Playlist
Show Playlist
Hide Playlist
G6PD Deficiency: Pathophysiology
-
Slides G6PP Deficiency.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
00:00 Now, let’s talk about the pentose phosphate pathway in greater detail. 00:04 You focus upon the fact that you’re producing NADPH for the RBC. 00:09 Why do you require that NADPH? So that you can produce the all important glutathione. 00:15 What about that glutathione? What kind of issues do you want to know about this? Well, glutathione not only protects the RBC, but if you remember correctly, what’s one of the common causes of liver transplant in adolescence and young adult? One of the most common causes is acetaminophen poisoning or Tylenol. 00:34 And so therefore, don’t you require proper amounts of glutathione in the liver in zone 3 so that you can then metabolize and detoxify some of these NAPQI that acetaminophen produces. 00:45 That’s the last time that you saw that and then you should know about that drug called N-acetylcysteine in which you then replenish the glutathione in patients that hopefully, hopefully, that you can reverse the effects of acetaminophen. 00:58 That’s the last time that you saw this clinically. 01:01 Here it is in the setting of G6PD deficiency. 01:05 This glutathione repairs the oxidative damage. 01:09 Now, let’s walk through this so that you can clearly understand the clinical picture of a patient that has G6PD deficiency. 01:17 So now, let’s say that you have a patient who is from the Mediterranean. 01:21 Maybe they’re Italian, maybe they’re Lebanese. 01:25 In that area, they end up consuming and they do consume quite a bit of fava beans. 01:31 And so let’s say that you have a patient who has X-linked recessive, who now has been exposed to fava bean. 01:38 What is a fava bean known as? What do you want to know as a fava bean? For each bean that you take in, think of it as being a free-radical. 01:46 Okay? So let me have a meal of free radicals. 01:49 Wow! So let’s say that a patient who has G6PD deficiency is introducing bean by bean by bean of free radicals into the body. 02:00 So now, what happens? There’s oxidative stress, isn’t there? And now, the RBC can’t protect itself effectively against the free radical that’s being introduced to the body. 02:11 So now, what happens? What does that RBC contain? No nucleus, no mitochondria, but a heck of a lot of hemoglobin. 02:20 So what happens? With these free radical damage or oxidative damage, give me another one. 02:25 How about if you’re going to the Caribbean or you’re going to some place tropical, shall we say? Maybe perhaps you're taking antimalarial drugs. 02:33 Those are oxidative stresses and free radicals that you’re introducing to the body. 02:40 So let it be fava beans, I’ll give you another one here such as chloroquine and company. 02:44 And so these are the free radicals that you’re introducing to the body. 02:47 And when you do so, the hemoglobin within the RBC will get damaged. 02:52 And it will precipitate. 02:54 This precipitation of the hemoglobin within the RBC is called a Heinz body, H&H, hemoglobin, precipitation, Heinz body. 03:05 So whenever you have a hemoglobin within an RBC which is unrecognizable, then this RBC unfortunately becomes the enemy. 03:12 So therefore, in the body, your RBCs is seen as the antigen. 03:16 What is that going to do? It’s going to attract your phagocytic cells. 03:19 Here comes the phagocytic cell and what does it do? It takes a bite out of your RBC. 03:25 Then you call this RBC what? A bite cell. 03:28 It literally looks like the RBC has been bitten into. 03:33 It’s amazing, it’s amazing. 03:35 So now, with that said, in terms of your question, remember that question that you want to ask yourself for every single anemia, intra-, extra-, intra-, extravascular. 03:44 Now, be careful with G6PD deficiency. 03:46 If you completely bite, bite, bite, bite like Pac-Man. 03:50 Well, I don’t even know if you know what Pac-Man is. 03:52 It’s a game that I used to play when I was young. 03:56 And it eats completely the RBC, then it's intravascular hemolysis, right? But what if you just had a bite cell? Then maybe that RBC will be taken out of the vasculature and taken to the spleen. 04:08 And that will extravascular. 04:10 So be very careful with G6PD deficiency because this patient upon exposure to the oxidative stress might either have hemoglobinuria or might have significant jaundice, intra and extra exists both with G6PD deficiency. 04:27 Let's continue. 04:28 So what is a Heinz body? H&H. 04:31 Heinz, denatured hemoglobin. 04:34 What’s a bite cell? It is the phagocytic cell that’s coming in and taking a bite out of your RBC membrane and that damaged RBC could either be completely destroyed in the vasculature, intravascular or commonly taken to the spleen and so therefore you call that extravascular hemolysis. 04:54 Now there’s a couple of other things that you’re going to like about GCPD deficiency as we go through these further because, well, I told you I’m never just going to give you one disease and walk away from this because you are taking the boards. 05:07 When you take your boards and you’re given questions, there are going to be certain things in the clinical vignette in the question stem that you might think of it as being a buzz word. 05:17 In your mind, you’re thinking, “Oh, my goodness. This is G6PD deficiency, no doubt.” No, no, no. 05:22 Be very, very careful. 05:23 What I mean is the following. 05:25 Say that your patient has susceptibility to catalase-positive organisms. 05:32 As soon as you see catalase-positive organisms susceptibility, you probably have gotten to the habit from basic pathology immunology of immediately going into chronic granulomatous disease. 05:45 Do not ever do that from henceforth. 05:48 Why? "How in the world, Dr. Raj, do you bring the differential of chronic granulomatous disease with G6PD deficiency, what the heck would they even have in common? Guess what? Both of your patients will be susceptible to catalase-positive organisms. 06:07 Give me an example, the prototype of course you all know, Staph aureus, right? Staphylococcus. 06:13 "Dr. Raj, I’m still not seeing it because you’re telling me that I’m being susceptible to an infection, but yet we’re talking about RBC, a red blood cell. 06:24 And red blood cell doesn’t protect me against bacteria. 06:26 I get all that and you have valid points, I understand. 06:31 However, what are you now producing in G6PD deficiency? Pay attention. 06:35 NADPH. 06:38 A neutrophil. 06:39 Jump over to the next cell. 06:42 Leave the RBC alone, I want you to think neutrophil, picture it. 06:45 What does it look like? Oh, segmented lobes, right? And what is a neutrophil responsible for? Good. 06:53 Phagocytosing or killing bacteria. 06:57 What’s the first enzyme that you require for destruction of your bacteria? Oh, my goodness, it’s called NADPH oxidase. 07:08 There you go. 07:09 So if that enzyme requires NADPH and what don’t you have in G6PD deficiency? Look at the first bullet point. 07:18 You don’t have NADPH. 07:21 "Dr. Raj, you’re telling me that there are two cells being affected in G6PD deficiency?" That’s exactly what I’m telling you. 07:27 You’ll have hemolytic anemia and you’ll have catalase-positive susceptibility. 07:32 You will never have that in chronic granulomatous disease. 07:36 In chronic granulomatous disease, it is only one cell that’s being affected. 07:41 And that is your neutrophil because you’re missing the enzyme, NADPH oxidase. 07:47 I hope that’s clear. 07:49 Repeat that a few times so that it’s clear to you. 07:52 Amazing, isn’t it? Good differential. 07:54 Do not just jump to conclusions. 07:56 Read the entire stem because those people that are making the boards, they know as to how you function. 08:06 Your job is to get into the minds of people like me, like people who are – the question makers so that you’re not fooled. 08:14 Don’t get trapped. 08:15 Don’t let them do that to you.
About the Lecture
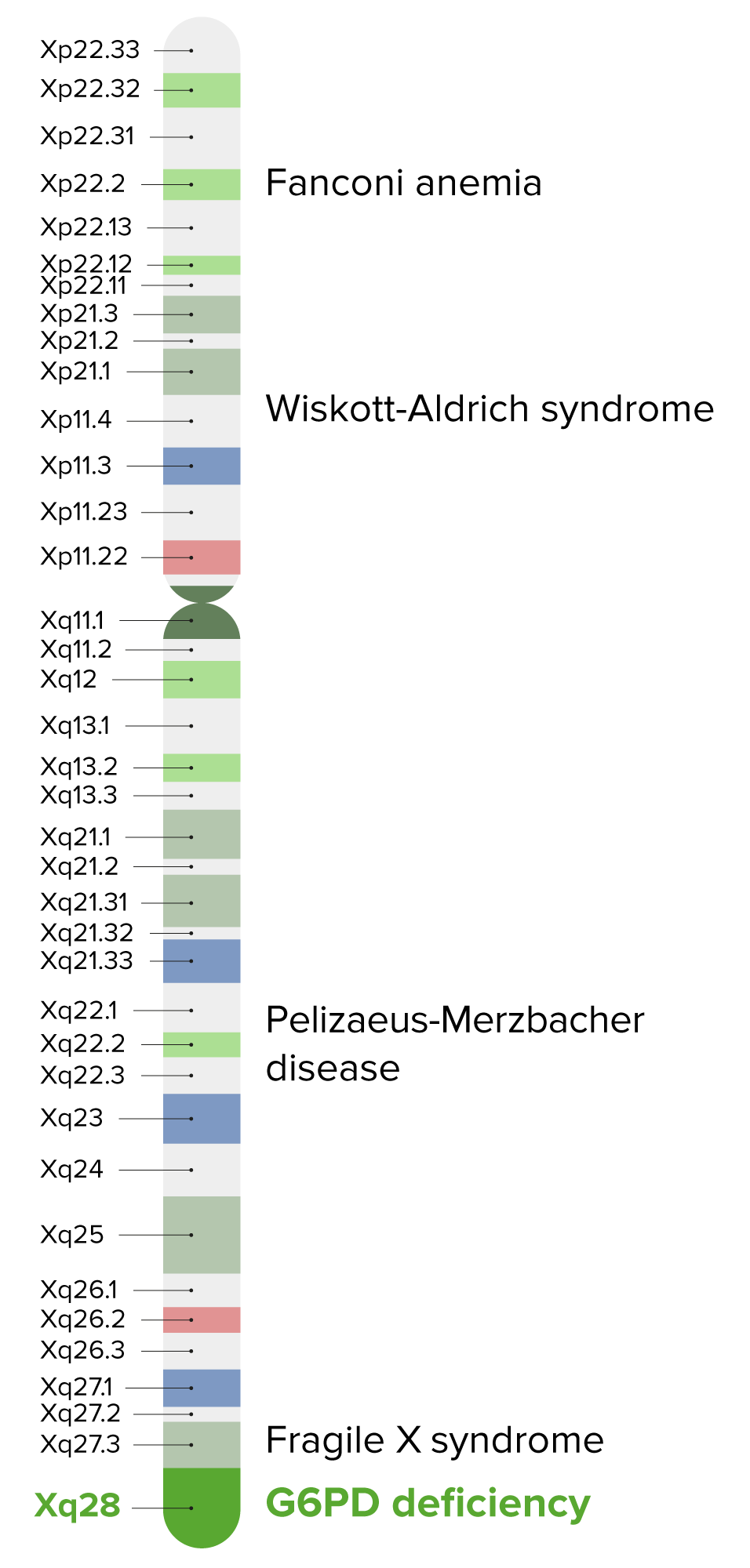
The lecture G6PD Deficiency: Pathophysiology by Carlo Raj, MD is from the course Hemolytic Anemia – Red Blood Cell Pathology (RBC).
Included Quiz Questions
The reduced form of nicotinamide adenine dinucleotide phosphate (NADPH) helps protect the red blood cells against oxidative damage by maintaining the level of which of the following?
- Glutathione
- Superoxide dismutase
- Interferon
- Hypochlorite
- Myeloperoxidase
What is the principal function of glutathione in erythrocytes?
- Prevents oxidative damage
- Maintains nicotinamide adenine dinucleotide phosphate (NADPH) levels
- Denatures hemoglobin
- Catalyzes the rate limiting reaction of hexose monophosphate shunt
- Regenerate glucose-6-phosphate dehydrogenase
All EXCEPT which of the following are characteristics of G6PD?
- Howell-Jolly bodies
- Heinz bodies
- Oxidative damage
- Intravascular hemolysis
- Bite cells
Which of the following are inclusions within red blood cells composed of denatured hemoglobin?
- Heinz bodies
- Bite cells
- Howell-Jolly bodies
- Burr cells
- Acanthocytes
Which of the following cells is characteristic of an acute attack in a patient with G6PD deficiency?
- Bite cell
- Tear drop cell
- Spherocyte
- Acanthocyte
- Target cell
Customer reviews
4,5 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Dr. Raj is amazing and funny too! Love the lectures and illustrations. Thank you!
pathogenesis explanation is detailed and Lecturer is great at helping us to distinguish difference btw the two entities