Playlist
Show Playlist
Hide Playlist
COVID-19: Vaccines
-
Slides Coronavirus Vaccines.pdf
-
Download Lecture Overview
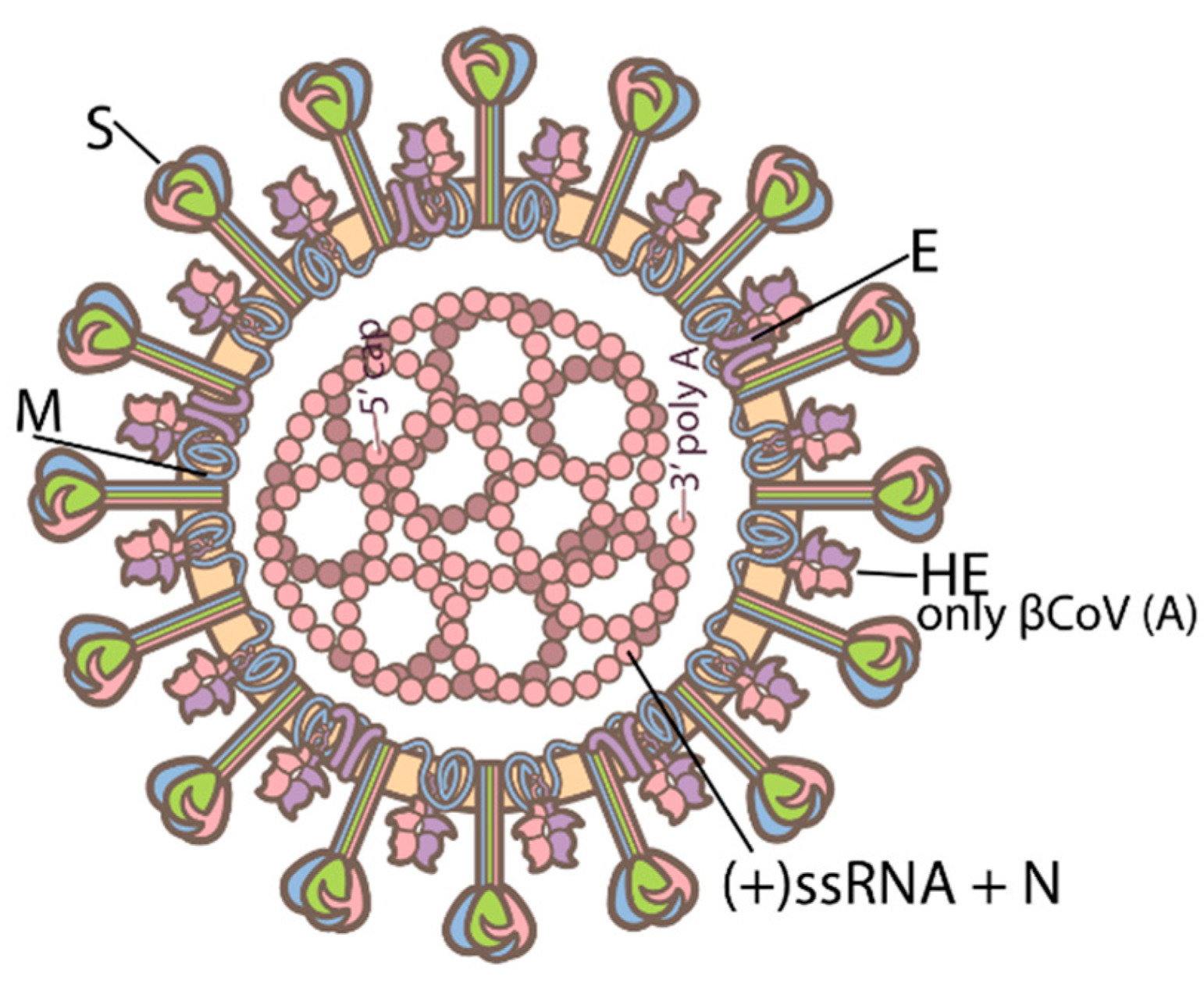
00:08 COVID-19 Vaccines. 00:10 Vaccines in general, are the best tool for prevention against any infectious disease. 00:15 And for them to be effective and to be accepted, as being effective and again this is any infection, it should be at least 50% effective. 00:24 Specific to COVID-19 and the SARS-Coronavirus II vaccines, the initial requirements in the United States, were that the new vaccine products, be at least 50 % effective. 00:36 Now, as we are moving forward into the current, there are many vaccine products, The CDC recommends everyone aged six months and older get vaccinated for COVID. 00:48 So, vaccines are always the best tool for prevention as noted and luckily, the COVID-19 pandemic, has triggered creation of very successful vaccines, even when compared to the influenza vaccine, which is perhaps one of the most common and upheld successful interventions. 01:07 The influenza vaccine, typically 40% to 60% effective in any epidemic year, but, it is still quite useful in preventing severe disease and preventing an overburdening of the healthcare system. 01:20 Full vaccines then, are recommended for everybody, including those who have had prior COVID-19, since it has been demonstrated that patients with mild to even moderate COVID-19, have a risk of second infections or even third infections and vaccines provide a robust, high level of antibody protection against currently the spike protein, which is, quite protective even for those who have had prior infection. 01:48 What are the types of vaccine methodologies? And we start with the products by AstraZeneca and Johnson and Johnson, similarly, Russia’s products Sputnik V, follows this methodology as well, these are vaccines which include a non-replicating adenovirus as the vector or the carrier for a gene encoding the spike protein of SARS-Coronavirus II. 02:14 The next category are the vaccines made by Pfizer and Moderna. 02:19 These are messenger RNA vaccines in which, the messenger RNA, specifically and only for the S-protein gene, are included in a nanoparticle encapsulated lipid particle construct, which then, triggers immune reaction. 02:36 And then a vaccine produced by Novavax, takes the actual spike protein itself the S1-protein, coats it with synthetic nanoparticles and then provides it in an immune boosting adjuvant, which triggers immune reaction. 02:52 So, in general, how do vaccines work? Well, we know that vaccines work by triggering, a specific adaptive immune response, by the human immune system, which then, creates memory, so, that the individual's immune system, can react to subsequent challenge, by that same antigenic challenge. 03:11 Looking specifically at the messenger RNA based vaccines and this this is newer technology to most of us, it is really quite unique and exciting as a platform for vaccines, because this process will work for other infectious diseases as well. 03:28 In a messenger RNA based vaccine against SARS-Coronavirus II, the messenger RNA code for the spike protein the S1-protein gene, is introduced into the human body, where, it is taken up or absorbed by antigen presenting cells, as with any other antigen delivery via vaccine. 03:53 However, those antigen presenting cells, as they ingest the messenger RNA, then go through translation and transcription processes, to create the spike protein and then express the spike protein, at their cell surface along with MAC classes 1 and 2 and or, release the spike protein where it is then able to be ingested and to trigger an immune response, by other antigen presenting cells. 04:20 So, here, we see the delivery vehicle, the messenger RNA vaccine, with the messenger RNA code, for the spike protein in its little nanoparticles, it then is taken up as the full construct by the anti-presenting cell, the messenger RNA is introduced into the anti-presenting cell, where, it is translated into spike protein, the spike protein then is expressed at the cell surface, with MHC class 1 and 2 to T-lymphocytes and B-lymphocytes, which, are the next stage and or secreted externally to where it is then taken up by other antidepressant cells in the same process and that then drives the adaptive immune response using T-lymphocytes the CD4+ T-helper T-lymphocytes and B-lymphocytes to create specific immunoglobulins. 05:15 So, that is the strategy, does it work? Now, this this is a historic slide, but it shows in the United States, the surge or peak, which occurred in the winter of 2021, in the States and you can see on the slider front of you, around, I guess it was December, is when,w max vaccinations started in the United States and it took quite some time of course, to get to anything resembling a decent vaccine coverage as that vaccine coverage has rolled out, one can see a decrease in the number of cases quite robustly, as we go into spring of 2021.
About the Lecture
The lecture COVID-19: Vaccines by Sean Elliott, MD is from the course Coronavirus.
Included Quiz Questions
What is the minimum level of efficacy required for FDA approval of a vaccine in the US?
- 50%
- 35%
- 65%
- 80%
- 95%
What is the level of efficacy of the Pfizer BioNTech (an mRNA vaccine) in individuals ages 5 to 11?
- 91%
- 50%
- 65%
- 80%
- 90%
How does an mRNA vaccine work to produce immunity?
- A nanoparticle-encapsulated lipid that includes mRNA specifically for the SARS-CoV-2 spike protein gene is injected into the host to produce an immune response.
- Inactive viral mRNA triggers an immune response so that T and B cells are already activated in case of exposure to a new virus.
- The mRNA of a non-replicating adenovirus is injected into the vaccine recipient.
- Viral mRNA from the SARS-CoV-2 virus is injected, causing an immune memory response to recognize and fight off future infection.
- A synthetic nanoparticle already coated with the spike protein is injected into the host to produce an immune response to future SARS-CoV-2 mRNA, if exposed.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |