Playlist
Show Playlist
Hide Playlist
Celiac Disease in Children
-
Slides CeliacDisease Pediatrics.pdf
-
Download Lecture Overview
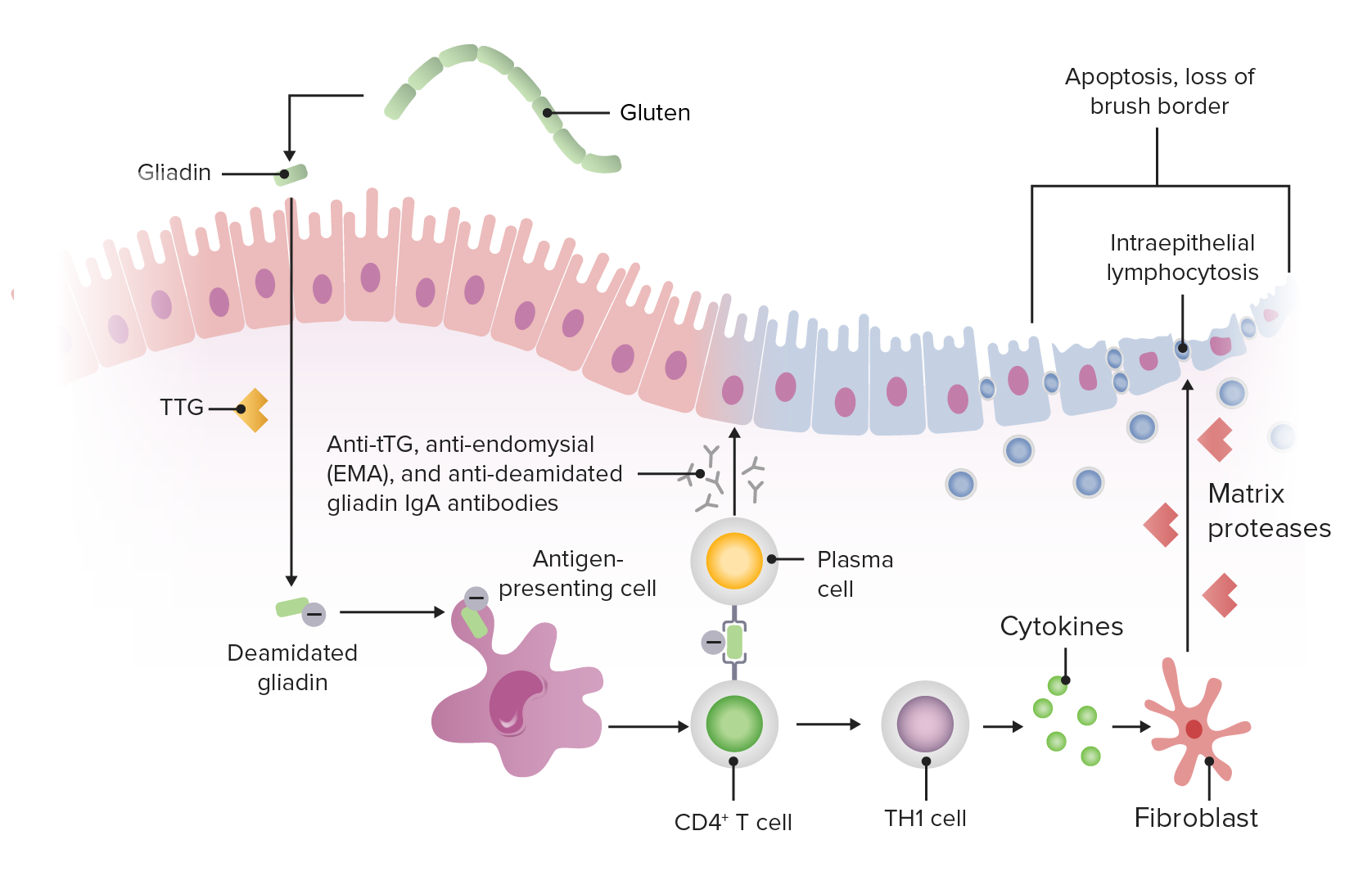
00:02 In this lecture, we’ll talk about celiac disease. 00:06 So here’s a classic case. 00:07 An 18-month-old boy presents to the pediatrician’s office for a visit. 00:12 His mother is concerned and reports that he’s been losing weight, has diarrhea, and is a bit irritable. 00:20 So, losing weight, diarrhea, irritability, what would you do? Well, I’d be worried about celiac disease. 00:30 Celiac disease is a T cell-mediated inflammatory disorder of the small intestine. 00:37 It’s an allergic response to gluten in the diet. 00:43 It’s caused by ingested gluten such as the protein found in bread. 00:50 Patients do have a genetic predisposition for this problem. 00:55 And it’s estimated that it’s occurring in approximately half to 1% of the general population. 01:02 So this is a fairly common problem. 01:06 Typically, this can present in younger children or in older children, and there’s a wide spectrum of severity. 01:14 Some people with this disease will present completely asymptomatically. 01:19 Other people have very severe limitations in what they can eat. 01:24 So, younger children may present with GI symptoms but really after they get gluten in their diet. 01:32 This would be an unheard of condition in the child who is under four months of age unless for some reason, the parent was feeding them a cereal that wasn’t rice cereal, such as oatmeal. 01:44 These patients may present with chronic diarrhea, they may present with poor weight gain or a weight loss, they may have vomiting, they often will have malnutrition. 01:55 It’s not just that they’re only eating gluten, it’s that the irritation of the bowel wall is preventing absorption of other important nutrients that the child may well have in his or her diet. 02:08 Oftentimes, children have behavioral changes such as irritability or fussiness, which is associated with their abdominal pain. 02:17 In older children, patients may have nausea, abdominal pain. 02:23 They may experience bloating. 02:25 They may obtain constipation as well. 02:29 And they may also have intermittent diarrhea. 02:32 So as you can see in older children, it’s a whole bunch of relatively nonspecific abdominal complaints. 02:40 The challenge is that in older children, abdominal pain and other nonspecific pains are quite common. 02:48 The majority of third-graders will have reported abdominal pain in the last week, and these are normal third-graders. 02:57 So, distinguishing a child with celiac disease and a child with abdominal pain can be a little bit tricky. 03:04 If a parent is coming to you with nonspecific GI complaints, celiac disease should come to mind. 03:12 Now, one extra intestinal manifestation of celiac disease that is important to recognize is dermatitis herpetiformis. 03:21 This has nothing to do with herpes. 03:23 It just was believed when it was first named to look a little bit like herpes. 03:27 And you can see that a tiny bit here on this slide. 03:30 This problem occurs in 15% to 25% of patient with celiac disease, but it’s really more common in older people than in younger children with the disease. 03:41 These patients will present with multiple excoriated papules, erosions, and crusts just like our picture here. 03:50 It’s typically over elbows and knees, extensor surfaces, but also can be found on the trunk. 03:57 And if it is to be biopsied, it will reveal IgA autoantibodies in the dermal papillae. 04:06 Complications of celiac disease included, as stated before, malnutrition. 04:12 And this malnutrition in children presents with impaired growth, and this may be how we pick it up. 04:18 Additionally, there is a small cancer risk in particular lymphoma of the intestinal wall that can happen in patients with unchecked celiac disease, and this is why we’re not sure whether we need to treat, and suspect, we do need to treat asymptomatic individuals as well. 04:38 So, how do we test for it? If it’s so nonspecific, do we have a test that’s reasonably good? And the good news is we do. 04:45 So, the first line test is called the tTG or tissue transglutaminase test. 04:51 This is an IgA antibody directed against transglutaminase. 04:57 This is one of the many IgAs in the body. 05:00 So, when we get this test, we also get a total IgA because if a patient is IgA deficient, they may have celiac disease but a relatively low tTG just because they’re deficient of IgA. 05:16 And here’s the rub. 05:18 IgA deficiency is associated with celiac disease. 05:22 So, we really have to get both levels. 05:24 We get a tTG, if it’s elevated, it’s abnormal, they have celiac disease. 05:29 If it’s low and they have low IgA antibodies, they may have celiac disease. 05:34 If the tTG is low and the IgA is normal, they likely do not. 05:39 It should be clear that we obtain this serologic testing while the patient is eating gluten. 05:45 If you put them on a gluten-free diet and then test them, you’re likely to get a false negative test. 05:53 If they test positive for the tTG-IgA test, a biopsy is needed to establish the diagnosis. 06:01 Once again, they need to be on the gluten in their diet when the biopsy is obtained to make a definitive diagnosis. 06:10 This small bowel mucosa reveals villous blunting and increased intraepithelial lymphocytes. 06:17 This is a key point for you to remember for your tests. 06:21 First, get the blood test while on gluten in the diet, then obtain a bowel mucosa biopsy and look for the typical finding of bvillous atrophy and crypt hyperplasia. 06:33 And you can see a picture of these blunted villi right here on this slide. 06:38 Treatment is a total lifestyle modification. 06:42 These patients must be placed on a lifelong gluten-free diet. 06:47 That means avoiding wheat, rye, and barley. 06:52 As this condition is becoming more prevalent in the United States, and why that is happening may be a discussion for another time, but likely as a combination of people growing up in a non-immunogenic way during their first year of life and genetic predisposition. 07:11 But if you make this diagnosis, you need to be off these elements for your diet for your life. 07:17 What we are finding is more and more people are becoming understanding of the gluten-free diet, and there are more and more dietary options out there, but patients need to be weary. 07:28 So, here are things patients can eat. 07:31 Go ahead and eat fruits and vegetables and meat and poultry and fish and seafood and dairy and beans and legumes. 07:38 You can eat flours obtained from certain types of grains that do not have gluten such as rice. 07:47 Here are some gluten-free grains, and the point is not that you have to memorize that arrowroot is a gluten-free grain. 07:55 The point is that there are many options out there and people with the disease need to be aware of these types of things so that they can adjust their diet accordingly. 08:06 So, things to remember about celiac disease. 08:09 First off, GI symptoms are primarily how they will present, and also behavioral symptoms in the younger children, fussiness, irritability. 08:22 Histopathologic signs are key such as the blunted villi, which you obtain on your testing. 08:30 Dermatitis herpetiformis is a pathognomonic rash for this disease, and if you see it, sure makes that diagnosis a lot easier. 08:38 And treatment is lifelong a gluten-free diet. 08:43 Thanks for your attention.
About the Lecture
The lecture Celiac Disease in Children by Brian Alverson, MD is from the course Pediatric Gastroenterology. It contains the following chapters:
- What is Celiac Disease?
- Clinical Presentation
- Signs & Symptoms
- Diagnosis & Pathology
- Management
Included Quiz Questions
What kind of rash do children with celiac present with?
- Dermatitis herpetiformis
- Eczema herpeticum
- Erythema multiforme
- Erythema marginatum
- Atopic dermatitis
Celiac disease is caused by an immune reaction against gluten in the diet, which is mediated by which of the following?
- T cells
- B cells
- Plasma cells
- Mast cells
- Basophils
What would you find if you were to biopsy a lesion of dermatitis herpetiformis?
- IgA antibodies in dermal papillae
- IgG antibodies in dermal papillae
- IgA antibodies in the dermal-epidermal junction
- IgG antibodies against hemidesmosomes
- Different classes of antibodies against desmosomes
Which of the following tests is appropriate initially for a suspected case of celiac disease while they are still on a gluten-based diet?
- Tissue transglutaminase IgA antibodies and Total IgA level
- Tissue transglutaminase IgA antibodies
- Total IgA level
- Stool microscopy
- There is no specific lab test
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
me gustó el video esta muy bien explicado y creo que esta todo lo necesario que necesitamos saber sobre enfermedad celiaca
Excellent lecture on an important topic in pediatrics, well explained, easy to remember. Just my colleague, I did not know about the skin manifestation.
I like that everything is very well explained and we are given only the information we need to know. Thank you. I didn't know about the herpetiformus dermatitis, for some reason they don't always mention it in our books.