Playlist
Show Playlist
Hide Playlist
Hypercalcemia: Types and Management
-
Slides Calcium Metabolis.pdf
-
Reference List Endocrinology.pdf
-
Reference List Metabolic Bone Disorders.pdf
-
Download Lecture Overview
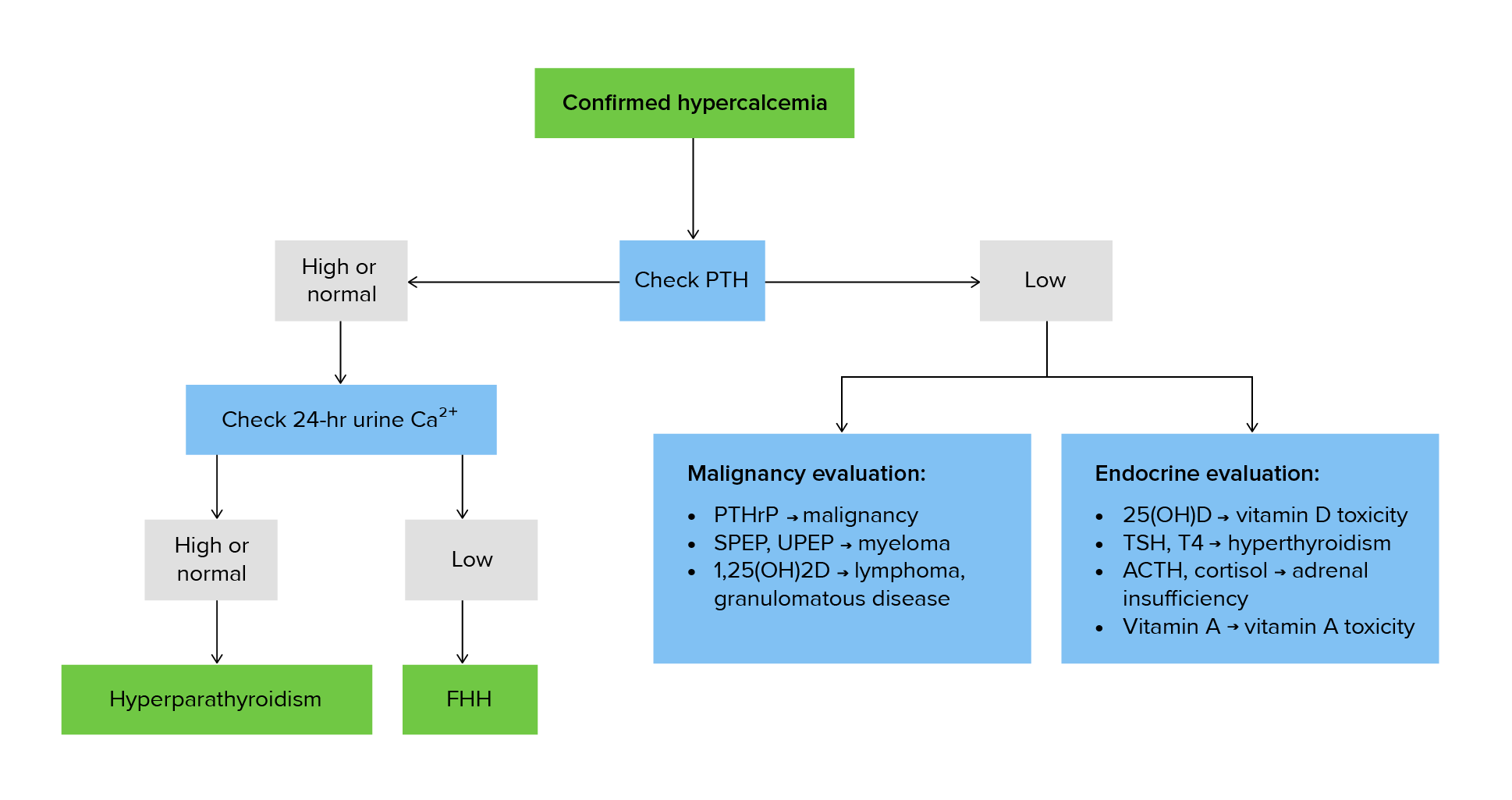
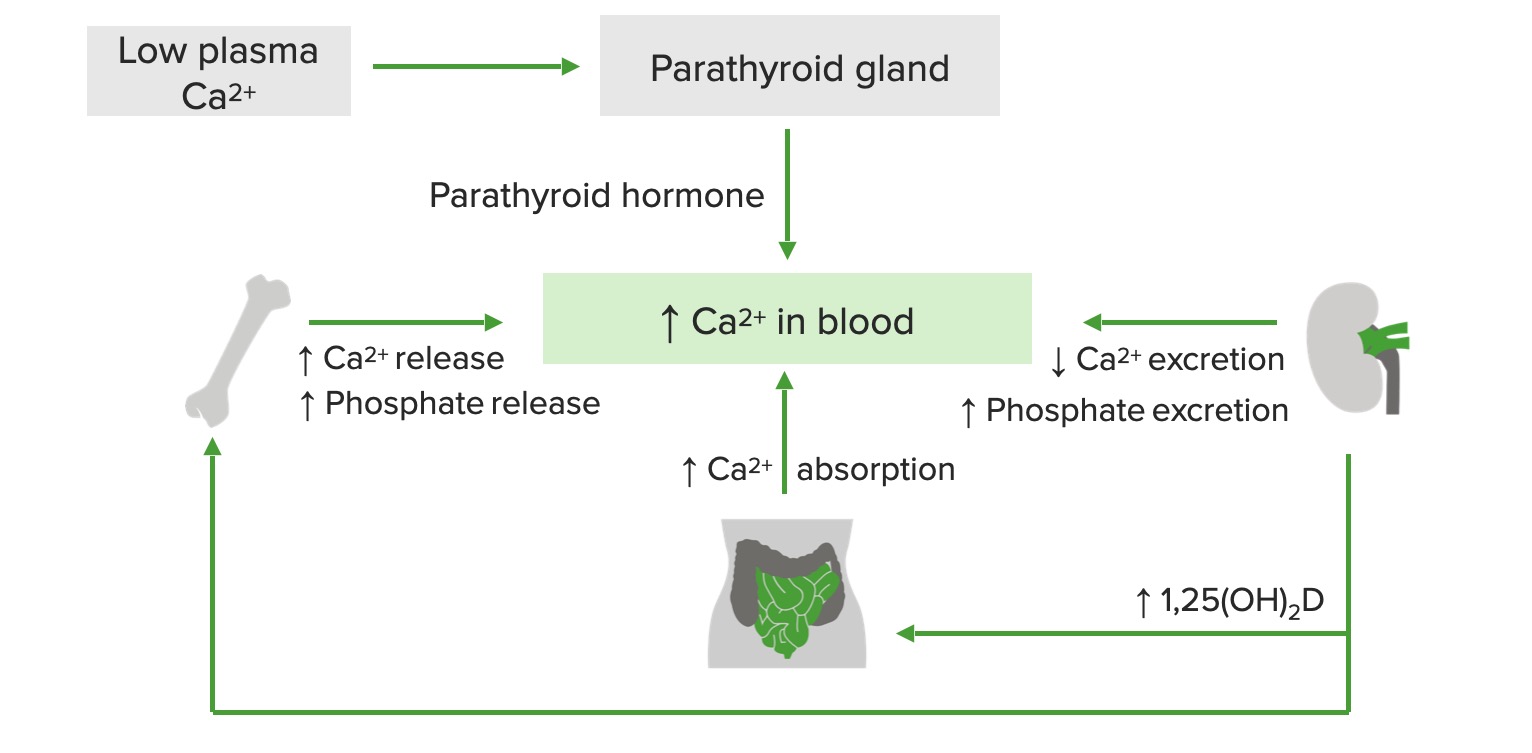
00:01 Malignancy associated hypercalcemia is the most common cause of non-parathyroid hormone induced hypercalcemia. 00:08 It is typically severe in that patients present with elevated calcium greater than 14 mg/dL. 00:16 It's often the result of a tumor-produced PTH-related protein or PTHrP leading to extensive resorption of the bone. 00:24 Renal carcinoma, breast cancer and squamous cell cancers are associated with PTHrP release. 00:32 Rarely, local mediated osteolysis from its extensive skeletal metastases, typically in multiple myeloma and breast cancer may cause the efflux of calcium from bone resulting in significant hypercalcemia. 00:46 Let's talk about the management of hypercalcemia. 00:49 This is really dependent on the severity of the elevation of calcium. 00:53 If it is mild, say under 12 mg/dL, treatment of the underlying disorder, for example, hyperparathyroidism, once you perform a parathyroidectomy. 01:04 This is usually sufficient and continuous monitoring of patient's calcium continuous after to surgery. 01:11 Treating calcium levels above 12 mg/dL usually requires hospitalization especially if patient's asymptomatic. 01:19 The key features to look at for are the presence of kidney disease and mental status changes. 01:25 Initial treatment of severe hypercalcemia consist of aggressive hydration to replete volume loss and to increase the kidney's excretion of calcium. 01:35 Loop diuretics are not recommended unless the patient manifest with kidney failure or heart failure. 01:42 For the acutely symptomatic patient, subcutaneous calcitonin should be applied as well. 01:49 Bear in mind that the half-life of the drug wanes withing 48 hours Calcium levels should be re-checked and re-dosing may be considered. 01:57 Long-term management of hypercalcemia may require intravenous bisphosphonate therapy to prevent mobilization of calcium from the skeleton but also requires adequate kidney function. 02:08 Always check the creatinine before prescribing a bisphosphonate. 02:13 Glucocorticoids and restriction of calcium and vitamin D intake are also beneficial in vitamin D dependent hypercalcemia. 02:22 Hemodialysis is reserved for the treatment of severe hypercalcemia in patients who are unable to produce urine and would not respond to fluid resuscitation or diuretics. 02:33 Vitamin D-dependent hypercalcemia is associated with normal to elevated serum phosphorus. 02:39 Vitamin D enhances intestinal absorption of phosphorus and suppresses PTH secretion which reduces kidney phosphorus excretion. 02:49 This is in fact, the opposite in hyperparathyroidism where one sees reductions in serum phosphorus. 02:58 In vitamin D-dependent hypercalcemia, the pathophysiology going on is the unregulated conversion of 25-hydroxyvitamin D to 1,25-dihydroxyvitamin D. 03:10 This is seen classically in the granulomatous diseases which include: fungal infections, tuberculosis, sarcoid and lymphomas. 03:20 What occurs is increased intestinal absorption of calcium. 03:24 Patients present with hypercalcemia. 03:28 These conditions are associated with inappropriately normal or frankly elevated 1,25-dihydroxyvitamin D level and a supressed PTH. 03:39 Decreased serum and urine calcium after intake of calcium and vitamin D is restricted. 03:45 Or rapid decrease in calcium after glucocorticoid therapy is consistent with these disorders. 03:52 Of note here that the treatment of hypercalcemia and sarcoidosis is to give steroids. 03:58 Let's talk about medication-induced hypercalcemia. 04:02 PTH mediated hypercalcemia occurs with lithium. 04:06 Non-PTH mediated hypercalcemia occurs with thiazide diuretics, classically. 04:12 And then excessive ingestion of calcium or vitamin D can also elevate serum calcium levels and should always be ruled out on history. 04:22 Let's go through a summary of the causes of hypercalcemia that we've discussed. 04:26 Primary hyperparathyroidism most commonly from a parathyroid adenoma is the most common cause of outpatient hypercalcemia. 04:37 In this case, the PTH is elevated in 80%, the phosphorus is classically low and the vitamin D levels are high. 04:44 Creatinine is usually normal and the parathyroid hormone releasing peptide is negative. 04:50 Clinical clues are symptoms and signs of hypercalcemia and xrays which are classic findings including osteitis fibrosa cystica. 04:59 Humeral hypercalcemia of malignancy is the most common cause if in-patient hypercalcemia. 05:06 In this condition, the PTH level is low, the phosphorus level is normal or low, vitamin D levels are normal or low and the creatinine can be increased depending upon whether or not there is calciuresis. 05:20 Parathyroid hormone releasing peptide is positive. 05:23 Symptoms and signs of malignancy will be found clinically. 05:27 weight loss, bone pain, etc., may also be manifestations. 05:31 Multiple myeloma is a clinical condition in which parathyroid hormone manifest as low, Serum phosphorus may be high, vitamin D levels are usually normal. 05:43 Creatinine is elevated if the condition also affects the kidney. 05:46 and parathyroid hormone releasing peptide is negative. 05:50 Symptoms and signs of malignancy are usually the common presentation usually with bone pain and weight loss. 05:57 Granulomatous diseases as we discussed, the classic example being sarcoidosis. 06:02 Here, the parathyroid hormone is low, the phosphorus levels are high, vitamin D levels are high, Creatinine, if the kidney is affected by the underlying condition will manifest as an increased creatinine or alternatively, if the patient has a very high level of calcium and they are dehydrated, may manifest with the pre-renal state which would be another cause of an elevation of creatinine. 06:28 And then finally, PTHrP will be negative. 06:32 The clinical features of sarcoidosis and TB vary but mostly affect the lungs. 06:38 Hyperthyroidism, interestingly enough, will not cause any derrangements in PTH, phosphorus, vitamin D or creatinine. 06:47 The PTHrP will be negative but they may be the direct stimulation of osteoclasts by thyroid hormone leading to hypercalcemia. 06:56 And then finally, the very rare condition of familial hypocalciuric hypercalcemia where all of the tests are negative. 07:04 One makes the diagnosis by checking a 24-hour urine calcium excretion. 07:09 Here, this will be low in the setting of an elevated serum calcium. 07:13 Checking a family history is usually indicated and these patients will then require managements depending upon the severity of the hypercalcemia.
About the Lecture
The lecture Hypercalcemia: Types and Management by Michael Lazarus, MD is from the course Metabolic Bone Disorders. It contains the following chapters:
- PTHrP Check
- Management of Hypercalcemia
- Vitamin D-dependent Hypercalcemia
- Medication-induced Hypercalcemia
- Summary of Hypercalcemia
Included Quiz Questions
Which type of carcinoma is commonly associated with hypercalcemia?
- Squamous cell carcinoma of the lung
- Small cell carcinoma of the lung
- Adenocarcinoma of the stomach
- Medullary carcinoma
- Anaplastic carcinoma
Long-term management of hypercalcemia can be achieved with which of the following treatments?
- Bisphosphonates
- Diuretics
- Antibiotics
- Parasympathomimetics
- Sympatholytics
Which of the following medications are most commonly associated with hypercalcemia?
- Thiazide diuretics
- Loop diuretics
- Potassium-sparing diuretics
- Carbonic anhydrase inhibitors
- Osmotic diuretics
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
so grateful for such a good lecture on a difficult topic. Very clear summary and helpful hints. Good summary.