Playlist
Show Playlist
Hide Playlist
Esophageal Motility Disorders
-
Slides GIP Esophageal Motility Disorders.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
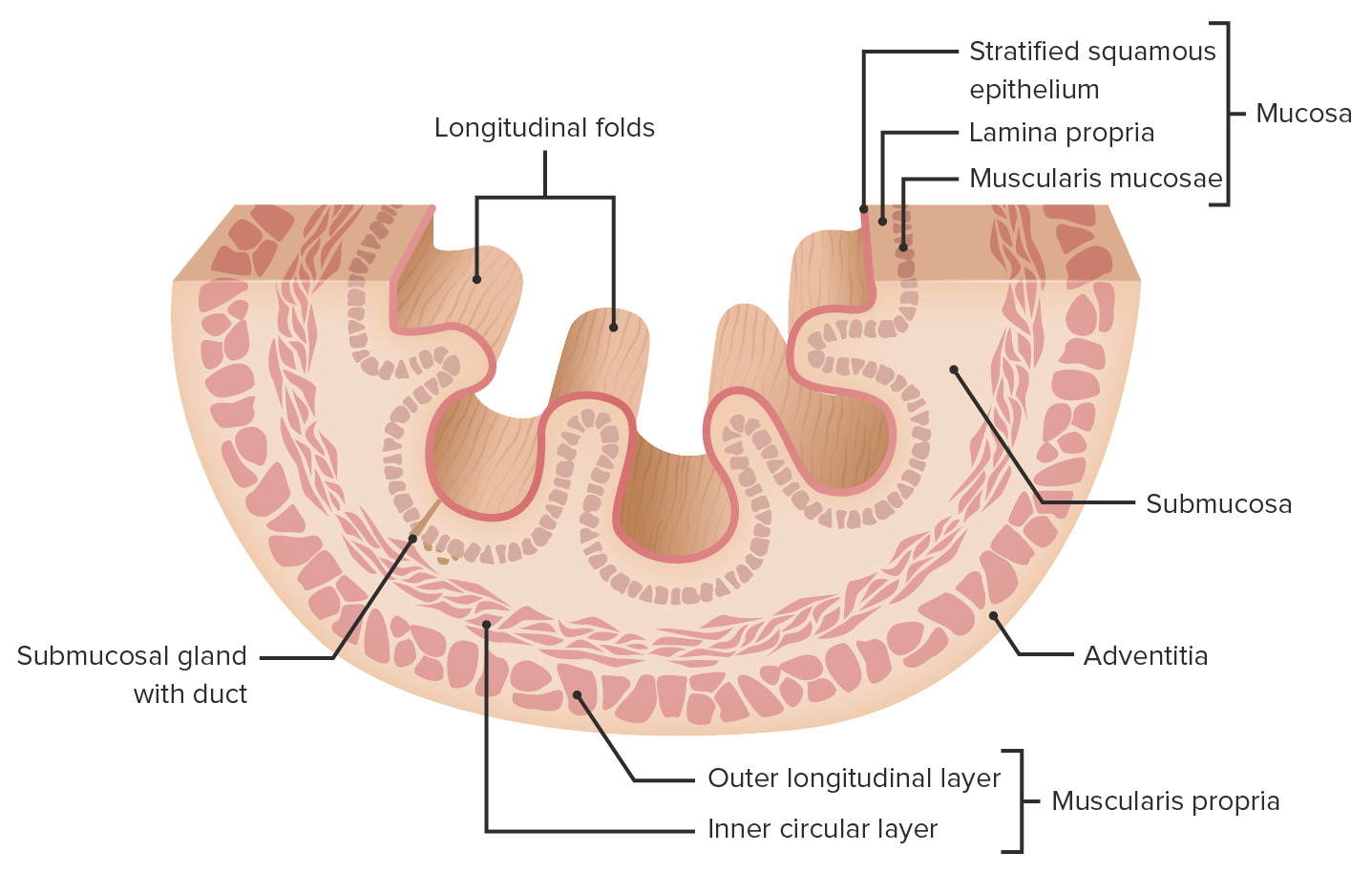
00:01 Welcome. In this talk, we're gonna cover esophageal motility disorders. 00:05 This is esophageal dysphagia. 00:07 Remember in a previous talk, we had covered oropharyngeal dysphagia and I promised you that we would come back and talk about things that occur more distally within the esophagus. 00:18 Here we are. Esophageal dysmotility can occur with three general mechanisms or flavors. 00:25 One is diffuse esophageal spasms. One is scleroderma and one is achalasia. 00:31 And these all have slightly different etiologies, different manifestations, and different treatments. 00:37 But they are all within the spectrum of esophageal dysmotility. 00:42 Let's first look at diffuse esophageal spasms. 00:45 To understand this, we just have to understand how the esophagus normally carries a peristaltic wave from the oropharynx into the stomach. 00:54 So diffuse esophageal spasms defined as you see here, are hyperdynamic and non-propulsive contractions of the esophagus. 01:01 And you can think of it as just random squeezing here and there along the esophagus without getting a nice peristaltic wave from top to bottom. 01:11 Pathophysiology of diffuse esophageal spasms are not entirely understood. 01:16 In many cases, the etiology is completely unknown, otherwise, called idiopathic. 01:22 The pathophysiology is also not fully understood but we can still get a general idea what's going wrong. 01:30 So esophageal smooth muscle tone. 01:32 The movement of a bolus of food from top to bottom requires a combination of normal sympathetic innervation which is cholinergic in nature, causing smooth muscle contraction. 01:44 However, we also have to have smooth muscle relaxation in a coordinated fashion and that's provided through the vagus nerve, parasympathetic stipulation that causes smooth muscle relaxation. 01:56 And you need a coordinated wave of contraction, relaxation, contraction, relaxation, all along the entire segment. Otherwise, you get spasm. 02:05 So esophageal spasm can occur due to impaired parasympathetic innervation. 02:12 That means that we're not relaxing appropriately. 02:15 This can happen due to diminished nitric oxide production which is actually in the mechanism by which we get the smooth muscle cell relaxation. 02:23 Inflammation can actually by increasing the production of a variety of inflammatory mediators will cause constriction or we may just have hypertrophy of esophageal smooth muscle which can occur for a variety of reasons, including just increased chronic intraabdominal pressures. 02:43 So as a result of this, the esophageal spasms manifest as frequent high-pressure non-peristaltic, so just random spasms of contractions that occur spontaneously. 02:56 The clinical presentation may be asymptomatic. 02:59 There may be patients who have this going on at a low level and not know about it. 03:03 Alternatively, there may be spontaneous but intermittent non-progressive dysphagia. 03:09 Just maybe it's difficult to swallow, it comes and it goes, don't know what causes it. 03:14 You may have angina-like chest pain, so spasms can actually directly manifest with prolong spasm as a chest pain. 03:22 Things may be aggravated by hot or cold. 03:25 So hot or cold can actually cause spasm or abnormal relaxation in an uncoordinated fashion. 03:33 And you may have associated gastroesophageal reflux disease. 03:37 So having the spasm may actually impact the ability to move gastric contents in a forward direction. 03:46 You may have retrograde bathing of the lower esophageal sphincter. 03:50 The diagnosis is made on manometry for the most part. 03:54 You assess the clinical diagnosis but to confirm it, you put in a manometer to measure pressures down the esophagus. 04:00 And what you will see is a multi-peak high-pressure contractions randomly along the entire esophageal segment. 04:08 There will be intermittent normal peristalsis. 04:11 So for a while, it may function exactly the way it's supposed to. 04:15 And then, at other times, these abnormal spontaneous random contractions. 04:20 And in most cases associated with this spasm, the lower esophageal sphincter tone is normal. 04:28 On a barium study, an upper GI study, you can see these random contractions. 04:33 So instead of having a nice, smooth tube of the esophagus, we have these kind of indentations throughout reflecting this random contraction of the smooth muscle along the length of the esophagus. 04:46 How do we manage this? So we're mainly trying to give symptomatic relief. 04:51 If there's pain, if there's gastroesophageal reflux disease, we really want to minimize that, so we can give a variety of agents that will relax the esophageal smooth muscle. 05:01 Peppermint oil is a good one. 05:03 We can give calcium channel blockers which will also cause relaxation of the esophagus. 05:08 Proton pump inhibitors will limit the reflux symptoms, the heartburn that may accompany this and if it's really severe, we can actually give localized botulinum toxin injections to reduce the lower esophageal sphincter tone for any of the refractory disease. 05:27 So that's diffuse esophageal spasm. Let's talk about scleroderma. 05:30 Another calm - another reasonably common cause of esophageal dysmotility. 05:36 So scleroderma is actually a systemic autoimmune disorder. It can affect the esophagus. 05:41 It also affects a lot of other areas in the body as we will see. 05:45 It causes atrophy and scarring, so sclerosis, hence the name sclero of the esophagus. 05:51 It also causes scarring and fibrosis of the skin where it gets its main name, scleroderma. 05:57 There will be diminished or even absent peristalsis as the esophagus becomes a stiff pipe of scar. 06:04 And the lower esophageal sphincter is also affected. 06:07 It becomes a stiff pipe and can't squeeze to close. 06:11 So you'll get massive reflux. So you have reduced LES tone. 06:15 The pathophysiology of this, it's an autoimmune disease. 06:18 So we don't really necessarily understand why the body decides to attack your own tissues. 06:25 But in this particular case, it attacks the tissues in the skin and the various other areas as well as the esophagus. 06:32 So we're looking at the typical esophagus in our patient. 06:34 There's mucosa lined by submucosa and then, a muscularis propria and adventitia. 06:40 In patients with scleroderma, they have abnormal autoimmune activation of T lymphocytes which will in turn, activate macrophages. 06:48 The macrophages and the lymphocytes make cytokines that cause the damage to the epithelium, to the smooth muscle cells in the esophagus and as a result of the ongoing inflammation, we will get scarring. 07:03 So we'll get atrophy of the epithelium and smooth muscle and we'll get a scar. 07:08 As a result of that, we have a stiff tube, so there's not any good peristalsis and the lower esophageal sphincter tone is diminished. 07:15 The clinical presentations. So the esophageal manifestations are one thing. 07:20 You get acid reflux. There's no LES tone. You get esophageal dysmotility. 07:24 You have a stiff tube without any peristalsis. 07:27 So it's difficult to continue a swallow and get food to move into the stomach. 07:32 So outside of the esophagus, there are a number of systemic manifestations. 07:38 Chief among these is skin thickening, hence the name of the disorder called scleroderma where you have the same autoimmune disorder affecting the skin and causing scarring. 07:49 Other places within the body they're affected include joints. 07:54 So we'll get abnormal calcium deposition and inflammation within joints. 07:58 So called calcinosis. We'll get Raynaud's phenomenon. 08:03 So the involvement of the autoimmune response of small vessels, typically, in the extremities and typically, within the phalanges or fingers and toes leads to abnormal sensitivity to various extrinsic factors such as cold and the vessels will spontaneously constrict which will cause loss of flow to the distal digits. 08:26 As a result of that, you will get cyanosis and you get pain. This is Raynaud's phenomenon. 08:33 Patients also get esophageal dysmotility. So we're actually spelling out a pneumonic. 08:37 So you can keep track of what happens in scleroderma. So we have C, R and E so far. 08:43 The S is sclerodactyly. 08:46 The scarring in the fingers like we see within the skin throughout the body but within the fingers in particular causes a progressive contracture of the fingers, so you get sclerodactyly and kind of a diffuse thickening and scarring of the fingers so that it becomes - the hand becomes relatively useless. 09:06 And you can get telangiectasia, so prominent vasculature in areas where we have the scarring occurring with the inflammation. 09:13 So C-R-E-S-T is CREST. CREST syndrome, although it sounds really bad with all of these different involvements of different parts of the body, CREST manifestations usually portend a reasonably good diagnosis. It's less severe disease. 09:32 So that's CREST syndrome. So other systemic manifestations of scleroderma. 09:40 You can have scarring that involves the lung parenchyma, so interstitial lung disease or scarring that involves the pulmonary vasculature leading to pulmonary hypertension and right heart failure. 09:52 You can have involvement of the pericardium of the heart, leading to a constriction around the heart and a constrictive physiology. 10:02 You can have renal disease and that's what's being demonstrated here. 10:08 That glomerulus is showing focal and segmental glomerulosclerosis. 10:12 So scarring that can also involve the kidney leading to renal failure. 10:17 So a lot of systemic manifestations. 10:20 Making the diagnosis for scleroderma involves a number of laboratory tests in addition to the clinical findings that we've just discussed. 10:29 So the laboratory tests include Anti-Scl-70. It's an autoantibody. 10:35 It's an antinuclear antibody that happens to be against the topoisomerase. 10:40 So something that helps to unwind DNA that occurs in about 20% of patients. 10:44 You can have anti-centromere antibodies. 10:47 Again, an antinuclear antibody directed against the centromere. 10:50 And that will occur in up to 95% of CREST patients. 10:53 Remember that CREST tends to give you a better prognosis overall. 10:57 And then, you can have Anti-RNA polymerase III autoantibodies that occur in about 20% of patients with scleroderma and that's usually bad news and the patient is going to do less well overall. 11:11 In terms of evaluating what's going on in the esophagus, remember, this is a talk about esophageal dysmotility. 11:18 We will wanna look and see that there will be diminished lower esophageal sphincter tone on manometry and that there won't be any peristalsis in the body of the esophagus. 11:28 Endoscopy, we can see the manifestations of that LES sphincter being relaxed. 11:33 We have a reflux esophagitis. We may have Barrett's metaplasia. 11:37 We may also have longstanding inflammation and scarring related to the gastric acidity and even have an esophageal stricture. 11:45 So how are we gonna take care of these patients with scleroderma? Well, we're gonna try, you see the last one. 11:51 Manage their autoimmune disease with immune suppression. 11:56 But we're also wanna give our patients symptomatic relief. 11:59 So we will give them proton pump inhibitors to reduce gastric acidity. 12:03 If there are strictures related to chronic reflux, we will do endoscopic dilation. 12:08 And for refractory GERD, we may do fundoplication. 12:12 We've talked about that in other kind of discussion associated with esophageal abnormalities. 12:18 Finally, one last flavor of esophageal dysmotility and that's achalasia. 12:25 An achalasia is esophageal dysfunction, dysmotility due to neurogenic causes. 12:32 There is absolutely or very diminished peristalsis and the lower esophageal sphincter cannot relax. 12:40 That means you end up with a big, huge, dilated mega esophagus and with that dilation and chronic inflammation associated with that, there's an increased risk of esophageal malignancy. 12:55 So the pathophysiology of this, it's idiopathic in the vast majority of cases. 13:00 Meaning we haven't got a clue. 13:02 However, it can be due to malignancy. It can be due to trauma, surgery, Chagas disease. 13:07 It could be due to radiation. So there are a number of things that can cause this. 13:11 And interestingly, Chagas disease, that infection, with that organism leads to an interesting predilection for going for the nervous system of the esophagus. 13:24 So that nervous system of the esophagus is Auerbach's plexus and this is a kind of a nervous innervation that allows us to have a well-controlled, well-structured peristaltic wave that goes from top to bottom. 13:39 And that Auerbach's plexus is very important to stimulating the smooth muscle to give us relative waves of contraction and relaxation. 13:46 And we're gonna see here on this slow motion of a bolus of food coming down the esophagus that we normally have a nice, controlled, peristaltic wave that moves things in one direction from top to bottom with relaxation of the lower esophageal sphincter and viola, into the stomach. 14:08 On the other hand, with achalasia where we have degeneration of the ganglion cells in Auerbach's plexus, we don't have that nicely coordinated smooth muscle relaxation and contraction. 14:20 We get this one instead which is a version of abnormal dysmotility where the primary problem demonstrated here is a lack of relaxation of the lower esophageal sphincter and we get things bound up at that point. 14:42 With recurrent amounts of food coming down, we get a mega esophagus with a very narrowed, poorly-relaxing lower esophageal sphincter. 14:54 So how do we - how do we see the manifestations of this in our patients? So there would be dysphagia, difficulty swallowing that with those symptoms becoming worse and worse overtime. With inability to eat appropriately, there will often be weight loss and with obstruction at the point of the lower esophageal sphincter, we'll get regurgitation of undigested food. 15:17 The diagnosis is made on endoscopy and/or on Barium swallow. 15:23 So we can do esophageal manometry to look at the tone of the esophagus and the lower esophageal sphincter. 15:31 The Barium esophogram as you see here is absolutely classic. 15:35 You see a markedly dilated, distended mega esophagus. 15:39 I like just saying mega esophagus with a very narrowed lower esophageal sphincter at the point of the green arrow, so called "bird beak" sign. 15:48 We want to do endoscopy with biopsy to rule out other causes such as cancer at that point or Chagas disease with infection. How do we manage this? Well, basically, the problem is we can't get things through the lower esophageal sphincter, and so we want to reduce the tone of that. 16:08 We can mechanically stretch the muscle fibers. 16:10 We can put in a balloon and blow it up, and dilate, and that will often give symptomatic relief for a significant period of time. 16:18 If necessary, we can go in and surgically cut the smooth muscle so that it will scar in an open position, a so called surgical myotomy. 16:27 We can also try to do pharmacologic intervention. 16:30 So botulinum toxin to reduce the lower esophageal sphincter tone, oral nitrates, or calcium channel blockers are also effective in some cases. 16:41 With that, we've covered a lot of territory with the inability of the esophagus to move a wave of food, esophageal dysmotility.
About the Lecture
The lecture Esophageal Motility Disorders by Richard Mitchell, MD, PhD is from the course Disorders of the Esophagus.
Included Quiz Questions
What is NOT a finding consistent with diffuse esophageal spasms?
- Symptoms improving with very cold liquids
- Spontaneous, intermittent, nonprogressive dysphagia
- Angina-like chest pain
- Symptoms worsening with hot liquids
- Being associated with GERD
What finding is consistent with diffuse esophageal spasms on barium esophagram?
- A "corkscrew" pattern
- A diffuse outpouching
- "Bird's beak" esophagus
- A lack of contrast below the upper esophageal sphincter
- A lack of contrast below the lower esophageal sphincter
What causes scleroderma?
- Immune system attacking the esophagus
- Increased compliance of the esophagus
- Necrosis of the esophagus
- Metaplasia of the esophagus
- Metaplasia of the stomach
What is NOT a typical symptom of scleroderma?
- Elevated hemoglobin
- Acid reflux
- Raynaud phenomenon
- Skin thickening
- Calcinosis
What is found on manometry in a patient with scleroderma?
- Decreased LES tone
- Increased peristalsis in the body of the esophagus
- Increased UES tone
- Hypermotility
- Esophageal spasms
What is NOT a typical treatment for esophageal dysmotility due to scleroderma?
- mTOR inhibition
- Proton pump inhibitors
- Endoscopic dilation
- Fundoplication for refractory GERD
- Immune suppression
What is the most common etiology of achalasia?
- Idiopathic
- Viral
- Autoimmune
- Myositis
- Bacterial
What is found in barium swallow in achalasia?
- "Bird's beak" esophagus
- A "corkscrew" pattern
- A lack of contrast below the upper esophageal sphincter
- A lack of contrast above the lower esophageal sphincter
- Steeple sign
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |