Playlist
Show Playlist
Hide Playlist
Cystic Fibrosis and ABPA
-
Slides 05 MajorAirwaysObstructionBronchiectasis RespiratoryAdvanced.pdf
-
Download Lecture Overview
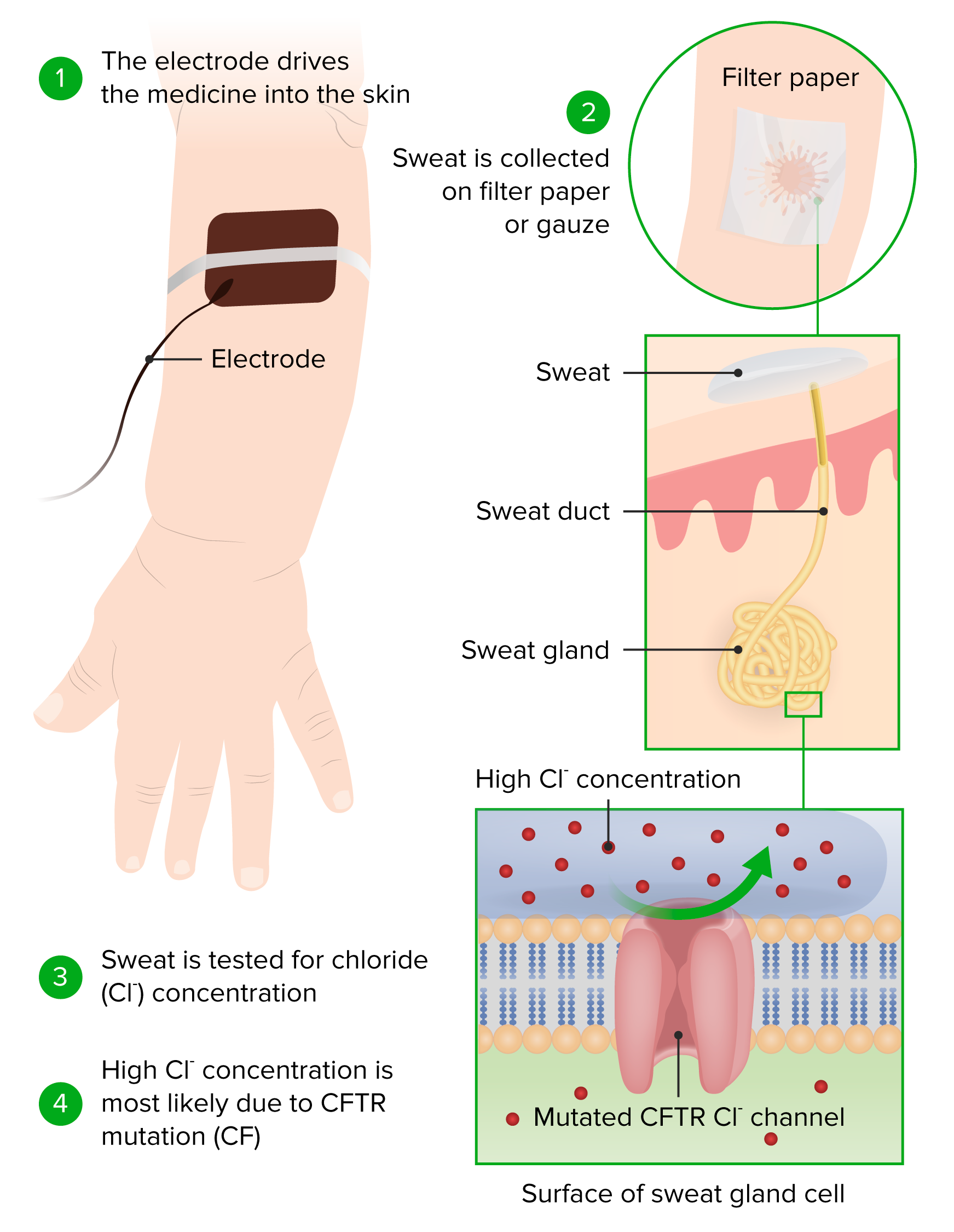
00:01 So I’m going to talk about a little bit about cystic fibrosis which is a very specific cause of bronchiectasis. Now this is a severe inherited genetic disorder. It is the commonest fatal genetic disease in the Western world. 00:14 It's present in 1 in 2000 to 3000 births. And what it causes is a progressive bronchiectasis with airways obstruction. Patients are universally colonized of Pseudomonas, they frequently have additional clinical problems, which I’ll describe in a short while, and most patients will end up dying over the cystic fibrosis when they are 40s or 50s. The cystic fibrosis, the genetics of this is an autosomal recessive disease, and it’s due to mutations of the cystic fibrosis transmembrane conductance regulator gene (CFTR), the CFTR gene. The CFTR is an ABC transporter protein that's present in the membrane of airway epithelium and exports chloride into the mucous. And when it’s not working, the mucous becomes much thicker and does not flow and that allows bacterial infection to occur within the lungs and bronchiole wall damage to occur and bronchiectasis to develop. There are a very large number of mutations, which have been identified as CFTR the cause of cystic fibrosis, but in fact, 60 to 70% of patients will have a problem with the deletion of the amino acid 508 of the CFTR gene. Now, the complications of cystic fibrosis. We’ve already mentioned the lungs. 01:32 Most patients will develop bronchiectasis, most patients will develop respiratory failure due to airways obstruction. In addition, they can get lobar collapse due to thick sputum plugs in the bronchi, they get pneumothorax, major hemoptysis, can have super infections, allergic broncopulmonary aspergillosis, non-tuberculosis mycobacteria infections. But because of this problem with the CFTR affects all the body, there are other organs that get affected as well. And the most important of these are the pancreas, where obstruction of the pancreatic ducks eventually leads to pancreatic damage and the patient will have malabsorbtion due to lack of release of the pancreatic enzymes into the gut, and many patients will develop significant diabetes or at least glucose intolerance. In addition, the men will be infertile because of the lack of production of sperm. And the upper airways are frequently affected in patients with cystic fibrosis. There are occasionally other complications that occur. Biliary obstruction and liver cirrhosis occur in a minority of patients. Gallstones are not that common, and small bowel obstruction is one of the relatively common serious complications of cystic fibrosis. How to make the diagnosis? It’s the sweat test that will indicate whether somebody has cystic fibrosis. It has a raised chloride concentration. There are other methods of testing, nasal potential differences for example, and eventually we actually do genetic testing on patients suspected of cystic fibrosis. 03:04 In fact, in the UK and other Western World countries cystic fibrosis is screened for at birth nowadays. Treatment is similar to that of bronchiectasis but more intense. Daily physiotherapy, Frequent antibiotic for exacerbations. Those often need to be intravenous because the patient is colonized with Pseudomonas. 03:23 Prophylactic antibiotics to stop those exacerbations and therefore to slow down the progression of respiratory failure. Nebulized hypertonic saline. Nebulized DNA. These are non-antibiotic mechanisms that try to reduce the phlegm production and keep the patient free of exacerbations. 03:39 Bronchodilators of the airways obstruction. But in addition they need other treatment. 03:43 They need pancreatic enzyme replacement therapy, Insulin for the diabetics, Dietary support. 03:51 And really the only life-saving treatment that can be used is lung transplantation. 03:55 So that is the treatment that will cure the patient in the minority that manage to get to that point. So I've just listed here for interest the standard therapy for somebody who has cystic fibrosis, an adult with significant disease. And as you can see, it's a very considerable treatment load. The patient needs to take daily antibiotics azithromycin, they'll have daily nebulized tobramycin, nebulized salbutamol, nebulized DNAs. Each of those takes a few minutes to take, so that's a considerable portion of the day is taken up by doing nebulized therapy. Perhaps they have to do physiotherapy twice a day, again, that takes a lot of their day up. They will require Creon capsules to help with the digestion of their food due to their pancreatic insufficiency, they may require insulin injections and overnight PEG feeding is very common in patients to try and supplement their feed and keep their BMI above a 19 or 20. So this is a very considerable treatment load that's required for these patients and despite this, almost all these patients will die by their 40 or 50 years of age. 05:04 Allergic bronchopulmonary aspergillosis, now this is a disease that has been mentioned in several different talks. It's an allergic response to inhaled aspergillus spores and it's a complication of asthma, cystic fibrosis and is a cause of bronchiectasis. What's actually happened is that you inhale the aspergillus spores which are ubiquitous in the atmosphere, so you cannot avoid them, and because the body has developed an allergy to those aspergillus spores, you get inflammation in response to the inhaled aspergillus spores. And that results in poorly controlled asthma, progressive airways destruction, upper lobe and central bronchiectasis and frequent lobar collapse in potentially bronchoceles as shown in this x-ray where sputum plugs are clogging off the bronchi and causing fluid retention or collapse of the lobe distorter. How do you make the diagnosis of ABPA? Well you need to think about it in somebody who has asthma, that has become poorly controlled or has been associated with a fall in their FEV1. It's also routinely tested for in patients with bronchiectasis. The diagnosis is made mainly by blood test, a high total IgE and aspergillus specific antibodies IgE or IgG, which show that there is a reaction in that person to aspergillus specific antigens, and skin tests does the same, also demonstrates that there is an aspergillus specific allergy. Treatment is pretty much the same as it is for asthma and for bronchiectasis, with inhalers, antibacterials for excessive exacerbations, but they often need a high dose of inhaled steroids and frequently they need oral prednisolone, and occasionally we use antifungals as they are beneficial in patients, especially those that need high doses of oral prednisolone to control their disease.
About the Lecture
The lecture Cystic Fibrosis and ABPA by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Airway Diseases.
Included Quiz Questions
Which of the following is NOT associated with cystic fibrosis?
- Lung cancer
- Pancreatic insufficiency
- Sinusitis
- Small bowel obstruction
Which of the following statements best describes the pathogenesis of infection in patients with cystic fibrosis?
- Thickened, difficult to clear, gastrointestinal and airway secretions
- Impaired acquired immunity
- Defective phagocytosis
- Primary defect in ciliary movement with increased risk of infection
- Loss of protection against proteases such as neutrophil elastase
Which of the following is NOT appropriate in the general management of cystic fibrosis?
- Exercise avoidance
- Inhaled DNAase
- Inhaled hypertonic saline
- Antibiotic
- Bronchodilator
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |