Playlist
Show Playlist
Hide Playlist
Colonic Polyps: Types and Polyposis Syndromes
-
Slides GIP Colonic Polyps.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
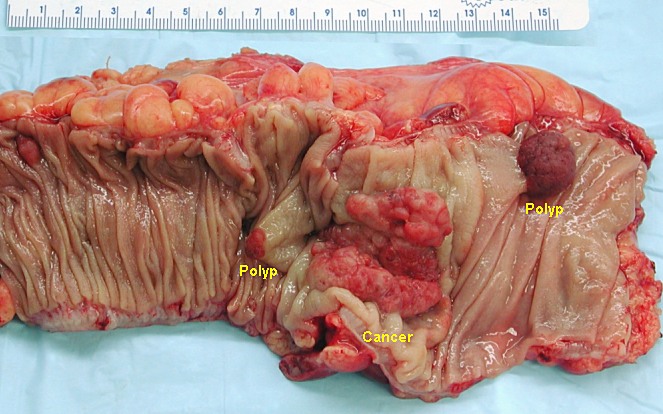
00:01 Welcome. In this talk, we're going to cover a rather broad set of topics related to colon polyps. 00:08 So, colon polyps are benign and premalignant epithelial or they can be inflammatory proliferations. 00:15 Let's look briefly at the epidemiology. So, colon polyps are found in a significant proportion of adults. 00:24 So, anyone over the age of 30 to 40. 00:26 Adenomatous polyps which are going to be of the premalignant variety are the most common types, so, about 70% of the time, if it's a polyp, it's an adenomatous polyp. 00:37 Most of the neoplastic or premalignant colon polyps are adenomas, okay? So, proximally, two-thirds overall. 00:45 And most colorectal cancers are felt to arise from sporadic adenomatous polyps. 00:51 So, that provides kind of a framework and a basis for thinking about these. 00:55 The risk factors for polyps across the entire spectrum. So, diets that are high in red meat and fat and have less fiber. 01:03 Inflammatory bowel disease, Crohn's disease, and ulcerative colitis. 01:08 If there's a family history of either colorectal cancer or adenomas, tobacco and alcohol use, obesity, and poorly controlled type two diabetes. 01:19 When we think about colon polyps, we're going to classify them into benign categories and neoplastic or premalignant categories. 01:27 In the benign categories are hyperplastic, hamartomatous, and inflammatory, and we'll cover each of those very quickly in short order. 01:36 The neoplastic adenomas, premalignant tumors are subdivided into tubular, villous, tubular villous and sessile serrated. 01:46 These are their appearance either a combination of the way they look grossly and/or microscopically. 01:52 It's not too important for you to be able as a medical student, to be able to identify which is which when you become a gastroenterologist or when you become a GI pathologist, then, we'll expect you to do that. 02:06 For now, it's enough to recognize that something is a benign lesion and something is an adenomatous or preneoplastic premalignant lesion. 02:18 So, for benign polyps, hyperplastic polyps are really just a benign epithelial proliferation. 02:24 About 35% of all polyps are going to be in this category and it's just more proliferation or less epithelial cells dying off as part of their normal lifecycle. These are completely benign. 02:37 There are no mutations in them and they are a very common feature seen across the spectrum. 02:47 Hamartomatous polyps may be sporadic or hereditary and there are five kind of hereditary polyposis syndromes that have been associated with them. 02:57 Hamartomas just mean accumulations of normal structures that should be present in that location but with an expansion of a particular subset. So, there may be more mesenchymal elements. 03:10 There may be more vascular elements. There may be more epithelial elements. 03:14 There may be more smooth muscle elements but those represent the hamartomas. 03:20 For the syndromes that we have here, Cowden syndrome are hamartomas that involve the skin, the mouth, and the GI tract. They're associated with a PTEN, that's a phosphatase and tensin homolog mutation PTEN is a tumor suppressor gene. 03:38 So, this influences cellular proliferation. Cronkhite-Canada syndrome is a polyposis syndrome associated with abnormal skin pigmentation and alopecia or hair loss. It's not hereditary. 03:51 We don't know what causes it. Tuberous sclerosis involves hamartomas that are seen in the brain, or the kidney, the heart, and the skin, as well as the GI tract and they're associated with various mutations and tumor suppressor genes, hamartin, tuberin, or mutations in the mTOR pathway. 04:11 mTOR stands for the Mammalian target of rapamycin pathway. 04:14 All these are involved in cellular proliferation and turnover. 04:17 Juvenile polyposis is a sporadic, sometimes, autosomal dominant mutation and it's mutations in genes that control, again, proliferation down the SMAD4 and transforming growth factor beta pathway. 04:32 And then, finally, Peutz-Jegher Sydnrome is a syndrome associated with pigmented lesions, typically, of the oral pharynx and lips and also, GI polyps. 04:42 It's an autosomal dominant disease due to mutations in the STK11 gene which is also involved in cellular proliferation. 04:51 Do you need to memorize all of these syndromes? No, until you become a GI pathologist or a gastroenterologist. 05:01 Do you need to know that they are there? Yes, and that these are associated usually with baseline genetic mutations and genes that influence proliferation. 05:12 Finally, inflammatory polyps and this is just due to cycles of inflammation and injury and this may be infectious or it may be associated with things like inflammatory bowel disease. 05:23 And that we're just accumulating increased numbers of lymphocytes or other inflammatory cells of the innate immune system such as macrophages below the epithelium. 05:33 It's not even really an epithelial proliferation at all but an accumulation of inflammatory cells. 05:39 So, these are our benign polyps. Let's get to the premalignant or neoplastic polyps. 05:45 And these are for the most part, going to be adenomatous polyps. 05:48 They can be low, middle, and high grade in terms of their degree of dysplasia or abnormality. 05:56 And as we've already talked about, they have a propensity to transform overtime into high grade dysplasia or frank carcinoma and eventually, can progress to colon cancer. 06:08 As you've already seen, they are precursors to the majority of colon cancers and they usually follow the same sword of genetic changes that we've seen previously when we talked about colorectal cancers. 06:21 So, I will refer you to that talk in the series of Lecturio lectures on colorectal cancer. 06:27 Again, adenomatous polyps can be tubular which constitutes the majority of such polyps or they can become villous which is a very small percentage. 06:38 Or they can be tubulovillous, somewhere in between, and you can see the risk of malignancy written there. 06:43 Again, do not necessarily need to memorize those details but be aware that based on the appearance that we can evaluate grossly and microscopically, we can assess relative risk. 06:57 So, the risk of developing colorectal cancer from an adenomatous polyp is based predominantly on size. 07:05 That's your most important factor. 07:07 So, if the adenoma is less than one centimeter in diameter, there's a very rare infrequent risk of malignancy. 07:17 However, when these adenomas get to be greater than four centimeters, then, the risk of having a focus of invasive cancer within it goes up dramatically. 07:27 And then, if these adenomas have higher grade dysplasia or have villous architecture, what we talked about on the previous slide, those also increase the risk of malignant transformation. 07:40 Amongst the various categories, we talked about villous and tubulovillous and tubulous, you know, tubular adenomas. 07:47 Sessile serrated adenomas are a subset of the overall group. They tend to be flat, so, hence, sessile. 07:56 They tend to have kind of an irregular serrated surface grossly kind of looking like a stegosaurus and they represent 15% of sporadic CRCs. 08:08 So, they have a relatively higher frequency of developing into malignancy. 08:12 They don't have the features, cytologic features of dysplasia, so, as a pathologist, you say, "That doesn't look too bad." But they do have a similar malignant potential as in adenomas of the tubulovillous category, etc. that have a higher grade dysplasia. 08:29 In the same way we had benign polyposis syndromes, there are neoplastic polyposis syndromes. 08:37 So, hereditary polyposis with neoplastic polyps include Lynch syndrome which are mutations in mismatch repair genes. 08:47 Familial adenomatous polyposis or FAP and their variants with a mutation in the APC gene, the adenomatous polyposis coli gene. And each of these syndromes, although it's relatively rare, they account for a disproportionate number of colorectal cancers. 09:04 So, let's take a moment to discuss them because they are more important in terms of driving malignancy. 09:12 So, HNPCC, your hereditary nonpolyposis colorectal cancer or more easy to say, Lynch syndrome, is the most common inherited cause of colorectal cancer, 2% to 4% of them is an autosomal dominant inheritance. It's about 1 in 300 people, so, it is a significant percentage of the population that will have this mutation. 09:36 These are mutations in DNA mismatch repair. So, if we have a double stranded break and/or we have a mismatch in terms of which nucleotide is matched with another, that's usually repaired quite efficiently and in Lynch syndrome, there are a number of mutations that lead to aberrant repair, so, an accumulation of mutations. 10:01 They will have a very high number of neoplastic polyps and the longer that they're there, the greater number of neoplastic polyps, the higher the rate of progression to colorectal cancer. 10:11 These patients are not affected just in their GI tract or in their colon. 10:16 If you have this, you also have an increased risk of endometrial and ovarian cancers and overall, there's a 60% lifetime risk of developing colon cancer if you have Lynch syndrome. 10:29 For the familial adenomatous polyposis syndrome and their variants, so, these are sporadic. 10:33 They can also be autosomal dominant inherited mutations. 10:38 The APC gene product is involved in targeting the degradation of beta-catena, a membrane associated protein that if it is released from the plasma membrane can translocate into the nucleus and cause cellular proliferation. 10:55 If you don't degrade it appropriately, the cells will proliferate more aggressively. 11:00 So, classic FAP is about one in 7000 people, so, it's less frequency than Lynch syndrome and in the classic FAP, we'll see colons that are completely littered, studded with polyps, over hundreds of polyps. 11:16 There are mild or attenuated versions of this of FAP with something less than 100 in the total colon but overall, an either one, classic or attenuated, there's essentially a 100% lifetime risk of developing colon cancer. 11:32 So, these patients need to be identified and they need to have a colectomy before they develop colon cancer.
About the Lecture
The lecture Colonic Polyps: Types and Polyposis Syndromes by Richard Mitchell, MD, PhD is from the course Small and Large Intestines Disorders.
Included Quiz Questions
What is the most common type of colonic polyp?
- Adenomatous
- Hyperplastic
- Sessile
- Inflammatory
- Villous
Which is NOT a risk factor associated with colonic polyps?
- Asbestos
- Inflammatory bowel disease
- Obesity
- High-fat diet
- Tobacco
Which types of colonic polyps are associated with neoplasms? Select all that apply.
- Tubular adenoma
- Villous adenoma
- Hyperplastic
- Hamartomatous
- Inflammatory
What genetic mutation is associated with Lynch syndrome?
- Mismatch repair genes
- p53
- Rb
- Tumor suppressor genes
- BRCA1
What genetic mutation is associated with familial adenomatous polyposis?
- APC
- BRCA1
- Mismatch repair genes
- Rb
- p53
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |