Playlist
Show Playlist
Hide Playlist
Hyperkalemia: Etiology & ECG
-
Emergency Medicine Bord Hyperkalemia.pdf
-
Download Lecture Overview
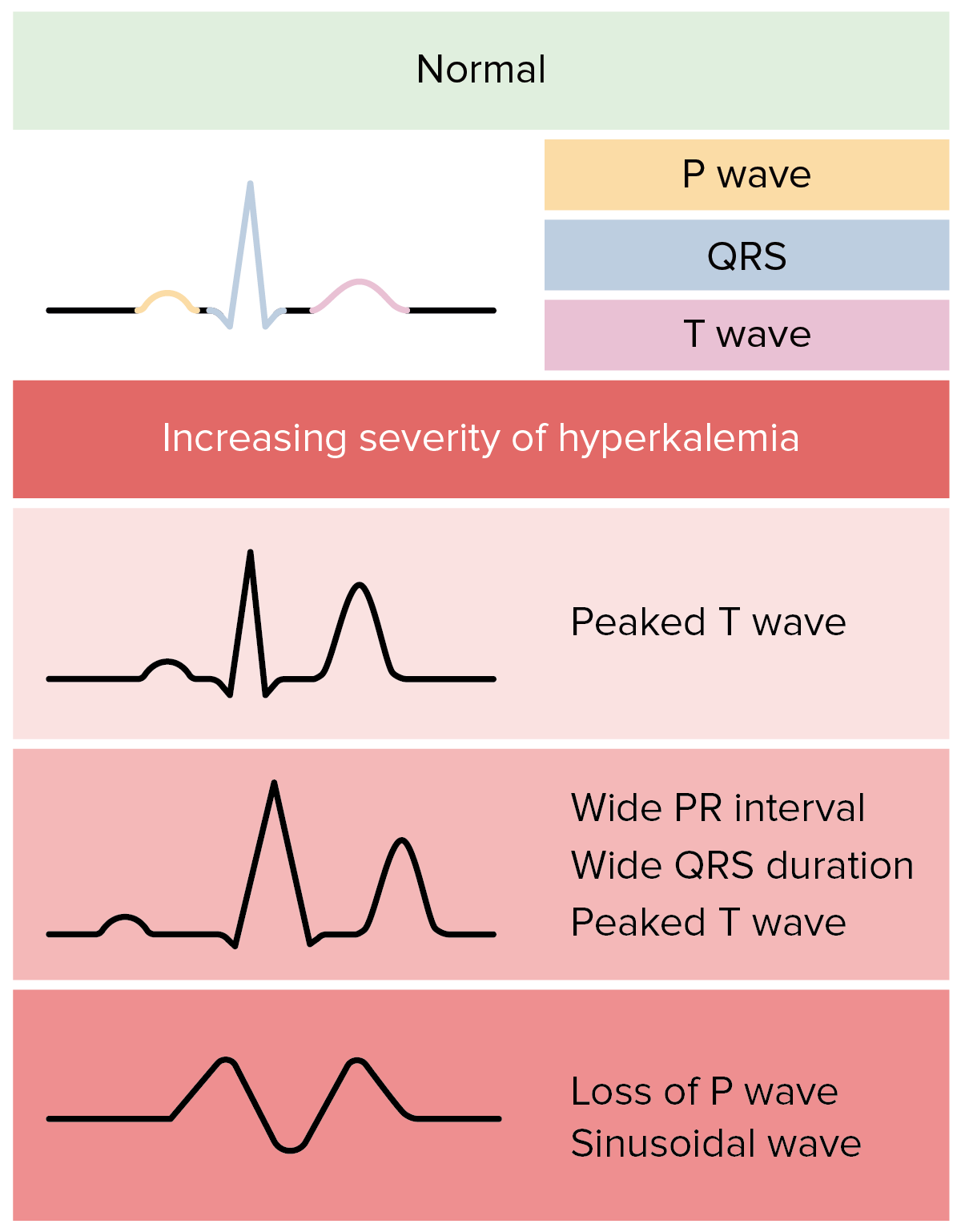
00:01 Hi, we’re gonna be talking about hyperkalemia and specifically, how to diagnose and manage hyperkalemia in the Emergency Department. 00:09 So let’s first start by talking about hyperkalemia and potassium in general. 00:16 So normal potassium levels are between 3.5 and 5. 00:19 Potassium is an interesting cation because it lives mostly intracellularly. 00:26 So when there’s too much potassium outside of the cell, that makes us concerned that issues could develop for the patient. 00:33 So mild hyperkalemia is between 5.5 and 6. 00:37 Moderate hyperkalemia is defined as 6.1 to 6.9. 00:42 And then, severe hyperkalemia is greater than seven. 00:46 Now, I wanna stress that this is a most dangerous electrolyte abnormality. 00:51 That’s not to say that having a low sodium or an elevated sodium, or a low glucose isn’t important. 00:57 Those things are definitely important to know how to treat and manage, and diagnose, but this electrolyte abnormality specifically can lead to dangerous cardiac side effects. 01:07 So when thinking about hyperkalemia, potassium is mainly regulated by the kidney. 01:13 So the normal value like I had mentioned is between 3.5 and 5 and it mainly lives in the cell. 01:19 The reason that it’s important to know that it’s mainly regulated by the kidney is because in patients who have a history of kidney failure or who are on kidney dialysis are at increased risk of getting elevated potassium levels. 01:33 There also can be cardiotoxicity. 01:37 So as the levels continue to rise, patients can get arrhythmias and cardiac arrest. 01:43 And if you think back to PEA, pulseless electrical activity, this is one of the H’s and the T’s. 01:49 Hyperkalemia is one of the H’s. 01:51 There’s also increased membrane excitability. 01:54 Now, beware of hyperkalemia in patients with known renal insufficiency or who are on dialysis. 02:02 Always ask about missed dialysis sessions. 02:05 Patients sometimes don’t go to dialysis for a variety of reasons. 02:09 They’re not able to get their ride there, they’re not able to – they don’t feel well, so they’re not able to go to their appointment. 02:15 There’s a variety of reasons that patients might not go. 02:18 They may go and then when they get there, they might have an issue with their fistula or with their dialysis catheter. 02:24 Definitely make sure you’re asking people whether or not they missed any sessions. 02:28 The other part of this is you can ask people if they had to have their session cut short for any reason. 02:33 Sometimes if the blood pressure gets low or they get a little temperature, the dialysis people will stop the session before it’s fully, fully completed and that in the end can also lead to elevated potassium levels. 02:45 So one of the main reasons that patients get elevated potassium is renal failure. 02:49 So are their kidneys failing acutely or are they on hemodialysis? Other etiologies are rhabdomyolysis or cell breakdown. 02:57 So anything that causes rupture of cells can lead to an elevated potassium level and the reason for that is because patients have potassium that lives mainly within the cell. 03:08 Rhabdomyolysis can develop if someone has a very vigorous workout or after they run a marathon, and that can in turn lead to the potassium levels becoming elevated. 03:18 There are also certain drugs that are associated with elevated potassium level. 03:23 One of them is spironolactone. 03:25 So this is a diuretic that reabsorbs the potassium from the kidney. 03:30 So by reabsorbing the potassium from the kidney, if that happens in too great of a quantity, the levels become elevated. 03:37 Beta blockers can increase potassium levels. 03:41 ACE inhibitors or Angiotensin Receptor Blockers can increase potassium levels due to the effects they have on the kidney. 03:48 And then lastly, potassium supplementation. 03:51 So some patients are chronically deplete of potassium and for those patients, their doctor may prescribe them potassium supplementation. 03:59 That they take a vitamin at home that contains potassium. 04:03 Now, every so often, if the balance gets a little bit out of whack, that patient can then get elevated potassium levels. 04:10 So it’s almost like an iatrogenic thing that happens. 04:13 That we prescribe the medication which then leads to the potassium levels being elevated. 04:18 Acidosis can also cause the potassium to increase. 04:22 The reason for that is because on the surface of cells, there’s a potassium hydrogen exchange channel. 04:28 As the body develops acidosis, it tries to protect itself. 04:32 So it takes the hydrogen ions and puts them into the cell and takes the potassium ion and puts it out of the cell. 04:39 So the body is trying to protect itself from the hydrogen ion, from the acidosis that’s developing and by doing so, it in turn creates an elevation of the potassium. 04:49 And lastly, it can be a spurious reading or lab hemolysis. 04:53 So when we send blood to the lab, they run it on a machine. 04:57 Every so often, what happens when the blood is drawn and sent to the lab is there can be breakdown of those cells within the tube, when the blood was being drawn, or after the fact. 05:08 And when there’s hemolysis or breakdown of those cells, the potassium will appear to be elevated on the labs. 05:15 So if you get a lab value from the lab that seems just totally out of whack. 05:19 They call you and they say the potassium is 8 and the patient looks great, and they don’t have any changes on their EKG, and no other reasoning for thinking that the potassium should be 8, go ahead and resend that lab. 05:32 It’s possible that it’s due to lab error. 05:34 The EKG is the first test you’re gonna wanna get for patients with elevated potassium or in whom you are concerned about elevated potassium. 05:45 So for example, you’ll wanna get this test when the patient comes in before you even send off the blood work or while you’re sending off the blood work especially in a patient with a good story for elevated potassium. 05:56 So for example, a patient who’s missed dialysis, who’s having palpitations, whose heart rate is slow. 06:02 You’ll wanna get that EKG very early because the EKG can give you clues as to what the potassium level is. 06:09 So as the potassium levels rise, you initially start by getting peaked T waves, then a flattened p wave and a prolonged PR interval. 06:19 Then, the QRS complex will widen, and then the EKG develops into sine wave, and then eventually, cardiac arrest. 06:27 This is in a lecture specifically on EKG’s but I’ll show you a couple of examples so you know a little bit what to look for. 06:33 So here’s the EKG with that peaked T wave. 06:37 So the arrow is pointing to one of the peaked T waves but you could see that the T waves all across the precordium. 06:43 So in V2, V3, V4, V5, V6 all are peaked. 06:47 We always say that you get concerned about a peaked T wave being related to hyperkalemia if it’s pointy at the top. 06:53 So we always say if it would hurt to sit on it, that’s when you get concerned about hyperkalemia. 06:58 So you could see here, that would probably hurt to sit on. 07:01 It’s a really pointy top of that peaked T wave. 07:03 It can be very helpful also to compare the EKG to a prior EKG. 07:08 So it’s possible that that’s what the patient’s EKG looked like in the past, but if you don’t have one to compare it to or it’s different than a prior, that’s hyperkalemia. 07:19 That’s a classic EKG finding for early hyperkalemia. 07:23 Moving along, as the potassium levels continue to increase, here the QRS complex is wider. 07:31 So normally, the QRS complex should be less than 120 milliseconds and here, it’s a wider QRS complex. 07:38 So we’re getting further down the line in our EKG findings that we’ll see as the potassium levels rise. 07:45 Again, here, you can also see some element of peaked T waves. 07:48 In the right person with the right story, you start treatment immediately when you see this EKG.
About the Lecture
The lecture Hyperkalemia: Etiology & ECG by Sharon Bord, MD is from the course Endocrine and Electrolyte Emergencies. It contains the following chapters:
- Hyperkalemia
- Hyperkalemia: Etiology
- Hyperkalemia: EKG
Included Quiz Questions
What is the most dangerous electrolyte abnormality due to its cardiac side effects?
- Hyperkalemia
- Hyponatremia
- Hypokalemia
- Hypernatremia
- Hypomagnesemia
What drug causes hyperkalemia due to reabsorption of potassium in the kidney?
- Spironolactone
- Beta-blockers
- ACE inhibitors
- Angiotensin receptor blockers
- Potassium supplements
What is the first test that must be done in a patient noted to have hyperkalemia?
- Electrocardiogram
- Serum glucose level
- Venous blood gas
- Oxygen saturation
- Electrolyte panel
Which among the following is not an expected EKG finding in hyperkalemia?
- J wave
- Peaked T-waves
- Widened QRS
- Prolonged PR interval
- Flattened P wave
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I really like Dr. Bord's explanation and back to basics review added here and there. I really like her explanation of the progression of changes you would see on an ekg.
Clear, succinct, and practical. Thanks for the lecture Dr Bord!
It’s very useful information. Thank you. I’ll use the knowledge from this video for applying with my real work and it is beneficial for my patients.