Playlist
Show Playlist
Hide Playlist
Cell Surface Receptors
-
Slides Introduction EndocrinePathology.pdf
-
Download Lecture Overview
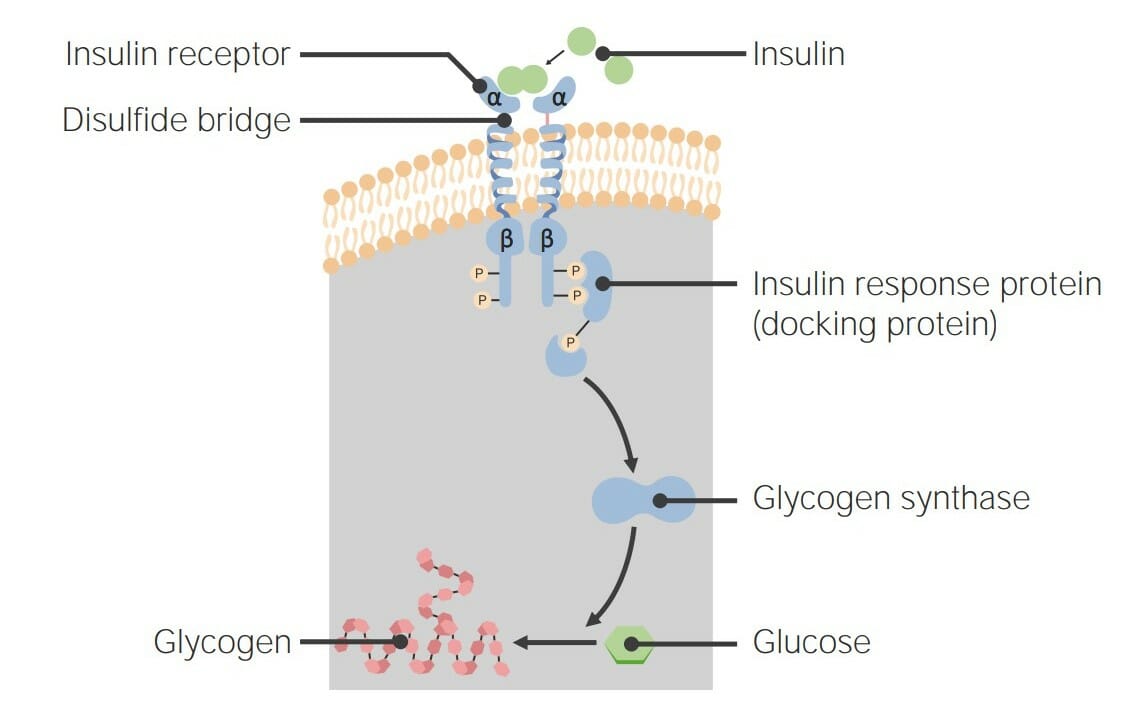
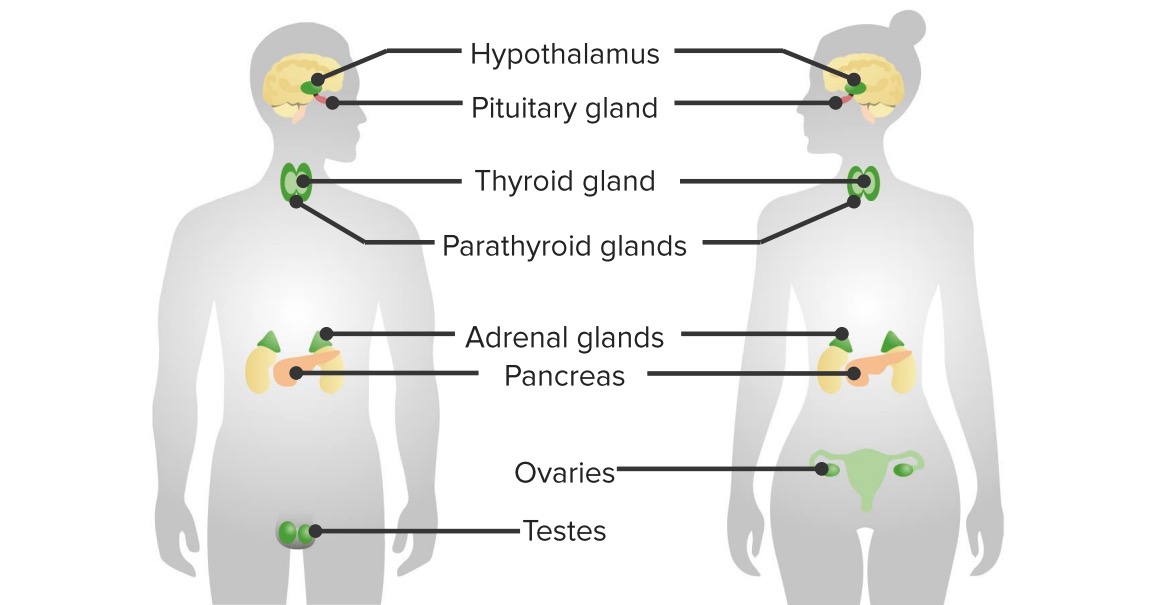
00:02 On this slide, we’ll take a look at the table that is dealing with receptors on that membrane and how the hormone, when bound to the receptor, is then going to bring about signaling to your cell, to bring about an appropriate response. 00:17 For example, take a look at tyrosine kinase here. 00:20 Now, tyrosine kinase has a global picture. 00:22 And by that, I mean tyrosine kinase, as we have seen, plays an important role in neoplasia. 00:29 We talked about tyrosine with receptor tyrosine kinase. 00:32 We talked about it with chronic myelogenous leukemia, 9 and 22. 00:36 Does that ring a bell? It should. 00:39 All that was tyrosine kinase. 00:41 Do not forget about those topics. 00:44 Now, under endocrinology, with tyrosine kinase, it's a fact that you have insulin being released. 00:50 When is insulin being released? It's being released when – well, let me ask you? Is it during the fed or fasting state? You're sitting there, listening to me, you're having a snack. 01:03 You're being fed. 01:04 How is it and what are you being fed with or maybe a granola bar? Some type of carbohydrate, a snack of some sort. 01:11 That glucose, that carbohydrate – that glucose is then going to work directly upon your beta (inaudible 1:16) in your pancreas, right? And when we talk about the pancreas, we will divide it into endocrine and exocrine. 01:24 Obviously, here, we will be dealing with endocrine pancreas. 01:28 This insulin will be released from the beta (inaudible 1:30) cell. 01:31 We'll talk about that in greater detail. 01:33 And that insulin is then going to work upon its target organs. 01:37 Those target organs include things like, well, maybe your skeletal muscle. 01:41 Your skeletal muscle is then going to do what? It's going to take up the glucose. 01:45 And my point is, during your fed state is when the insulin is being released. 01:49 That insulin is then going to up-regulate your glucose transporters. 01:53 Remember this from biochemistry. 01:55 And let's say that this is an insulin-dependent type of glucose transporter. 02:00 Obviously, our topic now brings us to glucose transporter. 02:03 2 or 4? 4, isn’t it? If you're not good with this, make sure you go back and review your biochem for glucose transporters. 02:13 Once insulin then works through tyrosine kinase, it is going to up-regulate your glucose transporter 4s, thus bringing in your glucose, aren't you? Welcome to insulin and tyrosine kinase. 02:26 There are growth factors as a umbrella of hormones that work through tyrosine kinase. 02:33 Let’s talk about a few important ones. 02:36 Here’s insulin growth factor 1. 02:38 Insulin growth factor 1, when would you ever use this clinically? To measure activity of which hormone? Good. 02:47 Growth hormone. 02:49 Where is IGF-1 coming from? It comes from the liver. 02:53 Remember that growth hormone and if you don't, that's okay. 02:55 We'll talk about this in greater detail. 02:58 Growth hormone coming from anterior pituitary – let me keep pushing you. 03:02 That growth hormone was being released by growth hormone releasing hormone. 03:06 That growth hormone has a very, very – well, in comparison to IGF-1, has a shorter half-life. 03:13 Hence, clinically, you're not going to measure growth hormone. 03:17 Is that clear? Especially because also the manner in which it's being released from the anterior pituitary is pulsatile. 03:27 Keep that in mind. 03:28 What do you mean? For example, baby goes to sleep at night or a child goes to sleep at night. 03:37 When we go to sleep at night, let’s say it's a child, it requires quite a bit of growth. 03:42 It is during this time at night when a child goes to sleep, in which the child is going to release growth hormone from the anterior pituitary. 03:52 So, what happens during the day? Well, during the day, there might not be as much growth hormone. 03:58 My point is this, because of the pulsatile, maybe a little bit more at night, during sleep, or less during the day, the pulsatile nature of growth hormone makes it a very unpredictable type of measurement of what you might want to do if you're thinking about a patient with growth hormone pathology, right? IGF-1 becomes reliable. 04:27 IGF-1 has a longer half-life. 04:30 Growth hormone works upon the liver to release IGF-I, hence it's important that you pay attention to the effective IGF-I clinically. 04:39 And you have other growth factors here, including platelet-derived growth factor (PDGF). 04:46 Or fibroblast growth factor. 04:48 These are important growth factors during the repair process, as the name implies. 04:53 These growth factors, also we’ve talked about this earlier in neoplasia, will be important markers for you to measure. 05:00 For example, if your patient has a glioma, maybe an astrocytoma, a CNS tumor. 05:07 Then, you’d be using platelet-derived growth factors. 05:09 Do you understand the significance? Do not just sit here and memorize these columns. 05:13 I'm giving you important connections, so that when you’re posed with the question on your boards, you know as to what you're referring to. 05:22 Fibroblast growth factor. 05:24 Fibroblast growth factor, when would you ever want to bring this into play? Good. During the repair process. 05:31 Say, that you have a wound and you have a secondary wound. 05:35 Mean to say that you have a knife wound, in which the edges is far apart – the edges of the wound are far part, don't you think that you might want to lay down a little bit more collagen? Sure, you do. 05:49 And so, therefore, what growth factor might you want to bring in? Fibroblast growth factor. 05:53 Working through whom? Tyrosine kinase. 05:57 Let’s continue. 05:58 This is Gs. 06:01 This brings me back to biochemistry. 06:03 What were the G proteins? Gs, Gi, Gq. 06:06 This is Gs. 06:06 What does that mean to you? AAAAA, what does that mean? That means that whenever you think about Gs, you should be thinking about the letter A. 06:14 You’re thinking about adenylyl cyclase, you’re thinking about ATP, you’re thinking about cAMP. 06:21 Let me walk you through this. 06:23 Take a look at ACTH, TSH, FSH, LH. 06:26 Stop there. 06:28 Why? All these hormones that I just mentioned and listed are all anterior pituitary hormones. 06:33 Anterior pituitary. 06:34 Stop there. 06:36 ACTH, tell me what organ that works upon. 06:38 Adrenal cortex – AC. 06:41 TSH, what hormone does that work upon? Thyroid. 06:45 FSH and LH, what organ does that work upon? Gonads. 06:50 These all work through Gs, cAMP. 06:53 Is that important? Oh, my goodness, yes! It's important that you understand when or what type of second messengers these are using. 07:03 We’ll play around with these a little bit more later. 07:05 Next. 07:07 This is V2 receptors. 07:10 Why do we call this V2? Why do we even call this a V? Because ADH is called vasopressin. 07:17 Good. 07:18 How many kidneys do we have that’s functioning normally? One, two, yeah. 07:23 Two kidneys. 07:25 Welcome to V2 receptors. 07:27 V2 receptors via ADH – before we go there, why would you want ADH? Are you in a state of drinking too much water, releasing ADH? Would that be the trigger? Or would the trigger be not drinking enough water, maybe dehydration. 07:47 Dehydration. 07:48 Good. 07:49 This is then going to stimulate what? The osmoreceptors. 07:52 Where are they located? Remember? Hypothalamus. 07:56 Tell me where ADH is being synthesized. 07:59 Good. 08:00 Hypothalamus. 08:02 Am I asking questions that are trivial? No, no, no. 08:05 I'm asking questions that are clinically significant. 08:08 All I'm doing is laying down the foundation. 08:11 Work with me here. 08:12 The ADH is being synthesized in the hypothalamus. 08:16 It is being delivered to the posterior pituitary. 08:19 You're releasing when? When you’re dehydrated. 08:22 What does that mean to you? Your plasma osmolality, you must know, will be elevated. 08:29 You’re going to go down to the collecting duct. 08:32 What do you want to do? Antidiuresis. 08:36 What do you want to do with the collecting duct in the nephron? You want to reabsorb that water. 08:40 Via V2 receptors. 08:43 Through Gs, cAMP. 08:47 That's one set of receptors. 08:49 The other set of receptors would be Vq. 08:53 Vq or Gq, think of it that way. 08:55 Your Gq will be a Vq. 08:57 In other words, your vasopressin, V1 vasopressin will work upon your blood vessels and that will work through Gq. 09:06 In other words, that will IP3 mechanism, as we shall see. 09:10 Let’s go to PTH. 09:12 Close your eyes. 09:13 Where is PTH coming from? Good. 09:16 Parathyroids. 09:17 What’s my trigger? Calcium. 09:20 What level of calcium is going to release PTH? High or low. 09:25 You got this. 09:26 Low. 09:27 Right? So, your patient for whatever reason is hypocalcemic. 09:34 That hypocalcemia is going to trigger my PTH to release your parathyroids. 09:41 Next, the parathyroids are going to work upon what organ? The kidney. 09:48 Where in the kidney are you going to reabsorb your calcium? You tell me. 09:53 Where? In the PCT or DCT? DCT. 09:59 Good. 10:00 In the DCT, you have PTH and its receptors. 10:05 Through what? Gs, cAMP. 10:10 My next question is this. 10:12 As long as you're perfectly physiological and you're releasing PTH because you want to maintain calcium, how much cAMP might you find in urine? Increased. 10:25 Do you know a pathology where your PTH receptors aren’t working? You should. 10:31 It’s called pseudohyperparathyroidism. 10:33 What? Pseudohyperparathyroidism. 10:38 So how much cAMP are you going to find in the urine of that patient? Not much. 10:43 Do you understand how important these columns are? Let’s go into glucagon. 10:47 Glucagon. 10:48 When are you going to release glucagon? Fed state or fasting state? The opposite of insulin. 10:54 Think about this as being a seesaw. 10:57 Seesaw. 10:58 What do you mean? Insulin is on one end, glucagon is on the opposite end. 11:04 Always. 11:05 Isn’t it? So, when did you release insulin? It’s all about language. 11:09 Your insulin was being released during fed state. 11:12 When did you release glucagon? Fasting state. 11:15 So, as you become hungry, the two hormones that are always going to work in conjunction would be your cortisol and glucagon. 11:25 Keep them always together. 11:26 Always. 11:28 If cortisol is not present, glucagon will never work, hence cortisol is the most important stress hormone. 11:38 I can't stress that enough. 11:40 So, cortisol, glucagon work in conjunction. 11:44 Glucagon is then going to bring about release of glucose or, should I say, gluconeogenesis. 11:52 From where? Biochemistry. 11:54 From where? Liver or skeletal muscle? Don’t you ever say skeletal muscle. 12:00 You do not ever have gluconeogenesis in your skeletal muscle. 12:04 You’ll have it in your liver. 12:06 Guaranteed. 12:08 Glucagon, cAMP, what kind of questions could they ask here? They love the biochemistry for glucagon. 12:15 Would you please tell me the name of the enzyme that’s responsible for breaking down cAMP? You've got this. 12:21 Give me the name of the enzyme that you learned in biochem that breaks down cAMP. 12:26 Is it called phosphodiesterase? Isn’t it? If you inhibit phosphodiesterase, in this particular situation, isn’t it possible that you might enhance the activity of glucagon. 12:39 I can't even tell you how important of a concept that is if you don't know that already. 12:45 Make sure you know about your biochem. 12:47 Make sure you know about signal transduction. 12:49 I'm giving you information here, so that you can attack your questions properly and get them correctly. 12:56 Let’s go into Gi. 12:59 It’s the opposite of Gs. 13:01 Inhibitory. 13:02 So, this brings us to somatostatin. 13:05 The really only hormone that we’ve discussed thus far that does what? Inhibits the release of growth hormone from your anterior pituitary. 13:12 Once again, somatostatin from hypothalamus inhibits the release of growth hormone from the anterior pituitary. 13:18 Last time we talked about this – so say that your patient has acromegaly. 13:21 What does your patient look like? Acromegaly. 13:24 Older or younger? Older. 13:26 Acromegaly. 13:27 Tall or wide? Just keep it simple. 13:31 Wide. 13:31 What do you mean wide? Wide hands. 13:34 “Hey, doc, my hand size seems to be increasing every couple of months.” Welcome to acromegaly. 13:39 What else? What about their jaw? Think of Sylvester Stallone. 13:44 What about his jaw? It’s pretty perfect, isn't it? So, I’m talking about jaw in which it is extremely masculine. 13:53 Welcome to acromegaly. 13:54 Right? So, what kind of drug might you want to use, so that you slow down the release of your growth hormone from that functioning adenoma from the anterior pituitary? A somatostatin analog such as octreotide. 14:07 Okay. Tell me about acetylcholine. 14:09 Acetylcholine works through Gi if your beta-1 receptors in the heart cause your heart to beat faster. 14:17 What particular branch of the ANS is going to slow down the heart? Good. 14:22 Parasympathetic. 14:23 And what’s the name of that receptor on your heart that slows things down? M2 receptors. 14:29 Welcome to Gi. 14:30 Let’s move on. 14:32 We have Gq. 14:34 What does Gq mean to you? As soon as you hear Q, you should be thinking about contraction. 14:39 Q, contraction, if that helps you. 14:42 What do you mean contraction? Contraction in terms of your blood vessel. 14:45 Welcome to vasoconstriction. 14:47 Take a look at some of these hormones that are responsible for contraction. 14:50 We have oxytocin. 14:52 What’s that contracting once again? It brings us back to that baby that was suckling or during delivery what happened. 14:58 Oh, yeah, contraction in the myoepithelial cells in the breast of a female, so you can breast-feed. 15:03 Or you have the uterus that brings about contraction, so you can deliver the child. 15:07 Welcome to oxytocin and Gq. 15:10 What does Gq mean to you in biochem? Work with me. 15:13 You've done this already. 15:13 I'm just walking through quickly. 15:15 IP3. 15:16 Calcium, calcium and calcium. 15:18 ADH, which one is this? Do not you daresay kidney. 15:24 Vasopressin, contracting whom? Blood vessels. 15:29 You call this vasoconstriction. 15:32 Ask you another question. 15:34 Dehydrated state or once again are you in a state of fluid overload in which you’re releasing ADH? Oh, yeah, dehydrated. 15:42 Most likely, your blood pressure is going to be – well, maybe perhaps a little bit lower. 15:46 Why? You’re dehydrated. 15:48 What do you want to do with your blood vessel? Vasoconstrict. 15:51 Are you putting this together? There is V1 receptor. 15:54 Why V1? Vasopressin. 15:57 Gq. 15:58 And we have TRH and GnRH and we have ACH (acetylcholine). 16:02 But, here, I want you to focus upon M3. 16:06 M3, why? Where do you find M3 please? Parietal cells in the stomach. 16:13 Parietal cells in the stomach. 16:15 Why in the world – well, let me ask you something else. 16:18 When you talk about digestion, what’s responsible for acid release into your stomach, parasympathetic or sympathetic? Remember? Parasympathetic. 16:33 What’s the name of that cranial nerve that stimulates your parietal cell or could contribute to further acid release into the stomach? Good. 16:43 You're talking about your vagus, right? Vagal. 16:48 That vagal tone releasing acetylcholine, working upon M3 receptors via Gq, assist you or contributes to acid release into the stomach. 17:01 Obviously, Gastrin will be the most important of the stimuli, but acetylcholine plays a huge role. 17:09 Speaking of which, there is Gastrin. 17:11 Gastrin also works in parietal cells, so that you release acid from your parietal cell.
About the Lecture
The lecture Cell Surface Receptors by Carlo Raj, MD is from the course Introduction to the Endocrine System.
Included Quiz Questions
Which malignancy is managed with a tyrosine kinase inhibitor?
- Chronic myeloid leukemia
- Small-cell lung cancer
- Cutaneous T-cell lymphoma
- Colorectal adenocarcinoma
- Classical Hodgkin lymphoma
In screening for growth hormone pathology, why is measuring insulin-like growth factor 1 (IGF-1) more clinically relevant than growth hormone (GH)?
- IGF-1 levels show less daily fluctuation than GH.
- IGF-1 is released from the liver.
- GH is released in a constant stream.
- GH is not released in high enough quantities.
- IGF-1 can be controlled with insulin.
What best describes the sequence of events after hypothalamic osmoreceptors sense an increase in serum osmolarity?
- Vasopressin is released from the pituitary, binds to kidney V2 receptors, activates Gs protein, and increases cAMP.
- Vasopressin is released from the pituitary, binds to kidney V2 receptors, activates Gs protein, and decreases cAMP.
- Vasopressin is released from the pituitary, binds to kidney V2 receptors, inhibits Gs protein, and decreases cAMP.
- Vasopressin is released from the pituitary, binds to kidney V1 receptors, activates Gs protein, and increases cAMP.
- Vasopressin is released from the pituitary, binds to kidney V1 receptors, inhibits Gs protein, and increases cAMP.
Which hormone is released in response to hypocalcemia?
- Parathyroid hormone
- Glucagon
- Follicle-stimulating hormone
- Luteinizing hormone
- Somatostatin
Which substance works on both Gi and Gq receptors?
- Acetylcholine
- Gastrin
- Glucagon
- Somatostatin
- TSH
Inhibition of what prevents the degradation of cAMP and may enhance gluconeogenesis by glucagon?
- Phosphodiesterase
- Cortisol
- G-protein
- Adenylate cyclase
- Protein kinase A
Which hormone exerts its effect by decreasing the levels of cAMP through an inhibitory G protein?
- Somatostatin
- Insulin
- Adrenocorticotropic hormone
- Thyroid-stimulating hormone
- Glucagon
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Great Lecture! Brings the connection between the receptors and their activities in a way that is easy to comprehend and recall. Very well organized for a lecture under 20 minutes!
I love Dr. Raj's style of teaching! Very clear and motivating introduction! My only recommendation would be to add diagrams along with the description of the receptors. I personally find them very helpful in remembering the downstream functions
Simple is better! Straight to the key-points and very well discussed!