Playlist
Show Playlist
Hide Playlist
Work Up of APE and CHF in the Emergency Department (ED)
-
Emergency Medicine Bord Pulmonary edema and CHF.pdf
-
Download Lecture Overview
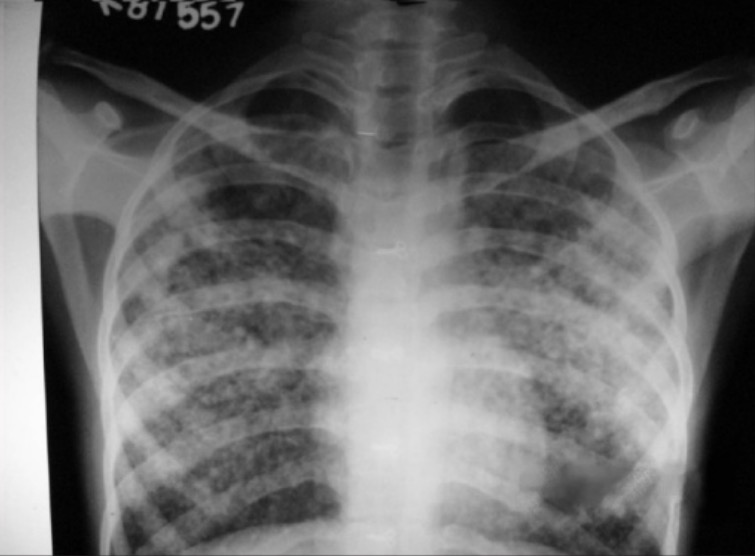
00:01 Now, while we’re simultaneously getting history and evaluating our patient, we also wanna be thinking about what additional testing we should do. 00:09 So we wanna send off some labs. 00:11 We’re gonna send of our basic lab work: A CBC, a metabolic panel, and then we’re also gonna wanna send off a troponin test to see if there’s been any evidence of decreased blood flow or strain on the heart and sometimes we also wanna send off a pro-BNP. 00:26 The pro-BNP is a test that it gets elevated when there’s been stretching of the heart and this is a test that generally gets elevated in patients with heart failure. 00:36 The key thing to remember about pro-BNP is that it may be helpful to have a baseline for the patient. 00:43 So a baseline number or value for where the patient normally lives because this number can potentially be chronically elevated in patients with heart failure. 00:52 It’s chronically elevated in patients who have renal failure who are on dialysis so you wanna have a level to compare to. 00:58 The number itself just by itself may not necessarily be beneficial. 01:03 You also wanna get an EKG. 01:06 The EKG is gonna help evaluate for ischemia. 01:09 Again, one of the common causes here for heart failure is that the patient has had a decrease in their ejection fraction which could happen in a situation of a heart attack, so the EKG will help screen for that. 01:20 It can also look for arrhythmias. 01:22 So sometimes if the patient has atrial fibrillation or another arrhythmia that can sometimes also lead for the patient developing worsening heart failure. 01:32 You also wanna get a chest x-ray. 01:35 The classic chest x-ray in heart failure and pulmonary edema is pictured here. 01:40 Basically, what it would look like is that it look like diffused kind of an infiltrative pattern, the vessels are gonna be very prominent on the chest x-ray and potentially you might also see fluid in the lungs like a pleural effusion or you may see what we call fluid in a fissure which will look like a white line where the fissure of the lung is located. 02:00 You also can get an echocardiogram. 02:04 Echocardiogram can be performed by the emergency medicine physician or are generally good at looking whether or not the ejection fraction is good, medium or bad. 02:15 It can also look for regional wall motion abnormality. 02:18 So is there a certain portion of the heart that’s not moving as well? Then in another portion of the heart that can also indicate possible ischemia or myocardial infarction. 02:28 So when we talk with this lady further and we get some additional history from the patient and her family, we find that she’s in severe respiratory distress and has a history of congestive heart failure. 02:40 She’s been eating pizza for dinner and not really being very compliant with her diet and she knows also that she’s had some orthopnea and has been sleeping on an increased number of pillows over the last 2-3 days. 02:52 Chest x-ray further reveals pulmonary edema so we go ahead and we treat her with the appropriate medication, we start her on noninvasive ventilation, we gave her nitrates in a form of IV nitroglycerin and we also gave her some diuretics. 03:06 And this patient quickly turns around and is doing better when she is admitted to the hospital from the emergency department.
About the Lecture
The lecture Work Up of APE and CHF in the Emergency Department (ED) by Sharon Bord, MD is from the course Respiratory Emergencies.
Included Quiz Questions
Which of the following is not a necessary work-up for acute pulmonary edema in the emergency department?
- Pulmonary artery catheterization
- Troponin
- Pro-BNP
- Echocardiogram
- Electrocardiogram
Which of the following statements regarding the diagnostic tools in heart failure is INCORRECT?
- A chest x-ray is not very helpful in cases of heart failure.
- Pro-BNP may be unreliable if no baseline result is available.
- Pro-BNP is elevated in patients with heart failure.
- An electrocardiogram will help evaluate presence of ischemia or arrhythmia.
- An echocardiogram helps determine if the ejection fraction is good, medium, or bad.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |