Playlist
Show Playlist
Hide Playlist
Epilepsy and Febrile Seizures
-
Slides 09 Seizures Neuropathology I.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
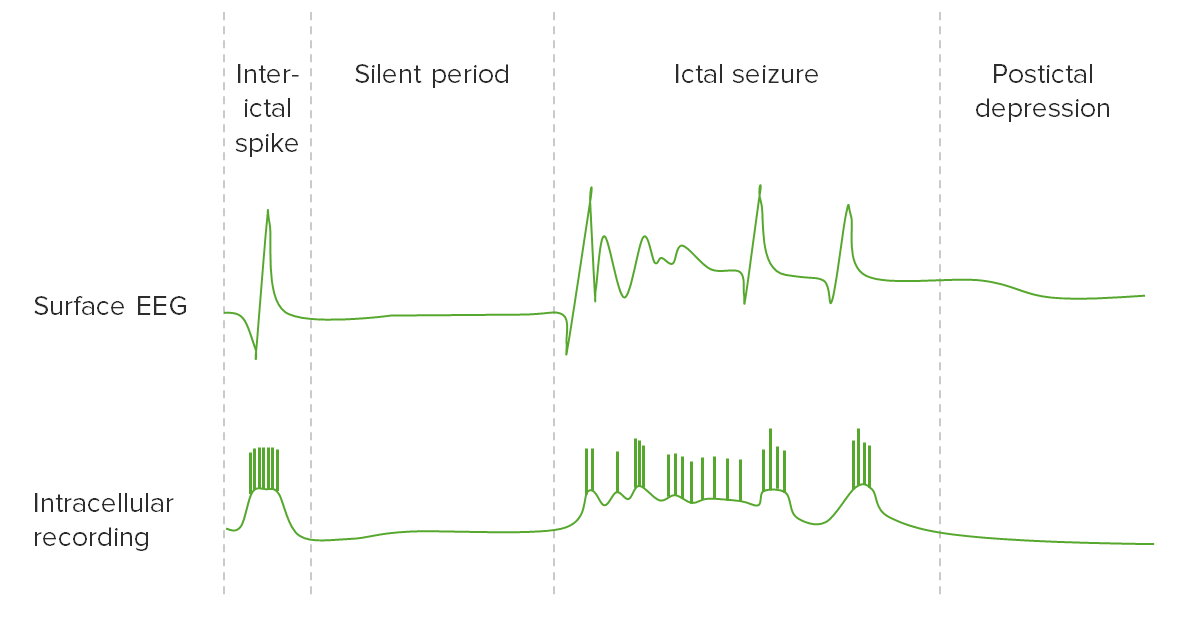
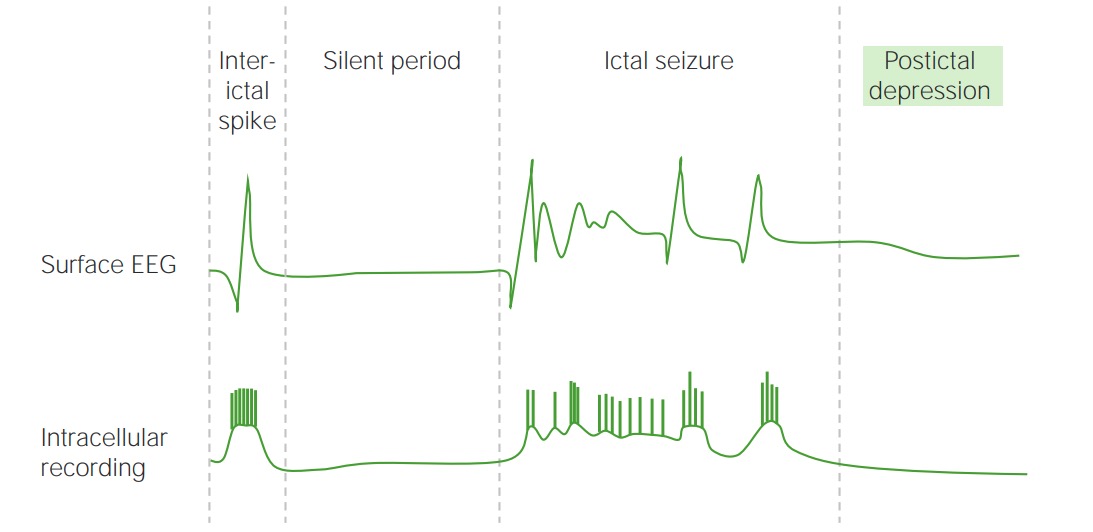
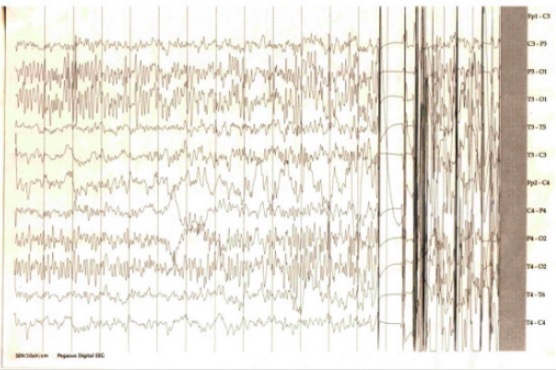
00:01 Let’s talk about epilepsy. 00:04 So with epilepsy, what does it mean? It means that you have unprovoked seizures. 00:08 I’ll give a general definition. 00:10 And what’s a seizure? A hypersynchronous type of electrical activity of the brain. 00:14 Hypersynchronous. 00:17 Risk factors. 00:18 TORCH. 00:19 Toxoplasma, Rubella, Cytomegalovirus, Herpes, so on and so forth. 00:25 Prematurity. 00:26 Hypoxic ischemic injury at birth. 00:30 So anything that may result in ischemia to the fetus could be a problem. 00:34 Family history of seizures. 00:36 History of febrile seizure as a child, that’s important, okay? We’ll talk about febrile seizure and when we do so, we’ll be focusing upon children. 00:45 History of meningitis or encephalitis or perhaps even head trauma. 00:49 These are risk factors for unprovoked seizures, epilepsy. 00:55 Epidemiology: Up to 10% of population will have seizures in their lifetime. 01:00 So that’s actually quite high. 01:02 10% is no joke in the U.S. 01:04 After one unprovoked seizure, there is a 30% chance that there might be second one. 01:10 That’s all part of epilepsy. 01:13 1% of the population has epilepsy itself. 01:16 So 10% could actually have a seizure. 01:19 1% could go onto epilepsy, whatever type. 01:22 The incidence in new onset seizure is highest among the very young and the very old. 01:27 Extreme, extremes of age. 01:31 Etiology of seizure varies – A lot of your seizure and a lot of your epilepsy, the etiology is unknown. Let’s talk about febrile seizures. 01:41 What does febrile mean to you? This is a fever. 01:44 The most common cause of new onset seizure in a child. 01:49 That’s what you want to know. 01:49 Typically occurs between the age of six months and five years. 01:56 So once again here, the clinical pearl is that the child has a fever and then they go onto his or her first hypersynchronous seizure. 02:07 Occurring in the setting of a febrile illness. 02:08 With that evidence of intracranial infection. 02:10 So there is no meningitis or whatever so we’re not saying a fever or an infection due to or from meningitis. 02:18 It could just be a fever that existed. 02:21 Unfortunately, resulting in a new onset seizure. 02:24 It can occur before the fever's even noticed. 02:27 Typically, generalized at onset. 02:31 And maybe recurrent with future fevers and the fever itself will then be the provoking portion. 02:40 So let me ask you something. 02:43 Would you call this epilepsy? Good. 02:46 You would not. 02:47 Because epilepsy, by definition, is unprovoked seizure. 02:52 If we or you as a doctor are able to establish that the trigger for the seizure in your child was fever, then you call it febrile seizure, period. 03:03 Is that clear? Child, fever, seizure, febrile seizure. Done. 03:09 Give me clinical pearls for everything that you need to know here about seizures in general. We typically have a benign prognosis. 03:19 Thank goodness. This is a child. Focal onset. Prolonged. 03:25 Other neurologic abnormalities could be present. 03:27 And family history of epilepsy could be present. 03:31 There is a rather small percentage of these febrile seizure patients that might go onto future epilepsy, which then would mean what? Unprovoked. Management: Obviously, treat the darn fever, please. 03:47 And what about these antiepileptics that we’ll talk about in greater detail? It should only be used if the seizures are prolonged or the fever cannot be controlled and the seizures continue to be problematic. So in other words, if you find that the seizures cannot be controlled and they do not go away by managing that fever, then at this point, you need to unfortunately look into your supply of antiepileptics.
About the Lecture
The lecture Epilepsy and Febrile Seizures by Carlo Raj, MD is from the course Seizures. It contains the following chapters:
- Epilepsy
- Febrile Seizures
Included Quiz Questions
What is a TRUE statement regarding childhood seizures?
- Febrile seizures are not defined as epileptic seizures.
- Febrile seizures typically occur between ages 6 and 10.
- Febrile seizures usually require anticonvulsant medications.
- Febrile seizures never progress to epilepsy.
- Prematurity is not a risk factor for epilepsy.
What increases the risk of progression to epilepsy in a child with febrile seizures?
- Family history of epilepsy
- Generalized seizures
- Onset before the age of 6 months
- More than one febrile seizure
- Delivery after their due date
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
1 customer review without text
1 user review without text