Playlist
Show Playlist
Hide Playlist
Focal Segmental Glomerulosclerosis (FSGS) – Nephrotic Syndrome
-
Slides Nephrotic Syndromes.pdf
-
Reference List Nephrology.pdf
-
Download Lecture Overview
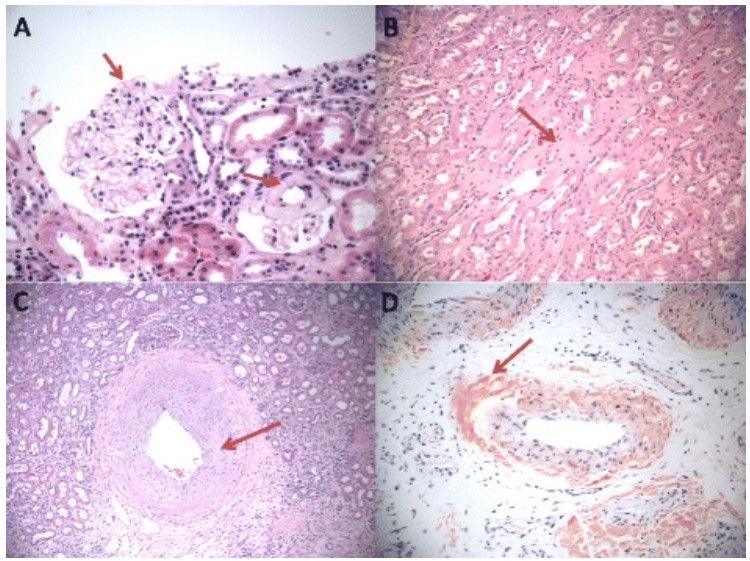
00:01 So focal segmental glomerulosclerosis, it's quite a mouthful to say so we're going to abbreviate it with FSGS. 00:07 And I want to talk about why we call it that. 00:10 One of the things I love about this is our pathologist have come up with this name and it pathologically describes exactly what's going on when we say the word focal it means that when we do the biopsy there's less than 50% of glomeruli that are involved. 00:23 So in the kidney by this disease process less than 50 or and percent of those glomeruli are going to be involved. 00:29 And then segmental means that, when you're looking at a glomerulus only a segment of the glomerulus is involved sclerosis means scar. 00:37 So less than 50% of glomeruli segmental are scarred, sclerosis meaning scar. 00:44 So that's where FSGS comes from. 00:46 It's the most common form of nephrotic syndrome in adults. 00:50 It's a second most common in children, second minimal change disease that we as we just discussed. 00:56 And again, it accounts for 35% of all biopsies of nephrotic syndrome in adults, there is an increased incidence in African American people as well as male gender. 01:08 So when we think about the ideology behind FSGS, it's a little bit complicated. 01:12 So we like to talk about it in terms of primary FSGS and secondary FSGS. 01:17 Under the primary category, we think about idiopathic and remember that's just a word to say that we haven't yet discovered what the exact etiology is, but there's also a genetic and familial type of FSGS as well. 01:29 And this involves genes that encode the slit diaphragm proteins in the foot processes of the podocyte. 01:33 That includes jeans like nephron, podocin, TRPC6 and alpha-acrinin-4. 01:38 There's also an association with the MYH9 and the APOL1 allelic variants in the African populations. 01:45 So we talked about this previously with causing hypertensive and chronic hypertension and chronic kidney disease. 01:51 We can also see a variant in association with FSGS. 01:56 So there's also a secondary FSGS, and this is going to occur in many forms of renal injury and systemic diseases. 02:02 It could be due to a loss of renal mass. 02:05 It could be due to things like obesity, HIV which is going to directly affect the podocyte, sickle cell disease, which is really a form of loss of renal mass, and drugs that directly into the podocyte. 02:16 This is these are things like pamidronate and heroin. 02:19 It's going to present more often with an erotic range proteinuria rather than nephrotic syndrome. 02:24 So oftentimes people who have secondary FSGS, may just show up with protein in their urine, but they're not always going to have the hypoalbuminemia in the lipid abnormalities in edema that we would see with our patients with full-blown nephrotic syndrome as you're going to see him primary fsgs. 02:41 So when we are biopsy our patients what we see on biopsy on our light microscopy This is a PAS stain, we can actually see segments of Scar. 02:52 So essentially what my arrow is pointing to over here is we have a sneaky attachment to Bowman's capsule and we have this area of scar that's accumulated accumulated in a segment of the glomerulus right at about 7 o'clock. 03:06 Am i immunofluorescence? It's very nonspecific. 03:09 Sometimes we get this innocent trapping of complements C3 in the area of scar, but it's not doing anything pathologically. 03:17 And then on electron microscopy what we see is in the capillary loop that involves the scar, We have podocyte foot processes of effacement. 03:25 My arrow is again pointing over here to that foot process being effaced you can actually see some of these little foot processes that are undergoing micro Villas transformation as well. 03:35 Now, in secondary FSGS, we're only going to see that foot processes effacement over the areas of capillary loop that are involved by segmental sclerosis. 03:45 In primary FSGS, over 50% of those capillary loops that are not involved by segmental Scar or going to have foot process effacement. 03:54 So that's a very helpful clue in order to distinguish between primary and secondary FSGS. 04:02 When we think about the pathogenesis behind FSGS, in primary, It's really an injury to the podocyte that most likely is due to some kind of circulating toxin which is supported by the rapidity of recurrent disease following renal transplant. 04:15 So it's very interesting when you have a patient with primary FSGS and you transplant that patient sometimes within 24 hours that patient can have an increase or explosion in proteinuria. 04:26 When you biopsy that patient they have changes consistent with minimal change disease that eventually through time develops into FSGS. 04:34 So it makes you think that there's some kind of circulating toxin that's causing this to happen. 04:39 We do think again, this is most likely related to minimal change disease because of what we see pathologically as they described. 04:46 And again, it's probably on the same disease continuum, but people with FSGS have a much less or reduced responsiveness to therapy compared to people who have minimal change disease. 04:58 In the secondary form of FSGS. 05:00 We have injury to the podocytes either by hyperfiltration mechanisms or an increase, or and an increased in glomerular capillary hypertension. 05:10 This is going to be due to those cases that include reduced renal mass, patients with chronic kidney disease, for example, our patient who has sickle cell disease will have reduced renal mass. 05:20 We also have hyperfiltration and glomerular capillary hypertension in obese patients particularly morbid obesity people greater than 40 for their BMI, tend to have vasodilation of the efferent arteriole glomerular capillary hypertension and they're at risk of obesity related FSGS. 05:37 We can also have direct injury to the podocyte, and those are things from viruses like HIV that directly affects the podocyte or drugs like pamidronate or heroin. 05:50 So in terms of how patients do overtime and primary FSGS patients may present either with acute onset of nephrotic syndrome, or it may be a little bit more insidious. 06:00 Sometimes we can see some hematuria. 06:03 They typically will have hypertension and variable degrees of reduced renal function. 06:08 Our patients again have no abnormalities in serum complements, complement is not getting activated. 06:14 In secondary FSGS, our patients always present with an insidious onset. 06:19 Remember this is something that's happening slowly over time and they may not have the full constitution of nephrotic syndrome. 06:25 They often present with asymptomatic proteinuria without the hypoalbuminemia or edema. 06:31 Untreated, primary FSGS will follow a progressive course to end stage renal disease. 06:36 So the rate of spontaneous remission in this population is really less than 10%. 06:42 The risk factors for progression include have, include having a high level of proteinuria, so greater than 10 grams at presentation people who have reduced renal function meaning that they have an elevated creatinine at the time of diagnosis. 06:53 And just as a membranous the presence of tubulointerstitial fibrosis. 07:00 So when we think about treatment of primary FSGS, it's important that all of our patients really receive nonspecific therapy. 07:07 So we've been talking about that. 07:08 That means that our patients need an ACE inhibitor or an ARB. 07:12 Loop diuretic again, that's to mobilize volume off their body and help treat that edema. 07:16 That can't happen without a low sodium diet, so we need that sodium to be less than 2 grams in their diet. 07:21 Blood pressure control us and 130/80 and hyperlipidemia treatment with a statin. 07:28 We also can do immune targeted therapy with prednisone. 07:31 So we typically very similar to a minimal change disease. 07:33 We're going to give high-dose prednisone 1 milligram per kilogram between 12 and 16 weeks duration with a taper over six months. 07:41 Again, very similar minimal change disease if her patients are steroid dependent meaning that we can't tape or steroid without them exploding again with their nephrotic syndrome. 07:49 We can give them an alkylating agent like cyclophosphamide typically between 8 and 12 weeks. 07:54 Or patients who are resistant or can't tolerate steroids. 07:58 We can give them cyclosporine in combination with low-dose prednisone. 08:03 Finally we can use things like antimetabolites like mycophenolate mofetil in our patients who are steroid dependent or resistant. 08:11 If your patient has no response to the above therapies. 08:14 It's very important that you really inquire about a familial type of FSGS or family history. 08:20 Because they may have that in these are those mutations that we talked about in the slit diaphragm. 08:25 Now, if you're patient does have familial FSGS, you can actually cure them with a transplant. 08:31 Because the recurrence is relatively low. 08:34 So for secondary FSGS, those patients typically get nonspecific therapy. 08:40 So they will have ACE inhibitors the ARB blockers that we talked about targeting that renin-angiotensin system in order to reduce the inter glomerular pressure. 08:48 That blood pressure again needs to be controlled treatment of their hyperlipidemia as we talked about. 08:54 If our patient is obese and they have obesity-related FSGS, weight loss is critical. 08:58 These are patients that we may target for bariatric surgery or other mechanisms in order to reduce their weight in order to save their renal function. 09:06 And we want to treat that underlying disease process that includes treatment of their HIV. 09:13 And anybody who is on offense of drugs, like pamidronate or heroin discontinuing those drugs are going to be of critical importance, again, in order to have a chance at saving their kidney function.
About the Lecture
The lecture Focal Segmental Glomerulosclerosis (FSGS) – Nephrotic Syndrome by Amy Sussman, MD is from the course Nephrotic Syndrome.
Included Quiz Questions
Which of the following is involved in the pathogenesis of primary focal segmental glomerulosclerosis?
- Mutations in slit diaphragm proteins
- Mutations in hemoglobin proteins
- Infection with a retrovirus
- Drug-induced podocyte damage
Which of the following is true regarding the clinical manifestations of FSGS?
- Secondary FSGS rarely presents with edema and hypoalbuminemia.
- Primary FSGS always has an insidious onset.
- Both subtypes of FSGS frequently present with nephrotic range proteinuria and lipiduria.
- Patients with primary FSGS have low C3 and C4 levels.
Which of the following histopathological changes is associated with FSGS?
- Electron microscopy reveals effacement of the podocyte foot processes.
- Light microscopy reveals fibrosis that involves > 50% of glomeruli.
- Fluorescence microscopy reveals a linear distribution of antibodies along the basement membrane.
- Light microscopy reveals the formation of spikes and domes in the basement membrane.
Which of the following is true regarding the management of FSGS?
- Familial FSGS can be cured with renal transplants.
- Blood pressure should be maintained below 140/90 mm Hg
- ACE inhibitors/ARBs are not indicated for the initial episode of FSGS.
- Cyclophosphamide is the first-line immune-targeted treatment for FSGS.
Which of the following predicts a poor prognosis in FSGS?
- Tubulointerstitial fibrosis on renal biopsy
- Young age
- Responsive to prednisolone
- Proteinuria > 3.5 g/day
- Plasma creatinine concentration < 1.3 mg/dL
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |