Playlist
Show Playlist
Hide Playlist
Gout: Diagnosis and Treatment
-
Slides Gout.pdf
-
Reference List Rheumatology.pdf
-
Download Lecture Overview
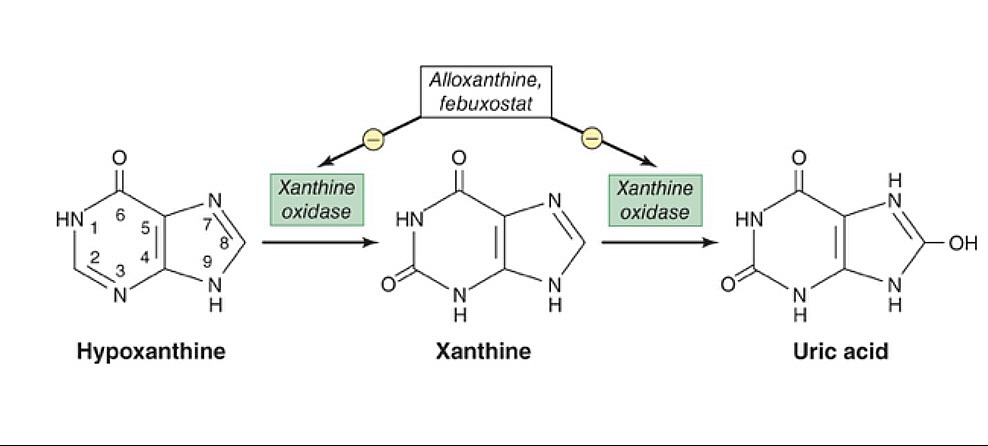
00:00 So let's go back to our case and see if he has any of those particular risk factors. 00:05 So, his age is 51 and he's a man. 00:08 Those are classic symptoms or classic features that may go along with gout. 00:12 HIV, a chronic inflammatory state. 00:15 That's gonna potentially contribute to increased purine synthesis. 00:20 He's got hypertension, we talked about that. 00:22 CKD, he's clogging the drain. He's obese, that's a factor. 00:26 He's on a diuretic, everything's going for gout for this guy. 00:30 And of course, he has a history of gout. 00:32 So enough things on the page that will help us to say that gout is a very likely contributor to what could be going on for him. 00:40 Now the thing that's unusual about our patient is the fact that he's telling us that he has 2 joints involved and that his symptoms evolved over the span of over 5 days. 00:48 And we looked at that picture before of a rat, biting unto somebody's toe and that was a monoarticular gout and was a very acute onset . 00:56 So what's the deal with this guy having multiple joints involved and at being a more protracted kind of evolution overtime. 01:02 So in order to answer that question, we have to understand the natural history of gout. 01:07 Starting here on the far left of this schematic is hyperuricemia. 01:12 It turns out that a person kind of have hyperuricemia with a level of uric acid in the bloodstream greater than 7.0 ng/dl for about 10 years potentially before they have their first gout flare. 01:25 Once they've had their first gout flare, which would typically be monoarticular, there's a 60% chance they will have a recurrence within the next year. 01:34 With each subsequent recurrence, the time between recurrences get shorter and shorter as shown here by the bars of recurrence time point over time. 01:45 And in addition, each recurrence is more likely to be prolonged with a more gradual onset and a longer phase of recovery. 01:53 And also, you are more likely to have polyarticular flares. 01:57 Our patient has an oligoarticular flare but overtime if the disease continues to be untreated, he may start to have 5, 10 different joints involved at a time. 02:06 With another 10 years of time, you can start to develop tophi. 02:10 Tophi are these tophaceous deposits in the joints that are basically just uric acid crystal deposition that can be palpable on the skin or around a joint. 02:22 And of course, chronic arthritis with some erosive changes being found as well. 02:27 So actually, his story of having gout for a long time and having this oligoarticular presentation and a slow onset of symptoms is pretty typical for untreated or prolonged gout. 02:40 So, this is actually a pretty typical story of a patient who has chronic gout and all of these symptoms could really be explained by that. 02:48 However, it's important for us to exclude some potential other pathologies, most notably, septic joint. 02:54 Something you just can't miss. 02:56 So, I think we're gonna have to perform an arthrocentesis In this case, nothing's easier than tapping the right knee. 03:02 It's a very large joint, easy to get some fluid from, so let's do that and see what we get. 03:09 Okay, so here's our arthrocentesis findings. 03:12 Many negatively birefringent needle-shaped crystals. 03:16 I wonder what that means. 03:20 So here we see negatively birefringent crystals. 03:24 This is basically monosodium urate which forms crystals when they deposit in fluid. 03:30 In this case you can see that they are negatively birefringent which means shining depolarized light in one direction will have a yellowish, orange coloration. 03:39 Whereas on the other direction, the blue crystals that are on the side are highlighting in blue. 03:44 That's a characteristic feature of monosodium urate crystals and is different than some of the other types of crystals which can deposit in joints. 03:51 So, in addition from our arthrocentesis, we see that he has a few blood cells, 55,000 neutrophils. 03:59 The number of neutrophils is also important. 04:01 On this schematic here, just highlighting how the number of white blood cells found in the arthrocentesis fluid may help to guide us towards thinking about different types of conditions that afflict the joints. 04:13 If you have less than 2,000 cells, we're thinking about non-inflammatory causes, osteoarthritis would be good example. 04:20 A rheumatologic idealogy may be reactive arthritis or lupus or something like that. 04:25 2,000-20,000 would be a typical number of cells to be found in such a joint. 04:30 Gout can be a wide range, about 20 to maybe 80,000 cells would be pretty typical for a gout flare. 04:37 And then if you've got more than 80,000 cells in a joint, maybe even over a 100,000 cells, then you really should be worried about septic joint. 04:45 So in our case, our patient's got about 50, that's pretty typical for acute gout flare. 04:50 It probably makes sense at this point that take a step back and ask, "Why are those cells in the joint?" This is the concept of crystal induced inflammation. 04:59 That is uric acid crystals cause an inflammatory cascade within in a particular joint. 05:05 How did the crystals end up in that joint? What's the number of extrinsic factors that contribute to that? We're thinking about the general chemistry here. 05:13 What causes a particular substance to crystalize in solution? Well, these factors are things like the pH of the solution, in this case synovial fluid. 05:23 The temperature, typically lower temperatures are gonna contribute to crystal supersaturation and crystal formation. 05:29 And then dehydration, simply that's gonna affect the concentration of uric acid in solution. 05:35 We think about podagra, again, which most commonly occurs late in the evening, it's afflicting the great toe and in the evening, that's when you're relatively breathing at a slower rate, so your pH of your blood and of your articular fluid is gonna be a little bit more acidic, you're gonna be little bit cooler especially if your toes are peeking out from underneath the sheets. 05:57 And you're also gonna be relatively dehydrated because you haven't had any fluid consumed while you've been sleeping. 06:03 All those factors contribute to why your first flare of gout tends to occur in the great toe while you're asleep at night. 06:10 So, uric crystals form and then once they form they deposit into synovial tissues and you can imagine having little knives sticking into your joint's synovial fluid or joint synovium, that's gonna contribute to an inflammatory response. 06:25 Initially, there will just be a local cell mediated response with some macrophages and monocytes. 06:30 Ultimately, they're gonna recruit large numbers of neutrophils and then boom, crystal-induced inflammation. 06:37 Fortunately, this process also is self resolving and over time, those neutrophils go away, inflammation dies down and your typical gout flare can last 5 to 7 days and go away on it's own. 06:50 So, we've got crystals, we've got neutrophils, sounds like we're done, right? No. 06:59 Always remember that just because the patient has gout, that doesn't mean, he doesn't also have septic joint. 07:05 We still need to perform a gram stain and a culture and keep this person on antibiotics until we get that information back. 07:12 A person can have gout and have an infection at the same time. 07:15 So, now we've got some more data, gram stain is negative, fluid culture has no growth. 07:21 Alright, so we should methodically just go through our list one last time here. 07:25 So we can officially take out pseudogout, we have no evidence of CPPD crystals on the synovial fluid. 07:31 We'll talk more about those crystals in a moment. 07:33 Septic joint, that's out. 07:35 We got a negative culture from the fluid as well as a negative gram stain. 07:39 Lyme disease, doesn't seem very likely anyway 'cause wh didn't have any risk factors and doesn't have any skin rash. 07:44 So, I think we can safely say that our patient's symptoms can be fully explained by an acute gout flare. 07:51 So, it's gout, now what? To talk about the treatment of gout, we should reflect again a little bit on our bathtub analogy. 08:02 If we wanna reduce some of the many symptoms of gout, we have to focus on either first, managing the acute inflammatory process and then secondly, we wanna focus on slowing down the tap and also unclogging the drain. 08:15 In our case, he's having an acute flare, we really wanna focus on cooling down on the inflammation before we do anything else. 08:22 So, this category down here is what we want to focus on. 08:25 Anti-inflammatories: NSAIDS, colchicine, systemic steroids or intra-articular steroids. 08:31 Now our patient has some CKD. 08:34 We have to be a little cautious about using NSAIDS or cochicine which are both renally excreted. 08:40 So in this case, since we know we can tackle two different joints, the knee and the ankle, it would be most pertinent to use intra-articular steroid. 08:49 Systemic steroids would be fruitful if it's a very hard joint to tap or if there's multiple joints involved. 08:56 Once we've accomplished that and cooled down his acute flare, then we could go back and start talking about managing the uric acid production by tackling things like or using things like allopurinol or febuxostat which is gonna decrease uric acid production. 09:12 And on the right hand side, trying to unclog the drain by promoting uricosuria or urate excretion. 09:19 Classic agents like probenecid and sulfinpyrazone have been shown to increase uric acid excretion. 09:26 Those are gonna be medications we'll be using in a long term to prevent future flares.
About the Lecture
The lecture Gout: Diagnosis and Treatment by Stephen Holt, MD, MS is from the course Non-Autoimmune Arthritis.
Included Quiz Questions
Which of the following tests is most helpful to differentiate between septic arthritis and gout?
- Arthrocentesis
- X-ray of the joint
- Serum uric acid level
- CT scan of the joint
- Urinalysis
Which of the following synovial fluid findings is most suggestive of gouty arthritis?
- Yellow, WBC count = 30,000 cells/mm3
- Colorless, WBC count = 150 cells/mm3
- Green, WBC count = 150,000 cells/mm3
- Yellow, WBC count = 700 cells/mm3
- Red, WBC count = 800 cells/mm3
Which of the following is the most appropriate treatment for a gout attack in patients with renal insufficiency?
- Intra-articular steroid injection
- Ibuprofen
- Celecoxib
- Allopurinol
- Indomethacin
Which of the following drugs is most appropriate to help prevent recurrent gout attacks?
- Allopurinol
- Colchicine
- Indomethacin
- Celecoxib
- Adalimumab
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
lots of useful and clinically relevant material given in a clear way