Playlist
Show Playlist
Hide Playlist
Celiac Disease: Clinical Presentation, Diagnosis, and Treatment
-
Slides GIP Celiac Disease.pdf
-
Reference List Pathology.pdf
-
Download Lecture Overview
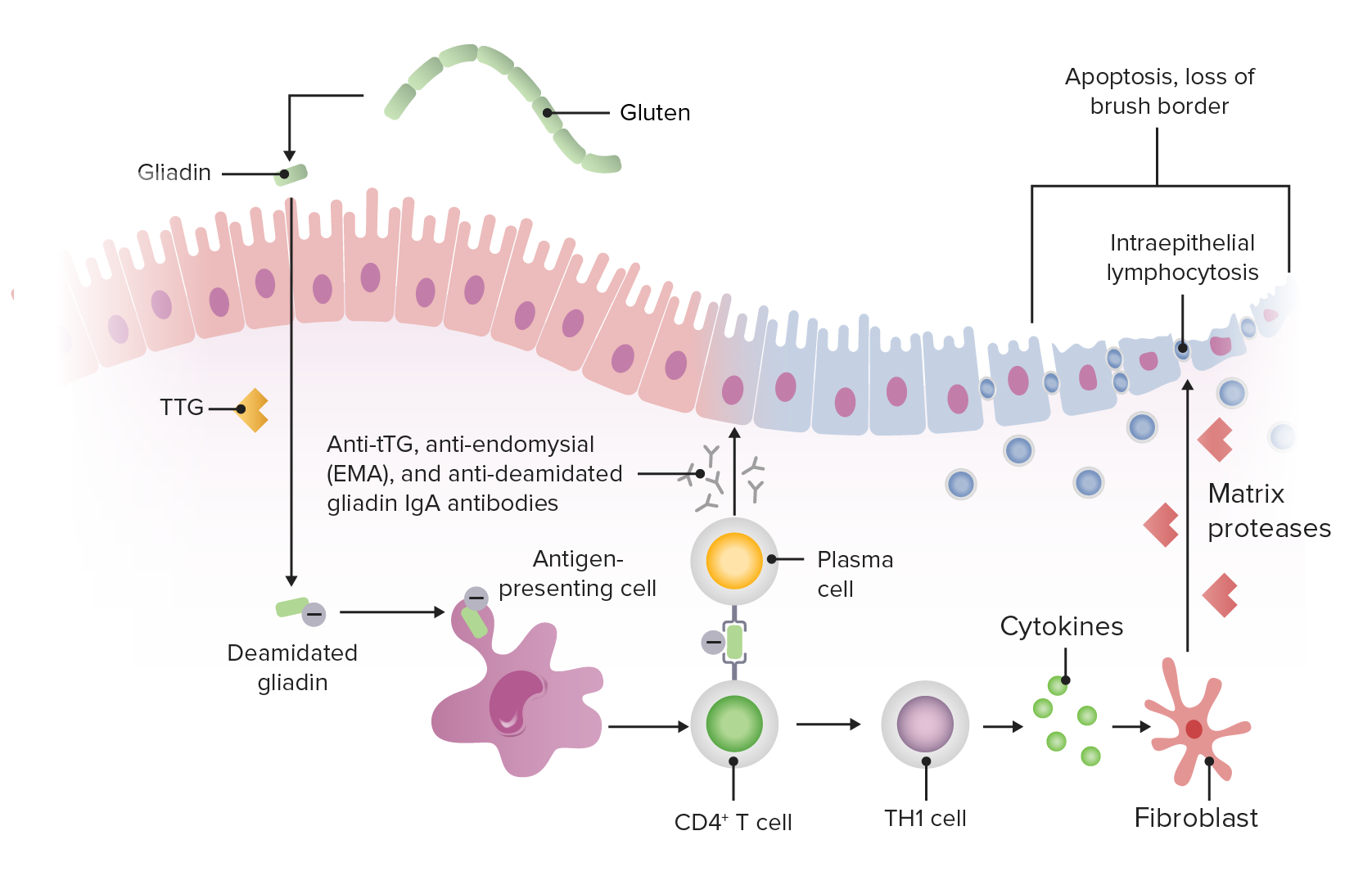
00:01 The clinical presentation. 00:03 So, the GI symptoms, we'll come back to the other manifestations in a moment, but the GI symptoms are going to be exactly what you expect. 00:11 You are not absorbing nutrients, you're going to have diarrhea, it's going to be the most common. 00:15 You will have steatorrhea. 00:17 So basically you're not absorbing fat, so you'll have floating stool that is incredibly foul smelling. 00:24 There will be bloating and flatulence. 00:26 That's because all those nutrients that you are not absorbing, the bacteria are metabolizing and fermenting to make gas. 00:33 They'll make hydrogen gas, they'll make CO2, And then with that bloating, with that basically gas expanding the bowel that will be felt as abdominal cramping. 00:46 The extra intestinal manifestations include things associated with malnutrition. 00:51 You'll be tired, there will be weight loss, there will be muscle wasting. 00:55 Little kids will have so called failure to thrive, they won't hit their milestones in terms of weight and height. 01:02 Because we are not probably absorbing iron and folate and B12 appropriately, there will be various forms of anemia that are seen. 01:11 We won't be able to absorb vitamin K, that's a fat soluble vitamin. 01:16 And as a result of that we may have a bleeding diathesis because we're not making the appropriate procoagulant factors in the liver. 01:25 Atrophic glossitis and oral mucosal lesions are due to folate and B12 deficiencies and can be seen in other settings. 01:34 But it may be something that occurs with celiac disease. 01:37 Peripheral cutaneous dermatitis herpetiformis may also be seen. 01:42 Making the diagnosis. 01:43 So a lot of this is clinical. 01:46 Yeah, I eat this food and I have a heavy pasta dish and I wash it all down with beer. 01:53 And I feel terrible for the next week. 01:57 Okay, that's a presumptive kind of story that you will often hear but things that you can look for that it's gonna be a little bit more specific perhaps, you'll see edema. 02:06 Well, that's because you are not synthesizing albumin appropriately because you are malnourished. 02:12 There will be increased fecal fat. 02:14 That's actually a kind of a pain in the rear end. 02:17 To accumulate that stuff, you actually have to have the patient collected for certain period of time. 02:22 Your patients won't like that. 02:24 So you may have a presumed fecal fat. 02:27 But it's going to be really hard in most cases to get your patients to go along with the actual process. 02:33 You may have prolonged coagulation times. 02:35 You're not making the normal procoagulation factors, because you're not absorbing vitamin K. 02:42 A microcytic anemia associated with iron deficiency and macrocytic anemia associated with folate or B12 deficiency. 02:48 And then we can look specifically for those biomarkers that I talked about. 02:51 So anti transglutaminase antibody, the IGA antibodies have that specificity is reasonably sensitive and specific for making the diagnosis of celiac disease. 03:05 Again, not causal of the primary GI manifestations, but are good biomarker and probably are involved in the peripheral cutaneous dermatitis herpetiformis. 03:20 And then to nail it, this is where pathology comes in. 03:24 Hurray for pathology. 03:25 We'll do a biopsy. 03:26 We will send a bioptome all the way down through the stomach through the duodenum into the small bowel and we'll take nips of tissue. 03:35 This will involve obviously an upper endoscopy. 03:37 So the endoscopic features, the mucosa looks atrophic. 03:41 There may be deeper fissures. 03:43 There are a whole variety of things that we can see if you're a trained endoscopist. 03:48 The histology is what you should be paying attention to. 03:51 We're going to see loss of the villi. 03:53 Remember that very first slide where you know we have beautiful villi sticking up in the air and then right next to it, not any villi. 04:00 Same thing is seen on biopsy. 04:03 And so that really helps in making the diagnosis. 04:06 We may also see that the bowel is trying to compensate, and we may see very deep crypts. 04:13 We will also see increased intra epithelial lymphocytes, inflammatory cells that have been activated and recruited to this location. 04:21 And so the lamina propria may be expanded with lots of little blue dots. 04:25 If there is a normal biopsy that pretty much excludes the diagnosis of celiac disease, and then we have to start thinking about other causes. 04:35 So managing this. 04:37 Get rid of the gluten. 04:40 It's kind of a pain. 04:42 But increasingly, especially in developed countries, you can find a lot of gluten free pastas and other dishes so that you don't have to quit eating things that you enjoy. 04:57 Approximate 70% of patients probably even more than that will have clinical improvement within a couple of weeks once they go on a gluten-free diet. 05:05 However, unfortunately, there are about 5% of patients who may not respond within that 2-week period or ever who have already had significant damage to their GI tract, and may have to be treated in other ways. 05:20 We'll get to that in a moment. 05:22 Remember, a negative biopsy pretty much rules this out. 05:26 So we need to consider alternative diagnoses and other things that can manifest in very similar fashion or irritable bowel syndrome, bacterial overgrowth, a primary pancreatic insufficiency, or an entity called microscopic colitis, where we have increased inflammation, again, probably autoimmune in nature, but not caused by glutens or gliadins. 05:49 In settings, where we think that there is an ongoing and severe inflammatory component, we may consider immunosuppression either with glucocorticoids or other agents. 06:01 The prognosis for those who respond overall is excellent. 06:05 You just need to stay off glutens and find alternatives. 06:09 For those who don't, we have to consider that ongoing inflammation and ongoing injury to the epithelium with proliferation in the setting of all the reactive oxygen species and other inflammatory mediators increases the risk for lymphoma and increases the risk for GI cancer. 06:28 So we have to then constantly monitor those patients who don't respond. 06:33 There is a variant or a variation on the theme overall of celiac disease called collagenous sprue, where as a result of the ongoing inflammation, we get a intense collagen deposition within the lamina propria. 06:50 And that really significantly impedes normal absorption. 06:53 So the epithelium may actually be intact, but we can't really get those nutrients from the epithelium into the lymphatics and into the small vessels that live in the lamina propria. 07:04 And so the patients will still have severe malabsorption. 07:07 And with really significant length of injury, we can develop scarring that will cause strictures, so you can have bowel obstruction. 07:18 With that we've reached the end of an interesting and important entity for you to recognize and that you will certainly see in many of your patients celiac disease.
About the Lecture
The lecture Celiac Disease: Clinical Presentation, Diagnosis, and Treatment by Richard Mitchell, MD, PhD is from the course Small and Large Intestines Disorders.
Included Quiz Questions
Which immunoglobulin is associated with dermatitis herpetiformis?
- IgA
- IgG
- IgE
- IgM
- IgD
What is the most common symptom of celiac disease?
- Diarrhea
- Constipation
- Hematochezia
- Dyschezia
- Pain
Which hematologic disorder is seen in celiac disease?
- Anemia
- Thrombocytopenia
- Thrombocytosis
- Lymphopenia
- Leukocytosis
What is NOT a histologic finding seen on a biopsy of the small bowel in a patient with celiac disease?
- Condensed nucleoli
- Increased intraepithelial lymphocytes
- Crypt hyperplasia
- Villous atrophy
- None of these answers
What is the initial management for celiac disease?
- Gluten-free diet
- Low-sodium diet
- PPI twice daily
- NSAID daily
- PPI and NSAID daily
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |