Playlist
Show Playlist
Hide Playlist
Esophageal Varices
-
Slides GD Esophagus.pdf
-
Download Lecture Overview
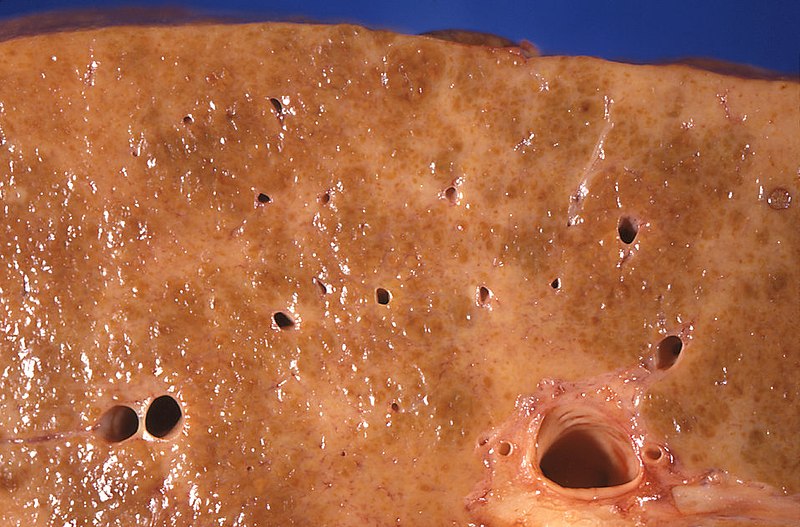
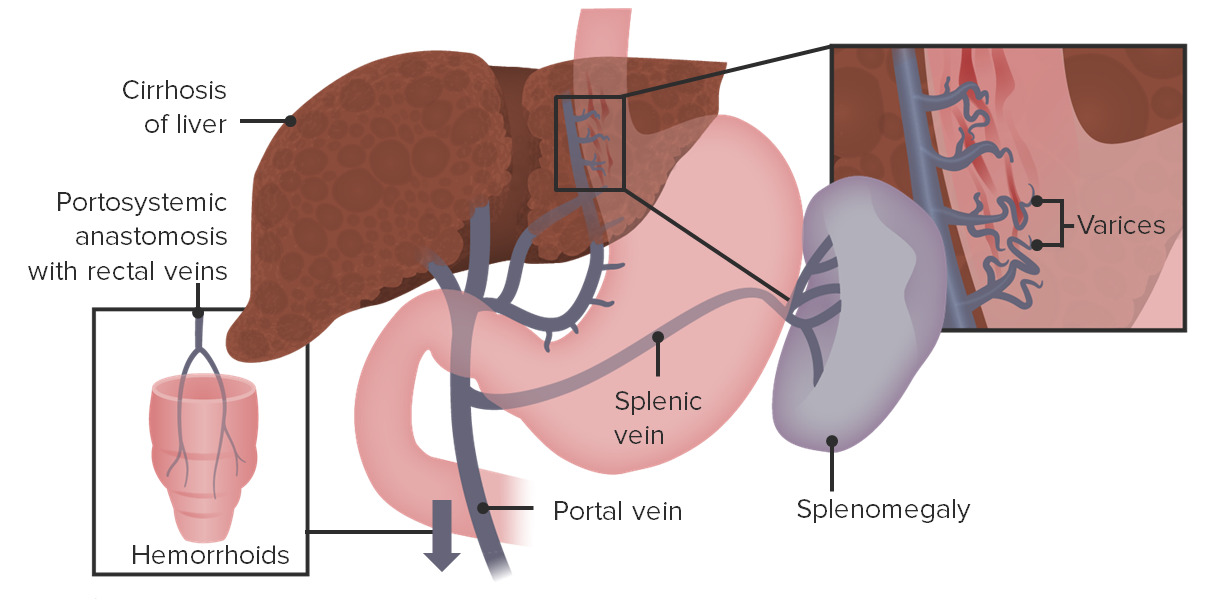
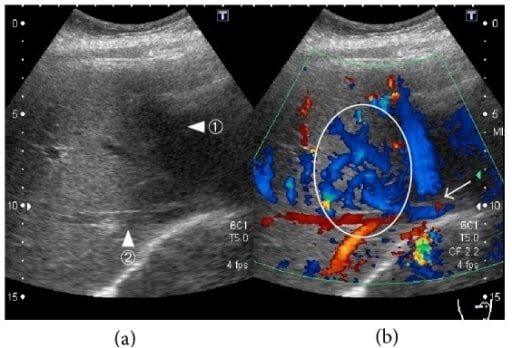
00:01 Here we have varices. 00:03 Esophageal varices to you, first, first place that you’re going to turn to for pathology in the origin of esophageal varices would be the liver, okay? Now, before we get there, what’s going on and what you’re going to find in your esophagus? Varices means dilation of the veins, esophageal veins. They’re known as the cardiac veins and… make sure that you know from anatomy your portocaval anastomosis. 00:31 Three different and I like the pneumonic, it’s cute: Head-Butt-Caput. 00:35 Head - esophageal varices; region, obviously not the head. 00:41 Head region, esophageal varices. 00:44 Butt - hemorrhoids. 00:45 Caput - caput medusa. 00:48 These are the three major areas of porto - portal vein, caval - inferior vena cava, anastomosis. 00:55 These will be the areas in which, if your patient, in the liver, results in portal hypertension. 01:04 Close your eyes, think about the portal vein. 01:07 The portal vein - the splenic vein and the superior mesenteric vein will come together. 01:16 These two veins form the portal vein draining into the liver. 01:19 At any point in time, if there is obstruction of the portal vein draining into the liver such as cirrhosis, such as Budd-Chiari with hepatic vein thrombosis backing up or portal vein thrombosis. 01:35 You call this pre-hepatic portal hypertension, portal hypertension - hepatic, or post-hepatic portal hypertension. 01:43 Are you with me? From henceforth, portal hypertension, there are many differentials. 01:50 Don’t always think that it’s always cirrhosis. 01:53 Any time the journey of your portal vein to the liver, if it’s been impeded or result in portal hypertension, what happens? You increase your hydrostatic pressure in three different places - Head-Butt-Caput. 02:08 Are you with me now? Of all the three places, which one’s the emergency? It ain’t the hemorrhoids. 02:17 Its esophageal varices. 02:19 What happens? If this ruptures, your patient actually may suffocate on his or her blood. 02:26 No joke. 02:27 This is an emergency. 02:29 So all jokes aside, let’s get serious. 02:32 Portal hypertension is your point; most common cause of massive upper GI bleeding, high mortality, 30% within 2 weeks. 02:43 Serious. 02:45 Recurrent hemorrhage noted in 70%, one year. 02:50 Early endoscopy for diagnosis and treatment and beta-blockers, beta-blockers, beta-blockers, reduced the recurrent bleeding by 50%. 02:59 That is pretty impressive. 03:02 We’ll do an upper endoscopy here yet once again. 03:06 This time you’ll notice the following, you’ll notice that here that the esophagus not nice and smooth. 03:12 You got these bulges. 03:16 You could find a little bit of bleeding, that means that this is dangerous isn’t it because with the varices, it’s what’s actually happening here. 03:22 Why do you find the bulges? Because the esophageal veins, secondary to portal hypertension resulting in that increased hydrostatic pressure, is causing engorgement of the veins. 03:34 Hence the hemorrhoids, hence the caput medusa, hence the esophageal varices. 03:40 Here you can actually notice it on upper endoscopy. 03:43 This is an emergency. 03:45 Acute episode, resuscitation and correction of coagulopathy is important. 03:51 Esophageal varices. 03:54 Endotracheal intubation for airway protection. 03:56 No joke. 03:59 Endoscopic band ligation or sclerotherapy. 04:03 IV octreotide to decrease portal pressure. 04:08 Now, that portal pressure which is going to be for the most part, the next set of… the next couple of bullet points here, become important because remember the problem began at the level of the liver or in the region with the portal vein. 04:28 There’s something called the tube placement, known as the Blakemore. 04:32 And then you have TIPSS. 04:34 A TIPS procedure, or trans-jugular intrahepatic portosystemic shunt, is the intravascular placement of a device used to help decrease portal hypertension, most frequently used in patients with liver cirrhosis. 04:46 The shunt allows some portion of the blood to bypass the portal system, and return to heart without being filtered by the liver. 04:53 This decreases the volume of blood needing to pass through the portal system, ultimately lowering the portal pressure. The issue then becomes, how much blood can you allow to pass the filtration system before toxic metabolites like ammonia reach levels high enough to impact the brain, or hepatic encephalopathy. For this reason, the shunts can be dilated or constricted until a balance is found between portal blood pressure and effective blood filtration. 05:18 Recurrent hemorrhage, beta-blocker, 50%. 05:21 You are, you are exercising prophylaxis. 05:27 Variceal banding is also a helpful tool in decreasing the chance of recurrent bleed.
About the Lecture
The lecture Esophageal Varices by Carlo Raj, MD is from the course Esophageal Disease: Basic Principles with Carlo Raj.
Included Quiz Questions
A 40-year-old alcoholic patient presents to the emergency department with massive upper GI bleeding. He had a similar episode in the past. On examination, you notice signs of portal hypertension. His blood pressure falls to 85/45 mm Hg. In addition to ordering an endoscopy and starting fluid resuscitation measures, what would be the NEXT appropriate step in the management?
- Octreotide
- Digoxin
- Calcium channel blockers
- Chest X-ray
- Proton pump inhibitors
Which of the following medications/procedures would NOT be a treatment option for a patient with esophageal varices resulting from portal hypertension?
- Omeprazole
- β-blockers
- Intravenous octreotide
- Transjugular intrahepatic portosystemic shunt (TIPS)
- Sclerotherapy
A 32-year-old male comes to urgent care complaining of bloody vomiting. He states that he drank heavily at a party last night. He had similar episodes in the past. Which of the following would be the best prophylaxis for this patient?
- β-blockers and stopping binge drinking
- Blakemore tube placement
- TIPS procedure
- Sclerotherapy
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Very funny the way that he explains everything, make difficult concept very much easy to understand and with high yield information!!!