Playlist
Show Playlist
Hide Playlist
Gastroesophageal Reflux Disease (GERD)
-
Slides GIP Gastroesophageal Reflux Disease GERD.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
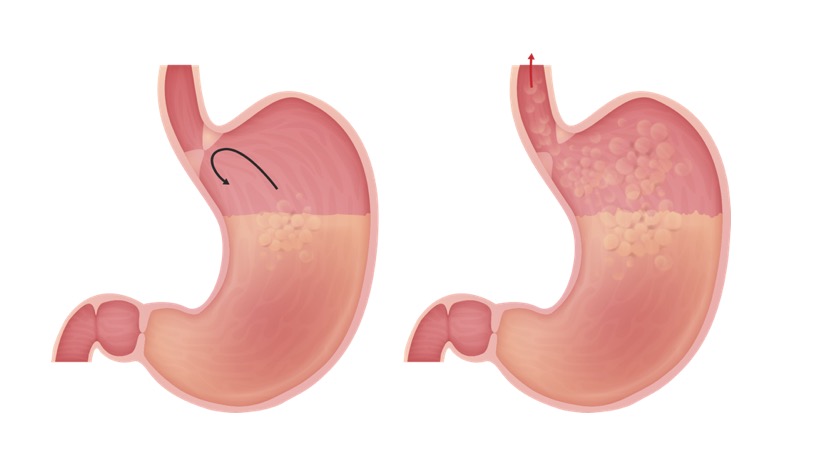
00:01 In this talk, we're gonna discuss gastroesophageal reflux disease or GERD. 00:05 And I would hazard to guess that everyone watching this at one point or another has had some of the symptoms of GERD, otherwise known as heartburn. 00:15 And particularly, for medical students who are constantly stressed, this is not an uncommon disorder for us to have. 00:22 So basically, this is reflux of gastric contents, stomach contents into the esophagus. 00:29 Those gastric contents are acidic and they will cause irritation of the lower lining of the esophagus which is not really designed to be flooded with gastric acidity, hydrochloric acid at a pH of 2. 00:43 So the epidemiology of this, there are a number of risk factors but fundamentally, you should think about it in these two ways. 00:51 One is that we could have increased abdominal pressure which is basically forcing the stomach to push its contents not down, but up. 01:00 Or you may have reduced lower esophageal sphincter tone, the LES. 01:04 And that lower esophageal sphincter is very importan for keeping things in the stomach and not going backwards. 01:10 When that tone relaxes and it does under normal physiologic conditions when a bolus of food is coming down but if it relaxes at another time, gastric contents can go up. 01:22 So how do we get increased abdominal pressure? Obesity is probably the greatest reason along with pregnancy. 01:31 But you can do it transiently without being obese or pregnant by just having a huge meal. 01:37 So at Thanksgiving for people in the United States, but at other celebratory events when you have a large bolus of food and it's not getting out of your stomach, that can cause increased abdominal pressure and you can get reflux. 01:51 Also, it turns out that physical activity, even so much as walking around the kitchen after you've had a huge meal will give you enough gastric motility to move that food out into the duodenum and into the small bowel. 02:05 So that was increased abdominal pressure. What about the other risk factor? Decreased lower esophageal tone or LES tone. A number of medications will impact this. 02:15 So nitrates, calcium channel blockers, things that we routinely give older patients for cardiac diseases will cause relaxation. 02:25 Smoking actually also causes relaxation of the LES as does caffeine. 02:31 Medications for asthma will frequently do this and asthma all by itself by causing neurogenic signaling can cause LES sphincter relaxation. 02:43 Alcohol will cause relaxation and anxiety or depression by changing neurogenic signaling throughout the body can affect it and then, for you medical students out there, stress. 02:58 So that will reduce. It doesn't increase intraabdominal pressure but it does relax the lower esophageal sphincter and you can get reflux. 03:06 So let's talk about pathophysiology. 03:08 As we've already discussed in terms of etiologies, decreased LES tone will drive this and a number of things that we just talked about will drive that particular phenomena. 03:21 You can also have transient lower esophageal sphincter relaxation. 03:25 This normally happens when a bolus of food is coming down. 03:29 Otherwise, you can't get food from the esophagus into the stomach, but you can have transient, inappropriate opening of that which will, when food is not coming down, allow gastric contents up. 03:41 You can actually have impaired esophageal motility. 03:45 So esophageal dysphagia can lead to this and we - and other talks will cover a variety of etiologies of that entity. Delayed gastric emptying. 03:55 So you can have food coming down, stored in the stomach, distended, and then, for a variety of reasons, the pylorus, the pyloric sphincter doesn't open. 04:06 And now you - it's like having a huge meal. 04:08 There's no place for it to go, so it tends to regurgitate. 04:12 And then, finally, if there's weakening at the point where the esophagus transcends through the diaphragm into the stomach, if there's a defect there, you can have the stomach kind of herniate up into the thoracic cavity and that's what we're looking at on the x-ray. 04:28 We're seeing the fundus of the stomach way up here in the chest as a result of a hiatal hernia. 04:33 Clearly, that will impact. It will stretch and open the lower esophageal sphincter and we'll get reflux. 04:41 So in terms of the pathophysiology, we're really looking at the crux of the matter right here. 04:47 When there are contents within the GI, within the stomach of the GI tract, it doesn't reflux because of the closure of the lower esophageal sphincter. 04:58 So you see that curved arrow. Things are not going up into the esophagus. 05:02 If on the other hand we have an incompetent or just a lower esophageal sphincter that is not closing appropriately, clearly, gastric contents can go retrograde. 05:14 We can also have increased frequency of the LES sphincter relaxations as I already talked about which will have very much the same effect. 05:26 And then, the hiatal hernia as you see here where there's a defect in the diaphragm, allowing the stomach to protrude up near the junction at which the esophagus enters the stomach. 05:39 And obviously, increased intraabdominal pressure will have a tendency to move things retrograde. 05:47 So what are the clinical manifestations? Well, as I said, I think probably every one of you has had some of the symptomatology associated with GERD. 05:57 And so, you're more familiar with what it feels like. 06:00 There will be dysphagia, so there will be a discomfort or abnormal movement of food after swallowing. 06:08 Or there may be pain associated with that, that's odynophagia and that's due to second, it's due to mucosal irritation and damage. 06:17 The most common symptom patients will tell you about is heartburn. 06:20 It hurts right here in the middle of my chest and it's kind of burning. 06:25 And I feel like I have a foul taste in my mouth. 06:27 Well, that's actually gastric contents going all the way back up into the mouth. 06:33 There's a sensation of something being in one's throat, a Globus sensation. 06:37 The patient may belch, may have nausea, and actually, if you are having significant gastroesophageal reflux, you can have those contents get into your airway, into the trachea, into the bronchi, and into the lungs. 06:52 And in fact, in a certain number of patients, late onset of asthma or even a frank pneumonia may actually be associated with gastroesophageal reflux disease. 07:05 So how do we make the diagnosis? Well, a lot of it is clinical. 07:08 You have the sensation after eating or in certain positions of a burning sensation or belching, or a foul taste in one's mouth, all of that. 07:17 We can formally document it by having pH monitoring. 07:21 We can actually put a probe down into the esophagus of a patient and see that the pH gets down to one or two in certain times where it's inappropriate. 07:31 If we are suspicious of someone with chronic GERD, we need to actually surveil them, pay attention to them in case they might be developing malignancy. 07:44 So reflux is associated, has a high risk of developing Barrett's metaplasia. 07:50 As I already said, the esophageal mucosa which is a stratified squamous, non-characterizing epithelium that you see in most of what's on the right-hand side, that epithelium does not like gastric acidity. 08:03 So when it is bathed in it recurrently, it undergoes what is called a gastric metaplasia or intestinal metaplasia and develops a lining that is much more like the stomach or small bowel and that's what's in the middle of that picture on the right. 08:18 When that happens, that metaplasia increases the risk of the development of adenocarcinoma of the esophagus. 08:25 So chronic GERD really requires that we'd look down the esophagus and that's what you're seeing in the left-hand side with an endoscope. 08:35 And we are looking at the lower esophageal sphincter. 08:38 That shouldn't look quite that red in the middle with that kind of ragged red edge. 08:43 It should look more like the white tan tissue that's all the way around the periphery, but not like that angry red stuff in the middle. 08:51 That's a patient with a Barrett's metaplasia and we need to watch that very carefully with recurrent biopsies to make sure that they don't transform into adenocarcinoma. 09:01 So how do we manage GERD? So there are a lot of simple things, and then, with more complex problems like a Barrett's metaplasia, we have to be more aggressive. 09:10 So the simple things. Let's do a lifestyle modification. 09:13 Gee, don't eat within three hours of bedtime, okay? And that will keep you from regurgitating during sleep into your lower esophageal sphincter. 09:23 If you're obese, let's lose some weight. 09:26 I realize it's more easily said than done but it's certainly something that will help your patients. 09:32 Elevate the head of the bed to prevent reflux and the nocturnal symptoms that happen during sleep. 09:38 And avoid triggers, alcohol and coffee as we've already talked about cause relaxation of the lower esophageal sphincter and that will make the symptoms of GERD much worse. 09:50 So we maybe not be able to get much success with just simple changes and may require that we do medical therapy. 09:58 Mostly, the medical therapy is targeted to reducing the acidity of the gastric fluids that could reflux over into the lower esophageal segment. 10:07 So we'll give antacids or histamine receptor antagonists or proton pump inhibitors all to reduce the gastric acid secretion. 10:15 As I've said previously, we're gonna have to watch very closely for the development of malignancy associated with the Barrett's metaplasia. 10:22 In some cases, all of this therapy is just not very successful or we have relative atypia of the Barrett's metaplasia in which case, we need to go in surgically to reduce in that fashion, the amount of regurgitation. 10:37 The typical surgical technique is to do a fundoplication where we literally tie a suture around the top of the stomach at the lower esophageal sphincter and make it tighter so that we don't have as much gastric reflux. 10:55 And with that, we've gotten to the end of heartburn, gastric esophageal reflux disease.
About the Lecture
The lecture Gastroesophageal Reflux Disease (GERD) by Richard Mitchell, MD, PhD is from the course Disorders of the Esophagus.
Included Quiz Questions
What is NOT a risk factor for GERD?
- Exercise
- Obesity
- Pregnancy
- Eating habits
- Nitrates
What is a symptom of GERD?
- Dysphagia
- Anemia
- Pleuritic chest pain
- Mouth ulcers
- Hematochezia
What is a complication of GERD?
- Barrett metaplasia
- Colonic adenocarcinoma
- GI stromal tumor
- Squamous cell carcinoma of the upper esophagus
- Zenker diverticulum
What is one recommendation for the conservative management of GERD?
- Avoiding eating within three hours of bedtime
- Maintaining weight
- Increasing coffee intake
- Antacid medication
- Eating a large breakfast
What is a surgical technique used to manage GERD?
- Fundoplication
- Whipple
- Gastric bypass
- Gastrohepatic ligament suspension
- Gastroduodenal ligament suspension
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
de los mejores doctores que tiene la plataforma, definitivamente amo sus videos!! saludos desde argentina..
4 customer reviews without text
4 user review without text