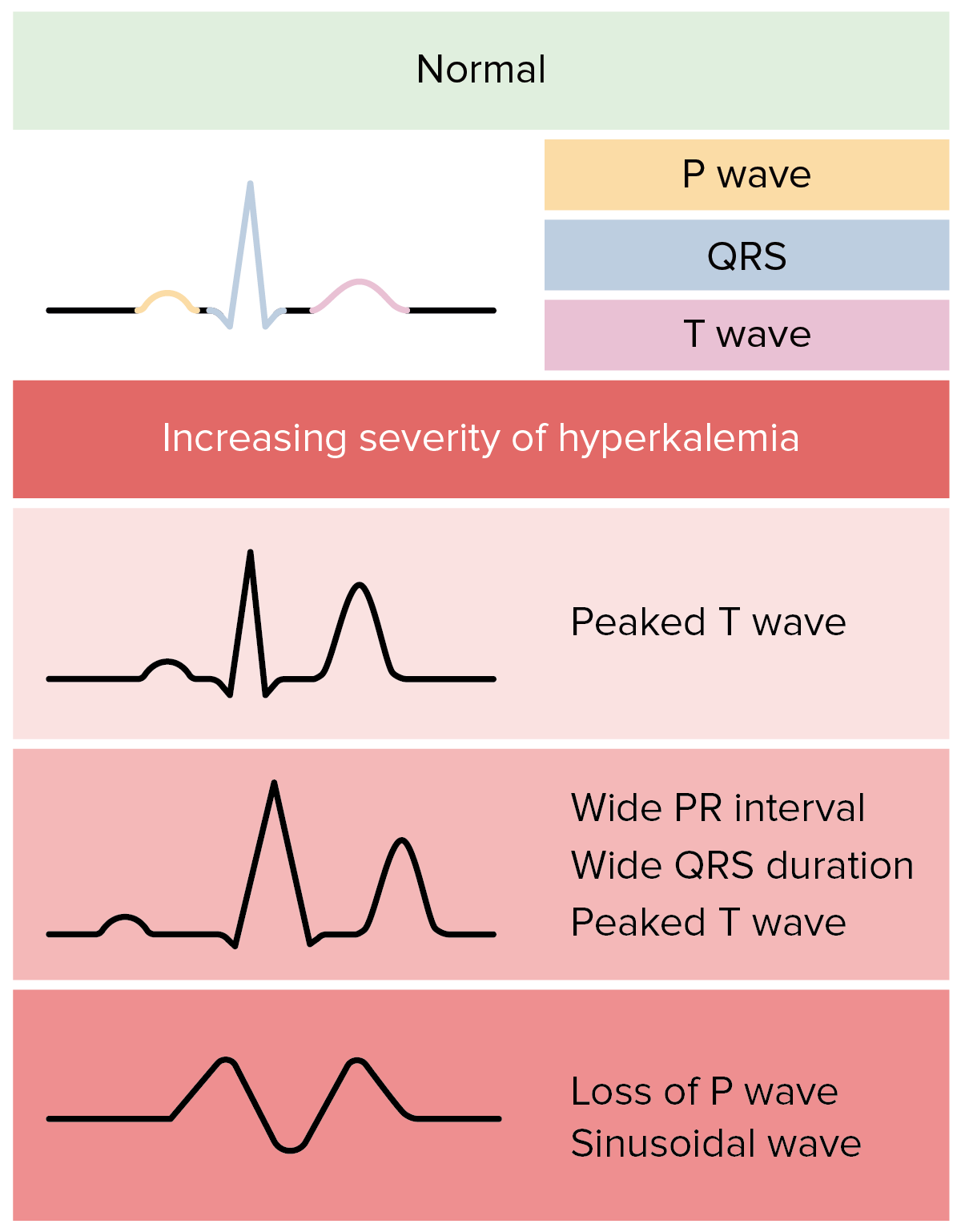
00:01 So what are our treatment steps? The first step is IV calcium. 00:06 Now, you do that when you see those EKG changes. 00:09 It’s debatable about whether or not you would do it for just the peaked T waves or whether you would wait for there to be further EKG findings, I personally am in the camp that I treat with any EKG changes but other emergency medicine physicians may wait to treat until there’s additional EKG changes. 00:28 What potassium is doing is it’s stabilizing the cardiac membrane. 00:31 So you’re preventing then those further EKG changes from happening and the patient from developing cardiac arrest. 00:38 The effects here last about 30 to 60 minutes, and the dose is one amp of calcium chloride or three amps of calcium gluconate. 00:47 Now, a few tips here. 00:49 Calcium chloride can be very caustic and toxic to the veins. 00:53 So, generally, we reserve calcium chloride for treatment of patients who are in cardiac arrest or who are near cardiac arrest. 01:00 Calcium gluconate is not caustic to the veins, but you have to give twice as much. 01:05 So we reserve calcium gluconate for patients who are not coding. 01:09 So we’ve gone ahead and we’ve given our calcium because that is the first most important step when the patient has EKG changes. 01:18 Next, we wanna move the potassium intracellularly. 01:21 So we talked about the fact that potassium mainly lives in the cell and a lot of the things that cause potassium to have elevated levels are things that shifted out of the cell. 01:32 So we wanna get it back in the cell, push it back in there. 01:35 What are the things we can do to push the potassium back in the cell? So the first is insulin and D50. 01:42 So you wanna administer the insulin IV. 01:44 Sometimes you’re gonna give your insulin subcutaneously. 01:47 But in this situation, you wanna give it IV because you want it to work right away. 01:50 Generally, you give about 0.1 units per kilogram of insulin or between 7 and 10 units of insulin. 01:58 You’re gonna give the D50 at the same time because you wanna prevent hypoglycemia. 02:03 So D50 is a 50% concentrated glucose solution. 02:07 So unless a patient has a very elevated blood sugar, you’re gonna wanna make sure that you give these two together. 02:14 Additionally, you’re gonna wanna give the D50 first and the reason that you do that is because if you give the insulin and then, you’re not able to get an IV line in your patient, you’re gonna be stuck potentially with a hypoglycemic patient. 02:27 So we generally will give the glucose containing solution first, then give the insulin after that. 02:34 You can also give a beta 2 agonist. 02:37 So you can give nebulized albuterol. 02:39 It’s a higher dose than what’s given for bronchodilation in a patient who has asthma, but beta 2 agonist can be of some benefit. 02:47 You’re gonna give it to your patient on a continuous snap at a higher dose than what you normally use. 02:53 Other things that can help the potassium go into the cell would be saline infusion. 02:58 You wanna be very careful in patients who have renal failure, patients who don’t make urine, because you could potentially volume overload them. 03:05 So if you give them a large saline load and they’re not able to urinate that out, that’s a patient that potentially may run into issues. 03:12 And lastly, you can give bicarbonate for patients who are very acidotic. 03:18 So their pH is low. 03:20 You can give bicarbonate and that will also help shift the potassium into the cells. 03:25 It does so via the mechanism of the potassium hydrogen exchange channels. 03:30 And then, we’re gonna talk about potassium excretion. 03:34 So we’ve stabilized the cardiac membrane. 03:36 We’ve pushed the potassium into the cell, and then, we wanna think of ways to get our body totally rid of the potassium. 03:43 So to have it go away. 03:44 So hemodialysis is most effective. 03:48 It’s the most effective way to get rid of potassium in patients especially who are chronically on dialysis. 03:54 We oftentimes reserve this for critically ill patients but this is one of the indications for emergent dialysis. 04:01 This is an indication where you call your nephrology consult and say I have a patient who emergently need dialysis. 04:09 Definitely, for a patient who doesn’t make urine, this was gonna be a key element of treatment of hyperkalemia. 04:16 Lasix is another possible option here. 04:19 So Lasix acts on the kidney as a diuretic and different than spironolactone, Lasix helps excrete the potassium. 04:27 It helps the potassium go away. 04:29 Lasix use is actually one of the reasons that patients may develop hypokalemia or low potassium levels. 04:35 What can be most helpful in tumor lysis or rhabdomyolysis but definitely something to consider when we’re trying to get our body total rid of potassium. 04:45 Again, you wanna make sure that your patient can make urine. 04:47 So if you’re treating a patient with furosemide, you wanna make sure that they’re gonna be able to urinate. 04:52 And lactulose or cation exchange resins are the other choice. 04:57 Now, these help patients excrete potassium in a bowel movement. 05:00 You wanna beware of Kayexalate which is a cation exchange resin in patients with renal failure, and that’s because it’s been shown to be associated with bowel ischemia in patients who have renal failure and patients who are on dialysis. 05:13 So for those patients, you would be more likely to use the lactulose rather than the Kayexalate. 05:19 Sodium zirconium cyclosilicate is another agent which may be used instead of Kayexelate for similar indications. 05:29 It’s important to remember that this does not take effect for almost over four hours because it has to make its way through the gut and then it has to cause the patient to have a bowel movement. 05:38 So it’s not gonna be a quick fix. 05:41 It’s not gonna be a quick fix like dialysis will lower it acutely, but it is something that you can give especially for the longer term, for 4 or 6 hours down the line. 06:03 So the conclusion here is that elevated potassium levels require emergent treatment. 06:07 It can have severe cardiac effects and as the level gets higher and higher, those effects can be greater and greater. 06:15 Causes of hyperkalemia are renal failure, breakdown of cells, medications or acidosis, and then hemolysis. 06:23 So if those cells break down when they’re on their way to the lab or when the blood is being drawn can lead to spuriously elevated results. 06:31 So if you get a result that doesn’t make sense, go ahead and resend that lab test. 06:35 The first test you should get is that EKG if there’s concern for hyperkalemia. 06:39 The findings start out with peaked T waves, all the way to sine wave, and ultimately, cardiac arrest and PEA arrest. 06:48 For cardiac membrane stabilization, go ahead and give calcium first. 06:51 Then, you wanna shift the potassium intracellularly and then, start thinking down the line for increasing potassium excretion.
About the Lecture
The lecture Hyperkalemia: Treatment by Sharon Bord, MD is from the course Endocrine and Electrolyte Emergencies. It contains the following chapters:
- Hyperkalemia: Treatment Steps
- Conclusion
Included Quiz Questions
In patients with EKG changes secondary to hyperkalemia, what is the first-line medication administered?
- IV Calcium
- IV glucose
- Insulin bolus
- Amiodarone
- Adequate IV fluids
Which of the following medications that shift potassium intracellularly is given to patients who are severely acidotic?
- Bicarbonate
- Saline infusion
- Albuterol nebulization
- IV insulin + D50
- SQ insulin
What is the most effective way to decrease potassium?
- Hemodialysis
- Furosemide
- Lactulose
- Kayexalate
- IV insulin + D50
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |