Playlist
Show Playlist
Hide Playlist
Deep Vein Thrombosis: Pathogenesis
-
Slides 10 VascularMedicine advanced.pdf
-
Reference List Vascular Medicine.pdf
-
Download Lecture Overview
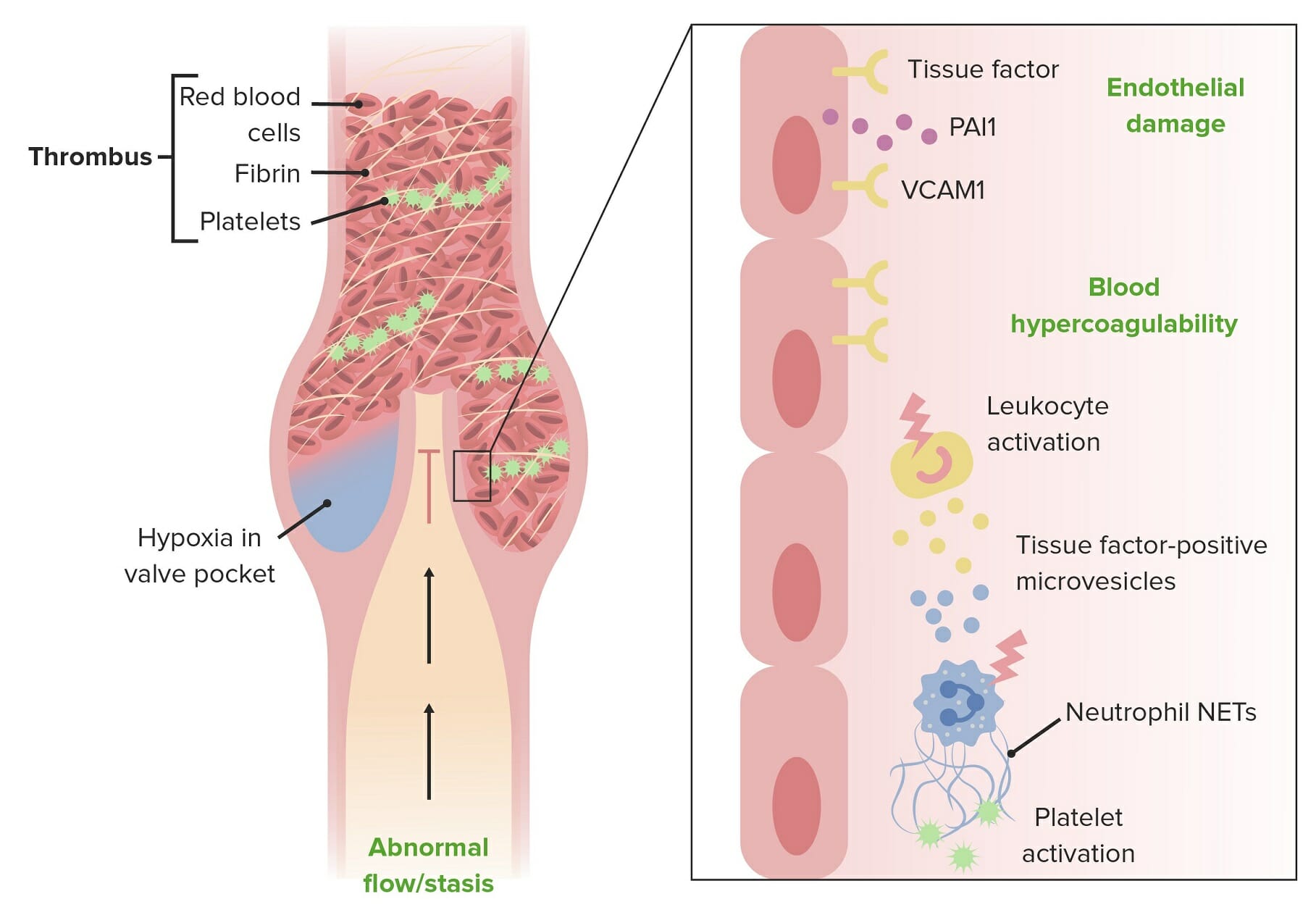
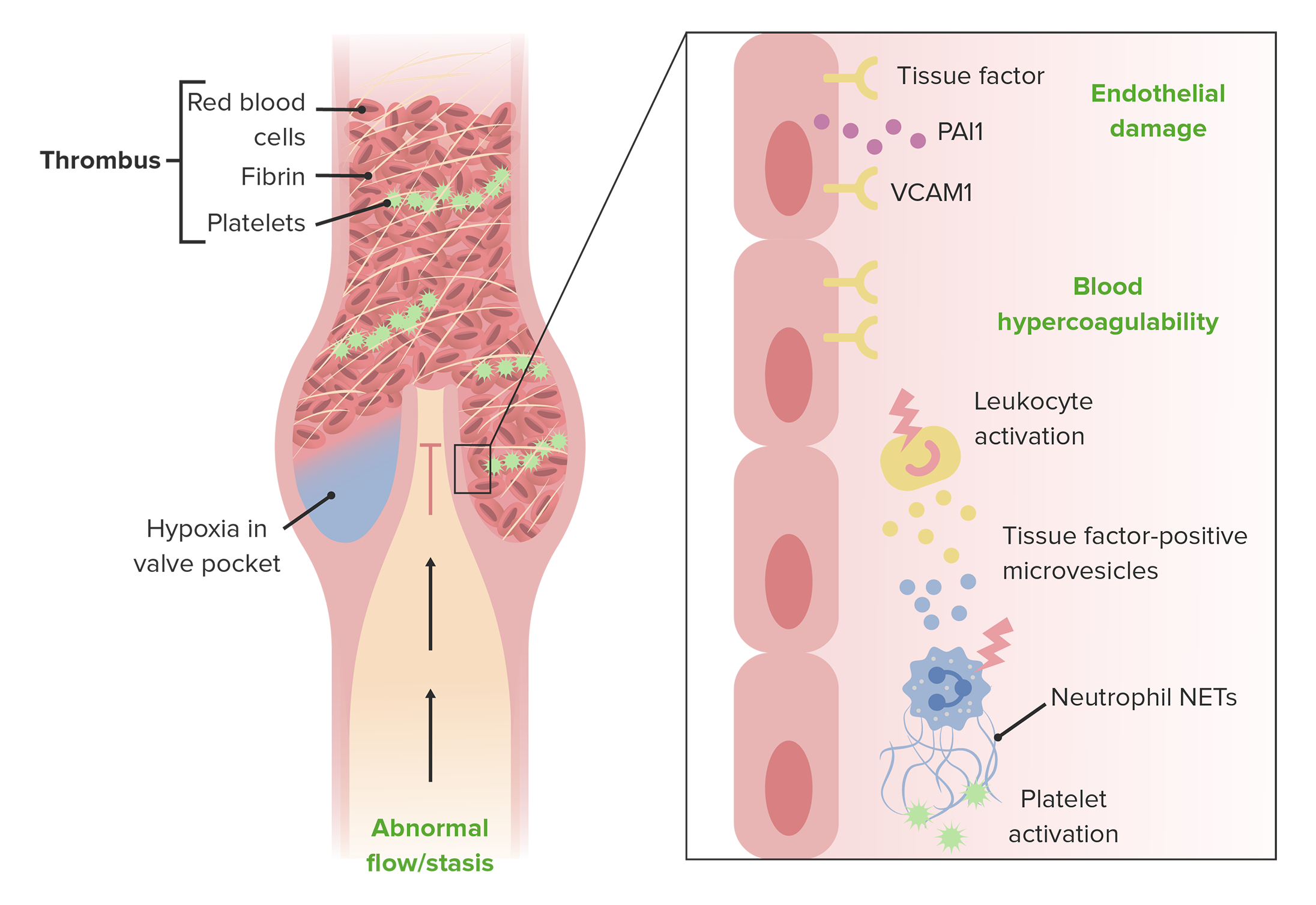
00:00 A little bit about the pathogenesis: You've seen this slide before. As you heard, 90% of DVTs and pulmonary emboli occur in the veins of the leg. Often, they start as very small clots in the popliteal vein, and often, they will dissolve and heal without any problem. 00:20 But once they get up into the femoral vein, which is a lot of people—you see, 42% of people—there is a greater likelihood of the clot growing. And then you can see, once it gets up into the common femoral vein or the iliac vein, inferior vena cava, there's a very significant chance that a large mass of clot will embolize to the lung and might prove to make the patient either very sick or even die. Just to emphasize one more time: The consequences of venous thromboembolism—pulmonary embolism—can be fatal. It can cause a very serious illness, acute morbidity. Once you've had one, you're at high risk for more. Thrombophlebitis itself, as you know, can lead to the postthrombotic syndrome, with edema and ulcers and, in a rare case, even amputation. So thrombophlebitis is defined as the presence of a thrombus in the vein. It's accompanied by inflammation in the vessel wall. It can happen, of course, in superficial or deep veins. The dangerous one is one that occurs in deep veins, not in the superficial veins. Of course, the danger is pulmonary embolism, and we've already talked about all the things that can lead to deep venous thrombosis, including long periods of sitting or standing, or a long plane trip. We've also already mentioned the postthrombotic syndrome. This is a long-term complication of DVT and venous insufficiency, where the internal veins are not working well. The valves are not working. Blood pools. The vein dilates. There's a great tendency for a blood clot to form. Edema forms. There's poor skin nutrition, and often, ulcers develop. The blood proteins and other blood products (hemoglobin) are deposited in the tissues, giving a brown discoloration, and the ulcers can be exceedingly difficult to heal, taking many months to heal with constant therapy. 02:28 Again, just to reiterate for how common DVT is: Patients in the United States in one year will have clinically evident venous thromboembolism—a total of 900,000 patients. And the deaths there are about… that are due to pulmonary embolism are about 300,000. And the annual incidence of venous thromboembolism increases by age and sex, as you can see in the graph. 02:58 Particularly as patients get above age 55 to 65, there's a marked increase in venous thromboembolism. Males a little more than females, but not very, very much difference. 03:11 Again, a huge increase. This data comes from the Worcester Vein Study in Worcester, Massachusetts. 03:19 The University of Massachusetts Medical Center has been studying all cases of DVT/PE in Worcester County over many years. The symptoms: I think we've already talked
About the Lecture
The lecture Deep Vein Thrombosis: Pathogenesis by Joseph Alpert, MD is from the course Venous Diseases.
Included Quiz Questions
When discussing the pathogenesis of a DVT, which of the following statements is correct?
- Post-thrombotic syndrome is a long term complication of a VTE.
- The more proximal the clot, the lower the likelihood of a substantial embolism occurring.
- Once a patient has successfully cleared their thromboembolism, they are unlikely to have a recurrence.
- Thrombophlebitis caused by a DVT is most dangerous when involving superficial veins.
- DVTs most commonly occur in the upper extremities.
A patient is recovering from a recent DVT. She notices some discoloration and swelling in the affected leg that does not seem to be resolving. What should she be told regarding post-thrombotic syndrome?
- Her condition is relatively common, occurring in 25-50% of patients with a DVT.
- The unresolved swelling is exceedingly rare after suffering a DVT.
- If she develops an ulcer in this area, it will likely heal quickly.
- Varicose veins are not associated with this condition, as they occur in superficial veins rather than deep veins.
- Even if her symptoms persist, they are unlikely to impact her mobility or quality of life.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
It´s a really good video, enough infomration and a easy way to understand it.