Playlist
Show Playlist
Hide Playlist
Decompensated Cirrhosis with Case
-
Slides Gastroenterology 13 Liver Pt3 End Stage Liver Disease.pdf
-
Reference List Gastroenterology.pdf
-
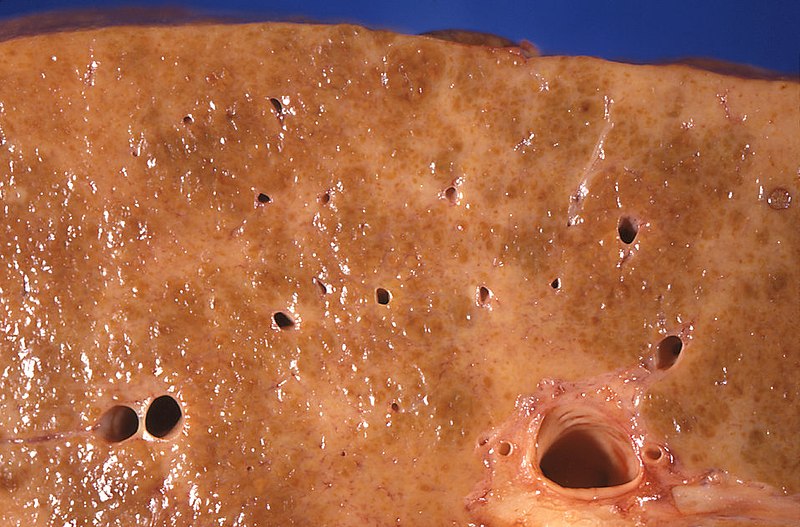
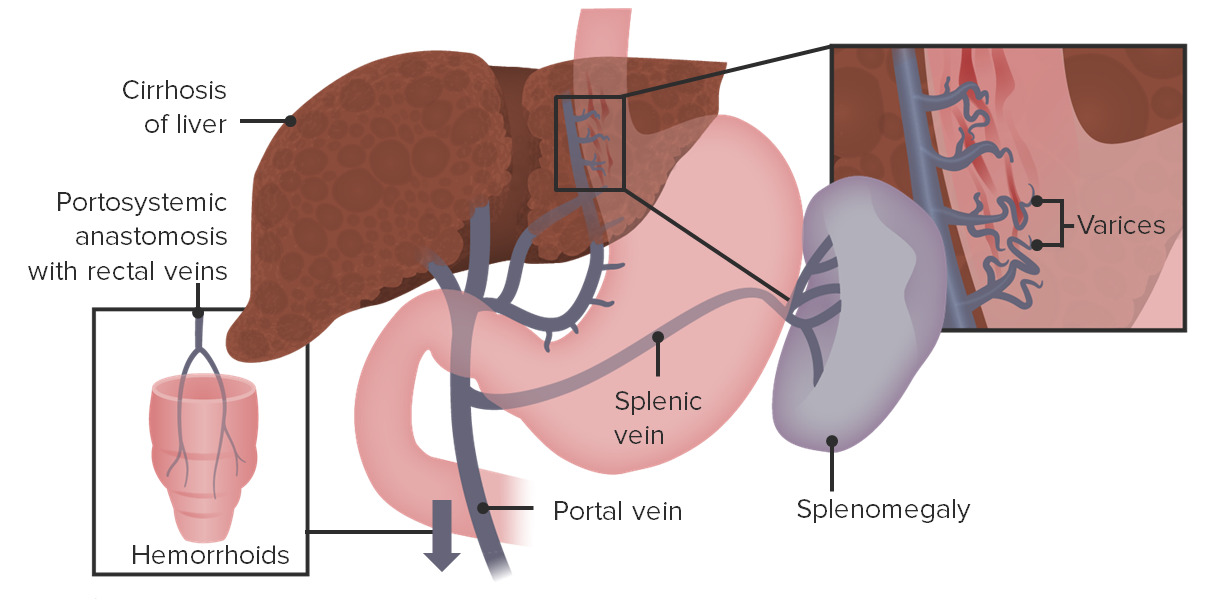
Download Lecture Overview
00:01 Let's move on to our next case. 00:03 A 48-year-old woman presents to the emergency department with one episode of bright red bloody emesis. 00:10 She has a history of alcohol-associated cirrhosis complicated by jaundice and ascites. 00:15 Her only medications are furosemide and spironolactone. 00:20 Vitals are notable for a blood pressure of 82/50 mmHg and heart rate 115 bpm. 00:25 She is disoriented. 00:27 Physical exam shows jaundice, spider angiomata, distended abdomen with a positive fluid wave and a firm liver edge palpated 3 cms below the costal margin. 00:38 Labs show a hemoglobin of 7.8 (g/dL). 00:41 IV fluid resuscitation is started. 00:44 So we are asked, what is the best next step in management? Let's go through some key features here. 00:51 She is presenting with hematemesis and she has decompensated cirrhosis. 00:57 In addition, on physical exam she has hypotension and tachycardia which we now know, indicates probably severe hypovolemia. 01:07 She has physical exam findings of cirrhosis and anemia on her labs indicating blood loss. 01:14 So, we mentioned the term "decompensated cirrhosis" What that means is there's an acute deterioration in the liver function in a patient with cirrhosis characterized by any of these things: so they may have new onset jaundice, they may have developed ascites or free fluid in the peritoneum, they may develop hepatic encephalopathy or confusion or coma related to the build up of toxins, they may develop hepatorenal syndrome which is a particular type of kidney injury that we'll discuss later, or they may present with new onset variceal hemorrhage, so bleeding from those dilated varices. 01:55 So, let's now review how cirrhosis leads to GI bleeding. 02:02 Recall that with portal hypertension, you have back up of flow and pressure into the portal systemic vessels. 02:09 So first, you may have back up of flow into the esophageal and gastric vessels leading to varices in those locations. 02:17 Next, you may also develop back up of flow into the splenic vein leading to enlargement of the spleen or splenomegaly. 02:25 And you may also have back up of flow into the rectal collateral vessels leading to hemorrhoids which can also present with GI bleeding. 02:36 So let's talk specifically about esophageal varices. 02:39 Patients often present with hematemesis and/or melena. 02:45 They can be very scary and that they can cause massive bleeding and so these patients require very urgent attention and stabilization. 02:53 Here on the right you can see an example of an upper endoscopy where you see very dilated tortuous vessels along the length of the esophagus, that's what varices appear like. 03:05 So the key elements of management are providing aggressive, supportive care. 03:09 So that's fluid resuscitation and/or transfusion if they meet the parameters. 03:14 You should then do upper endoscopy which can be diagnostic and therapeutic at the same time. 03:20 You should give vasoconstricting medications like octreotide which will reduce blood flow to the esophageal area and hopefully reduce the amount of bleeding. 03:31 And another important element of management is giving antibiotic prophylaxis, This is to prevent the high risk of infections like spontaneous bacterial peritonitis that can occur with GI bleeding. 03:44 We manage that by giving antibiotics like ceftriaxone or norfloxacin. 03:49 So now that we've reviewed that, let's return to our case. 03:53 A 48-year-old woman, who's now coming in with hematemesis. 03:57 We know that she has decompensated cirrhosis because of the presence of jaundice and ascites. 04:01 So knowing that, we should always be concerned for a variceal hemorrhage in a patient with these complaints. 04:07 In addition, she has signs of severe hypovolemia and physical exam findings of cirrhosis. 04:13 Note that she's already been started on IV fluid resuscitation. 04:17 So the best next step in management will be to start octreotide which is a splanchnic vasoconstricting medication. 04:24 and giving antibiotic prophylaxis for spontaneous bacterial peritonitis, giving a transfusion as needed and colon GI for an upper endoscopy. 04:35 Note here that although her hemoglobin was 7.8 (x10^9) and she doesn't quite meet that threshold of a hemoglobin less than 7 g/dL because she's actively bleeding and we know that esophageal varices can bleed very quickly, you would transfuse her before she hits that threshold.
About the Lecture
The lecture Decompensated Cirrhosis with Case by Kelley Chuang, MD is from the course Disorders of the Hepatobiliary Tract.
Included Quiz Questions
Which of the following is a possible complication of decompensated cirrhosis?
- Variceal hemorrhage
- Anal fissures
- Gastric ulcers
- Constipation
- Diarrhea
Which of the following is the best next step in the management of esophageal varices after initiation of IV fluids?
- Upper endoscopy
- CT of the chest
- Abdominal ultrasonography
- TIPS
- Liver transplant
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |