Playlist
Show Playlist
Hide Playlist
Chronic Bronchitis: Multistep Approach
-
Slides ObstructiveLungDisease ChronicBronchitis RespiratoryPathology.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
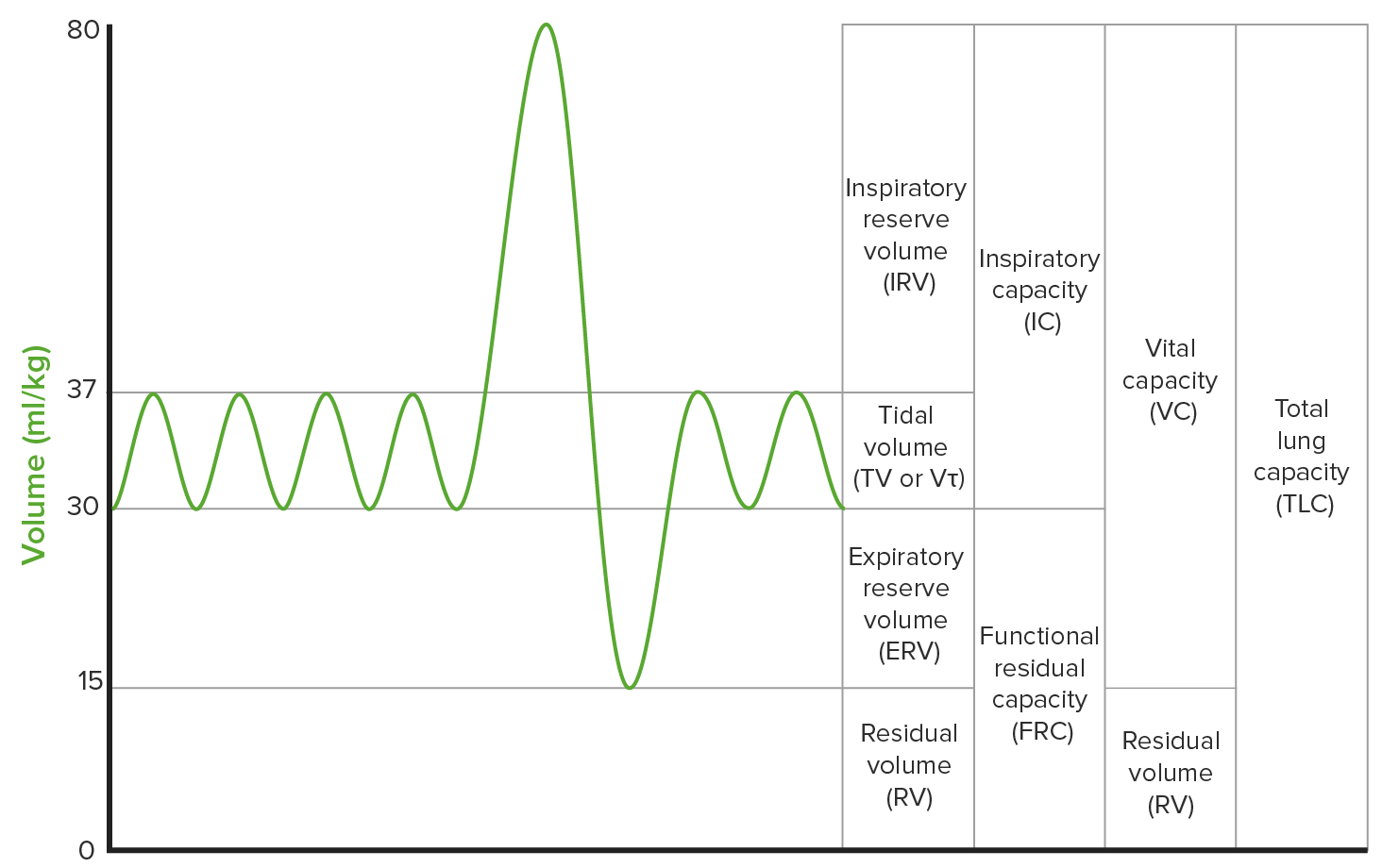
00:00 Good. Inspiration. That has been compromised. Then finally, what we talked about extrathoracic, well, intrathoracic, meaning to say an obstruction and therefore you have problems with your expiration-exhalation loop. 00:10 Now, let’s take a look at smoking. So that was review, make sure you’re clear about that. Let’s take a look at smoking. It’s never too late to stop smoking is the point of this graph. Never. On your Y-axis represents your FEV1 and that’s your percentage of air as you know that you are exhaling in one second. Now, on the X-axis represents your age. 00:33 Let’s go to worst case scenario. Let’s go to worst case scenario where we have death at the bottom line. That’s pretty final, isn’t it? Death. So, with the death occurring, I want you to now come to, please, the earliest age that we see here. The earliest age, the dark green solid line, in which your patient has died before the age of 75. That is a patient who is continuously and regularly smoking and therefore, susceptible to all kinds of issues including chronic bronchitis, including your emphysema. If the patient had asthma, then it could be all kinds of mixtures. Or, my goodness gracious, what about those lung cancers? Any of them. But, more likely, squamous or small. You’ll notice there that the average age is below 75 with the patient continuously susceptible to damage due to smoking. It’s never too late. 01:35 Your patient now, now let’s move over one to the right where it says “Stopped at 65”. Even stopping at 65, the patient might have potentially gained 5-10 years of life. It’s never too late to stop smoking. 01:51 Let’s go further proximal, shall we? I want you to take a look at the title where it says “Stopped at 45”. You stopped at 45, you have then prolonged your life so much more. It’s never too late to stop smoking. 02:06 If the patient has never smoked, obviously, natural. 02:10 Take a look at disabilities. Disability will always take a little bit, will take place a little bit younger in your patient who’s smoking and death will always take place a little bit younger in your patient. I hope that’s clear, your point to your patient. 02:24 You’re a clinician, you’re doctor, I don’t have to tell you anything. At least do this for me and do this for the field of medicine, tell your patients “It’s never too late to stop smoking”. 02:38 Let’s take a look at multistep approach in pulmonary function test, a diagnostic test of choice. Reveals your classic obstructive pattern. What’s that mean to you? A decreased FEV1 to FVC ratio. Tell me about your total lung capacity. It is increased and residual volume as well. Tell me about your DLCO, especially, let’s say, for example, if it’s emphysema. 03:02 You can then expect that you’ve lost your surface area and therefore, your DLCO in fact is decreased. What does that mean, DLCO? Good. Your oxygen from the alveoli to your pulmonary capillary is not moving quick enough. Why in this case with emphysema? Loss of surface area, good. 03:23 Now, preventive medicine. How big is this? Huge. These individuals might be susceptible, all COPD patients are susceptible to? Pneumonia. Vaccine is a very good idea. Yearly influenza vaccine is a good idea. Ultimately, tobacco cessation. You do this, you slowly progress the disease process, that’s amazing. 03:47 Now, home oxygen therapy to correct hypoxemia, if PaO2 is less than 59 or saturation is less than 89. Are we clear? Remember, PaO2 on the arterial side normally should be, how many times have we talked about this? 95-100. If it drops below 60, not good. Home oxygen. 04:07 You're worried about your saturation of oxygen clinically even if it drops below 90%. Keep that in mind. 04:15 Management, treatment of acute flares. Steroids, oxygen, antibiotics, especially for Strep. pneumo and the big one here, Hemophilus influenza may require non-invasive ventilatory support. Which one would be a better choice? BiPAP, CPAP, intubation or synchronised intermittent mandatory ventilation? All the discussions that we had before. First, you want to try to remain non-invasive. Therefore now you’re left with two answer choices. 04:52 Either have CPAP or BiPAP. Which one’s better, if your patient has hypercapnia? Good. BiPAP. 05:00 Why? Bi-level. What’s Bi-level mean to you? Inspiration, positive airway pressure. 05:07 It’s also going to help you with, Bi-level, exhalation. What’s my problem in a patient that might have acute flare? Retention of your carbon dioxide. Wouldn’t you like to facilitate some of that carbon dioxide efflux? Sure, welcome to BiPAP. Bi-level, representing both of the breathing patterns. Much more comfortable for the patient, much more effective, and as far as costs, becoming much more reasonable.
About the Lecture
The lecture Chronic Bronchitis: Multistep Approach by Carlo Raj, MD is from the course Obstructive Lung Disease: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following is NOT part of the definition of chronic obstructive asthma?
- Has 3 months of productive cough consecutively for 2 years
- Childhood asthma
- Heavy smoking for years
- Showing signs and symptoms of COPD
- Usually occurs in the 2nd or 3rd decade of life
Which of the following is NOT a measure of prevention for a patient with chronic bronchitis?
- Systemic steroids
- Tobacco cessation
- Home oxygen
- Influenza vaccine
- Pneumoccocal vaccine
Which of the following are the cut-off values for starting home oxygen therapy in COPD?
- PaO2 of less than or equal to 55mm Hg or oxygen saturation less or equal to 88%
- PaO2 < 69mm Hg or oxygen saturation < 89%
- PaO2 < 59mm Hg or oxygen saturation < 99 %
- PaO2 < 79mm Hg or oxygen saturation < 89%
- PaO2 < 59mm Hg or oxygen saturation < 95%
Which of the following is not part of the treatment for acute flares of chronic bronchitis?
- Pneumococal vaccine
- Systemic steroids
- Oxygen therapy
- Antibiotic
- BiPaP
A 30-year-old male presents with a history of dyspnea and chronic cough. He claims to have been smoking 4 packs a day for 10 years. He mentions allergies during childhood. Which of the following is the most likely diagnosis?
- Chronic obstructive asthma
- Asthma
- Chronic bronchitis
- Chronic obstructive pulmonary disease
- Atopic asthma
A patient's loop spirometry results reveal a fixed loop obstruction pattern. Bronchodilators do not alleviate the breathing difficulty. Which of the following is the probable cause of this presentation?
- Late stages of central airway obstruction
- Early stages of central airway obstruction
- Chronic bronchitis
- Chronic obstructive asthma
- Atelectasis
Which of the following loop spirometry is correctly matched?
- Fixed obstruction - both expiration and inspiration loops are shortened Variable extrathoracic obstruction - Inspiratory loop is compromised Variable intrathoracic obstruction - Expiratory loop is compromised
- Fixed obstruction - only inspiration loop is shortened Variable extrathoracic obstruction - Inspiratory loop is compromised Variable intrathoracic obstruction - Expiratory loop is compromised
- Fixed obstruction - expiratory loop only is shortened Variable extrathoracic obstruction - Inspiratory loop is compromised Variable intrathoracic obstruction - Expiratory loop is compromised
- Fixed obstruction - both expiration and inspiration loops are shortened Variable extrathoracic obstruction - Expiratory loop is compromised Variable intrathoracic obstruction - Inspiratory loop is compromised
- Fixed obstruction - both expiration and inspiration loops are shortened Variable extrathoracic obstruction - Inspiratory loop is compromised Variable intrathoracic obstruction - Inspiratory loop is compromised
Which of the following is the diagnostic test of choice in a patient with chronic bronchitis?
- Pulmonary function tests
- Chest CT
- Chest X-ray
- Bronchoscopy
- Peak expiratory flow meter
What is the advantage of using Bi-PAP to provide non-invasive ventilatory support for patients with chronic bronchitis and hypercapnia?
- Bi-PAP helps in CO2 efflux and also maintain positive airway pressure
- Bi-PAP is more affordable
- Bi-PAP is more available in the market than CPAP
- Bi-PAP has less complications associated with it.
- Bi-PAP was invented prior to CPAP
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |