Playlist
Show Playlist
Hide Playlist
Chest Wall and Muscle Disease
-
Slides 10 RespiratoryDisorders RespiratoryAdvanced.pdf
-
Download Lecture Overview
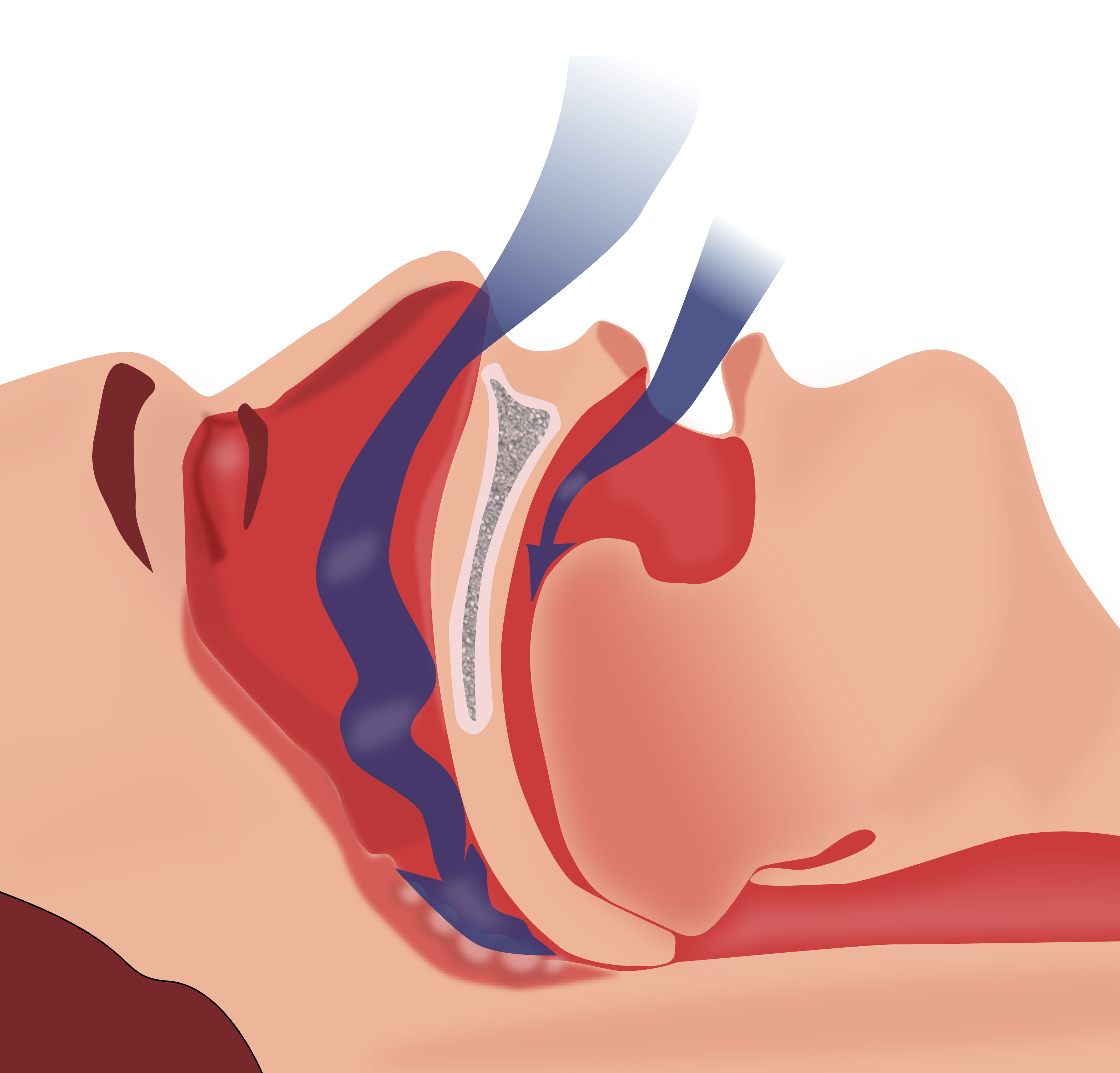
00:01 Just moving on, chest wall and muscle diseases, now we've discussed these briefly already, these are a mixed bag of diseases where you underventilate the lungs because the mechanical, the muscle or the nerve input to ventilation has been impaired, so acutely this might happen if somebody has had a road traffic accident, they get a flail chest that's where three or more ribs are broken in two or more places and that means that you don't get movement of that portion of the chest during respiration and that hyperventilates. Guillain-Barre syndrome is an acute polyneuropathy, which can ascend to affect the nerves that control the respiration, and these patients need to have their FEV1 monitored, because if it falls then they're likely to develop respiratory failure. And again a high cervical cord lesion during a road traffic accident or something like that would cause diaphragmatic weakness. The chronic causes muscular dystrophies, motor neuron disease, severe kyphoscoliosis, and obesity as we've discussed already and again the high cervical cord lesion would persistently cause underventilation of the lungs. And these patients present similarly to the presentation of anybody with chronic type II respiratory failure, morning headaches due to the high CO2, general deterioration in their overall condition, feeling tired and sleepy. Their spirometry is very important because with these disorders you cannot develop type II respiratory failure unless you have significant restrictive lung function. 01:41 The oxygen saturations may be a little low but the important test is blood gases because that will identify whether there is type II respiratory failure present or not. 01:49 The treatment is long-term ventilation, if you give patients long-term noninvasive ventilation overnight, then if you have a nonprogressive cause, such as kyphoscoliosis, then their prognosis is very good. Unfortunately, with progressive causes, it is only a temporary treatment, so patients with motor neuron disease for example, they will usually die because of type II respiratory failure despite noninvasive ventilation as the disease progresses. 02:15 Two various types of underventilation of the lung is obstructive sleep apnea and obesity hyperventilation syndrome. Obstructive sleep apnea is a very common condition, mainly affecting men in which the pharynx is recurrently obstructed at nights during sleep leading to recurrent dips in the arterial oxygen concentration. And this is diagnosed using a sleep study and treatment is essentially weight loss, and if necessary, you can use CPAP therapy overnight, which for the patients with more severe disease and that can be very effective. Obesity hypoventilation is related to central underventilation and that is caused by obesity, it tends to be in women rather than men, although it’s both sexes and that's an increasingly common cause of acute and chronic type II respiratory failure which can often be very difficult to treat because the underlying problem, obesity is not quick to be resolved. Thank you for listening
About the Lecture
The lecture Chest Wall and Muscle Disease by Jeremy Brown, PhD, MRCP(UK), MBBS is from the course Other Respiratory Disorders.
Included Quiz Questions
Which of the following is NOT true for both obesity hypoventilation syndrome and obstructive sleep apnea?
- More common in men
- Associated with obesity
- May cause type 2 respiratory failure
- Worsened physiological disturbance at night
Which of the following is an appropriate test to identify a patient with chest wall abnormalities going into type 2 respiratory failure?
- Blood gas analysis
- Spirometry
- Chest X-ray
- CT scan
- Peak expiratory flow
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I found the lesson very clear and useful! Thamkyou Professor Brown!!