Playlist
Show Playlist
Hide Playlist
High-pressure Headache
-
Slides Headaches High Low Pressure Headaches.pdf
-
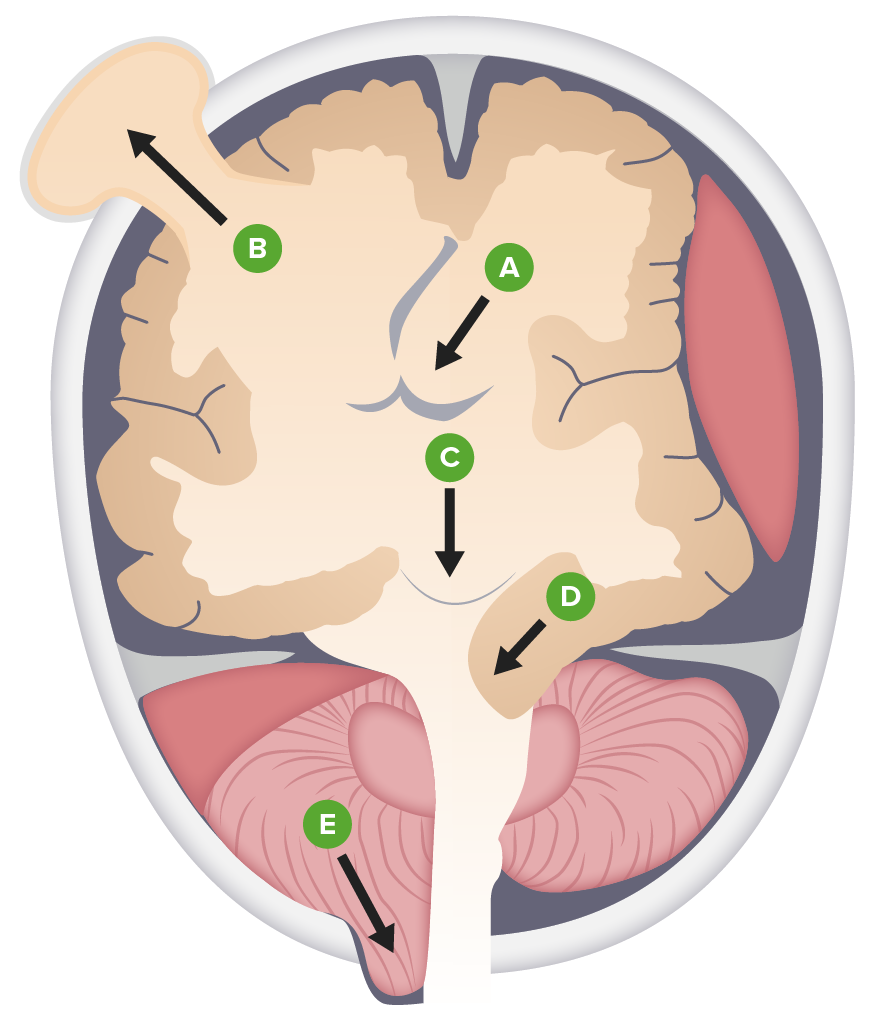
Download Lecture Overview
00:01 So let's talk a little bit more about high-pressure headaches. 00:04 What are the types? How do we evaluate them and what are the treatment? Well, high-pressure headaches occur as a result of increase in the total cranial volume. 00:14 And there's really 3 things that sit in the cranial vault, there's the brain tissue, the CSF, and the vascular system. 00:21 And an increase in any of those one compartments too quickly can result in a high-pressure headache. 00:28 Too much brain can result in a high-pressure headache, and that's a brain tumor. 00:32 Too much cerebral spinal fluid can result in a high-pressure headache, and we call that pseudotumor cerebri. 00:39 It looks like a tumor. 00:40 But when we do imaging to evaluate the tumor, we don't see it. 00:43 It's not a too much brain problem or brain tumor, it's too much CSF, that's contributing to that patient's symptoms. 00:49 Or too much of the blood vessels, and in this case, the veins and the finding, we would see there would be a venous sinus thrombus increase in the total venous volume can contribute to high-pressure headaches. 01:03 And these patients can have a positional component to their headache. 01:06 However, the early awakening is the most concerning feature that really is the red flag that points us to needing secondary evaluation. 01:15 So what are the full constellation of symptoms that we see in these patients? Patients can present with frontal headache, but we see many causes of frontal headache. 01:23 And so that's not the most specific clinical description. 01:26 The headache can be worse with lying flat, but that's actually not the most prominent symptom that we usually see in most patients. 01:33 What is important is early-morning awakening headaches. 01:37 When we go to sleep, we slowly reduce our respiratory rate. 01:40 And as the respiratory rate goes down, we maintain good oxygenation. 01:45 But we reduce the amount of CO2 that we blow off. 01:47 There's extra CO2 circulating around in the system at night, and it builds up slowly over the course of night. 01:54 CO2 can cross the blood brain barrier and it is a venodilator. 01:58 So over the course of the evening and the night, we get extra CO2 in the cerebral veins, there is relative venodilation. 02:08 And that venodilation increases the total volume in the cranial vault. 02:12 And so patients with high pressure headaches, develop increased pressure in the brain developing overnight and present with early-morning awakening. 02:20 They don't wake up and then find they have a headache at 3 or 4 or 5am. 02:24 The headache awakens them from sleep, and that's a red flag symptom that prompts and needs to prompt further evaluation. 02:32 These headaches can be initiated by coughing, sneezing, or Valsalva. 02:36 Again, those are maneuvers that reduce the venous egress from the brain. 02:42 When you Valsalva or sneeze or cough. 02:45 There's reduced venous egress, venous exit, drainage of the blood through the venous system from the brain. 02:51 There's extra blood within the venous compartment and that increases rapidly resulting in increased total brain volume and accentuates that high-pressure headache. 03:03 Patients can present with peripheral field defects, pulsatile tinnitus, or nausea. 03:09 And here on the schematic to the right, we can see how the brain drains. 03:12 We have the superior sagittal sinus and the inferior sagittal sinus and obstruction to either of those veins can cause a high-pressure headache like we saw in our patient. 03:22 Those drain down into the transverse sinus which runs around the cerebellum and we saw this transverse sinus thrombosis in our patient. 03:31 This drains into the sigmoid sinus and then ultimately down into the jugular vein and blockage of any of those veins can cause increase total brain a volume and a high-pressure headache or a venous sinus thrombus as was the case for our patient. 03:46 So what are some of the causes of high-pressure headaches? We talked about increased brain tissue from a brain tumor, a brain abscess or inflammatory lesions like Balo's concentric sclerosis. 03:56 Each of those can cause increase in the total brain volume and present with a high-pressure headache, often with some other focal neurologic deficit or seizure. 04:04 Too much CSF and that's called pseudotumor cerebri or intracranial hypertension. 04:10 For some reason there is increased CSF production without the ability to reabsorb that results in increased total brain volume and a high-pressure headache. 04:19 Those patients present like they have a tumor. 04:21 They can have papilledema and high-pressure headaches. 04:23 And when we do a scan, we don't see the tumor and it's called pseudotumor cerebri. 04:29 And then vascular system problems like venous sinus thrombus. 04:32 So those are the three things to consider in patients who present with high-pressure headaches. 04:37 How do we evaluate these patients? Fundoscopic exam is critical. 04:41 This is a high pressure headache, there is increased ICP and we look for that through fundoscopy and looking for papilledema which is increased pressure of the optic nerve head. 04:52 Papilledema would point us to needing additional imaging with either CT or MRI. 04:57 And really MRI is the modality of choice with and without contrast. 05:01 And we're looking for signs of a venous sinus thrombosis or a tumor abscess or other contributing cause. 05:07 And ultimately lumbar puncture may be needed. 05:10 That's how we look at the pressure, we can check an opening pressure and look whether the opening pressure in the CSF is elevated. 05:17 An opening pressure greater than 25 or around 25 cm of water is considered elevated and would be diagnostic of intracranial hypertension or elevated ICP. 05:29 Here's an example of endoscopy and a patient with intracranial hypertension. 05:33 This patient has pseudotumor cerebri. 05:36 We see both the right and the left eye, we're looking right in on the optic nerve, and we see the optic nerve head is bulging out. 05:44 We do not see a clear disc, a clear line of well-demarcated optic disc. 05:49 Instead, as it bulges out, we see a poorly defined indistinct border of the optic disc. 05:56 Sometimes that bulging out obscures blood vessels and we lose the ability to see the blood vessels as they course out of the optic nerve and optic disc to feed the rest of the retina. 06:08 This is severe bilateral papilledema, which is indicative of increased ICP and would be consistent with a high-pressure headache presentation. 06:17 This patient was treated with both medical therapy, maximum medical therapy and over time there was resolution of the patient's papilledema. 06:25 And here in the bottom, we see very well-demarcated optic nerves. 06:29 Look at the difference between the bottom and top, those optic nerves. 06:32 We see the arteries exiting out of the optic nerve and optic cup. 06:38 You can see the entire course of the arteries and resolved papilledema in this patient who was treated. 06:45 And this is why funduscopy is so important. 06:47 It's how we see the pressure in the brain non-invasively. 06:53 How do we treat high-pressure headaches? Well, it really depends on what the cause is. 06:56 Pseudotumor cerebri that idiopathic intracranial hypertension, too much pressure is treated with a number of interventions. 07:06 Weight loss is important, to increase weight can cause increased CSF production. 07:10 And so weight gain can be one contributing factor not always the only cause but an important contributing factor. 07:16 And this is a modifiable intervention, where we can reduce patient's likelihood of developing severe vision loss in association with pseudotumor cerebri. 07:27 Acetazolamide is a medicine that has carbonic anhydrase properties that reduces CSF production. 07:34 It's not perfect, and some patients can fail this medicine. 07:37 But in patients where there's increased CSF production, acetazolamide, which reduces CSF production is an important to intervention. 07:44 And for those that fail conservative management with weight loss and acetazolamide will consider CSF diversion of ventricular shunt diverting CSF out of the brain. 07:54 And in some cases, for patients who have severe vision loss or impending vision loss, we would consider optic nerve fenestration and that's making small cuts into the optic sheath that surrounds the optic nerve and allowing that CSF to egress out to avoid a compression and ischemia or infarction of the optic nerve. 08:15 For patients that have a brain tumor, we need to find and treat the tumor or whatever that cause may be abscess or an inflammatory lesion. 08:23 And in patients who have a venous sinus thrombus, the treatment choices anticoagulation and removal of the causative factor. 08:31 Whether it be oral contraceptive pills or underlying hypercoagulability, or what the nytus was for of the venous sinus thrombus. 08:41 So let's talk at the very end about idiopathic intracranial hypertension. 08:45 This is a very important condition to understand. 08:48 And I'd like for you know a little bit about how we treat this. 08:51 The other name for this is pseudotumor cerebri. 08:53 And you will see both of those used interchangeably. 08:57 Weight loss is an important management. 08:59 It's often not the only management, but weight gain is a modifiable risk factor. 09:04 And so we counsel patients in weight management to help reduce the amount of CSF production and manage this condition. 09:11 In addition, if patients do not have an immediate threat to vision, then we would consider medical therapy with acetazolamide. 09:19 Starting at a moderate dose and escalating that dose as needed based on the patient's vision exam and so ophthalmology consultation is critical for these patients. 09:28 We think about a headache assessment evaluating the headache phenotype, eliminating medications that may be contributing or causing this condition. 09:37 Tetra cycling's are known to cause pseudotumor cerebri and there are others that need to be evaluated, and then we treat again with acetazolamide and weight loss. 09:46 Ophthalmology assessments are critical. 09:48 Looking at the degree of papilledema is important to understanding patient's response to treatment. 09:54 If significant deterioration in visual function occurs, we would consider diagnostic lumbar puncture. 09:59 We want to make sure that the reason for the decline is increase in intracranial pressure, it's worsening of the intracranial hypertension. 10:07 If the LP shows pathologically high opening pressure, then we would consider temporizing with a lumbar drain to drain off the spinal fluid, and if needed, potentially a shunt or other intervention to manage a CSF diverting procedure, or optic nerve fenestration. 10:23 Though this is really rarely done these days, and few ophthalmologists would consider this and really favor CSF diversion these days. 10:30 If the opening pressure is not pathologically high, then we have time to reevaluate and treat other potential offending causes. 10:37 So the management of pseudotumor cerebri is important to understand those broad strokes if not each of the individual details. 10:45 And if the patient does present with fulminant threat to their vision, we would consider going straight to CSF diversion or lumbar drain or a procedure that would quickly resolve this increase in CSF pressure.
About the Lecture
The lecture High-pressure Headache by Roy Strowd, MD is from the course Headache.
Included Quiz Questions
What is the other name for pseudotumor cerebri?
- Idiopathic intracranial hypertension
- Balo concentric sclerosis
- Sagittal vein thrombosis
- Brain abscess
- Pituitary apoplexy
What is papilledema?
- Swelling of the optic discs due to increased intracranial pressure
- Swelling of the eyeballs due to increased intracranial pressure
- Edema of the pupils
- Edema of the papillae of the brain
- Cerebellar edema due to increased intracranial pressure
What is the mechanism of action of acetazolamide in treating increased intracranial pressure?
- It is a carbonic anhydrase inhibitor that decreases CSF production.
- It is an anti-inflammatory that decreases the swelling in the brain.
- It is a pain medication that treats high-pressure headaches.
- It is a loop diuretic that decreases CSF production.
- It is an anticoagulant that treats venous sinus thrombosis causing high-pressure headaches.
In addition to recommending weight loss for a patient with idiopathic intracranial hypertension, what is an essential part of treatment?
- Referral to ophthalmology
- Referral to bariatric surgery
- Referral to otolaryngology
- Starting on tetracycline
- Starting on antihypertensive medication
What is considered a significantly elevated opening pressure on lumbar puncture?
- 25–30 cm H20
- 5–9 cm H20
- 10–14 cm H20
- 20–24 cm H20
- 15–19 cm H20
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |