Playlist
Show Playlist
Hide Playlist
Case: 68-year-old Man Presenting with Fainting Episodes
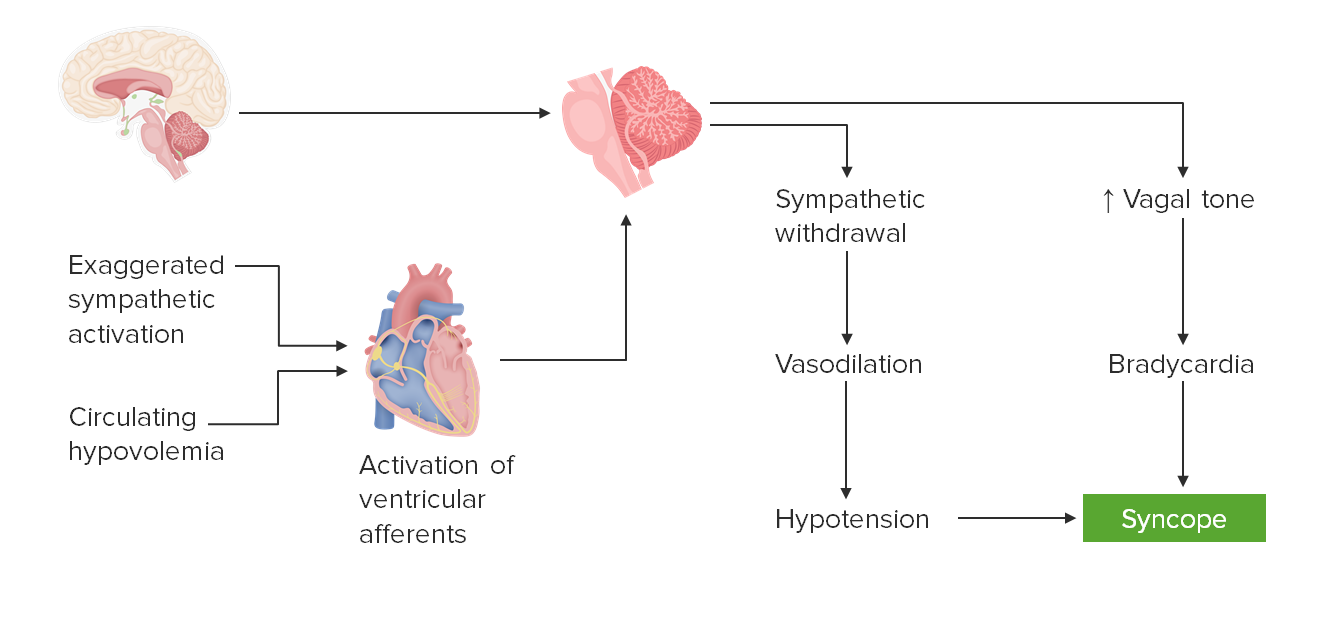
00:01 In this lecture, we'll talk about the approach to presyncope or syncope. 00:05 Let's start with a case. 00:07 A 68-year-old man with a history of hypertension, hyperlipidemia, diabetes, and prior stroke presents for recurrent episodes of dizziness. 00:17 The patient says that for the past two months, when he stands he becomes severely lightheaded and dizzy. 00:23 He says that it feels as if he's having tunnel vision, and one time, he actually passed out. 00:29 In fact, he was told that he slumped over to the ground and began to convulse throughout his body. 00:35 Afterwards, he stood right up and asked what had happened. 00:38 At times, this will develop immediately after he stands, and at other times, it can be about five minutes or so when he's walking around that he'll become dizzy. 00:48 He's on three anti-hypertensives including amlodipine, lisinopril, hydrochlorothiazide, and metoprolol. 00:54 so four medicines, which were started about two months ago. 00:58 Examination is unrevealing with normal cerebellar signs and no nystagmus. 01:04 Blood pressure, when he's lying down is 125/75 with a heart rate of 70 beats/minute. 01:11 And three minutes after standing, his blood pressure drops to 90/50, with a heart rate of 75. 01:17 So what's the diagnosis? Well, there are many features of this case that we should be attuned to. 01:24 When when we approach dizziness, one of the things we focus on is the timeline of onset. 01:29 This began about two months ago, it's subacute and onset. 01:33 It's not acute beginning within the last one day. 01:36 It's not chronic going on for months or years, but it started within the last several months a subacute onset condition. 01:44 The second factor is the provoking factors or provoking signs. 01:49 And this is also important when evaluating anyone with dizziness. 01:53 These episodes begin when he stands. 01:56 And this could point us in the direction of orthostatic hypotension, or when the patient stands their blood pressure drops, which is one type of syncope or presyncope. 02:07 We also focus on the patient's description, which again is important when evaluating any patient with dizziness. 02:14 This patient describes lightheadedness, a fainting feeling. 02:18 He passed out with one of the episodes and after passing out, convulsed. 02:23 This gives a description of syncope or presyncope with one event that may have been a convulsive syncopal event. 02:31 And so the patient's description is critical in evaluating this vignette. 02:37 So what is the most likely diagnosis? Is this a cerebellar stroke? A seizure? BPPV or Benign Paroxysmal Positional Vertigo? Syncope? Or is it labyrinthitis or vestibular neuritis? Well, it doesn't sound like labyrinthitis or vestibular neuritis. 02:55 Those are two causes of vertigo. 02:57 And this patient's description is consistent with syncope. 03:00 He's not describing vertigo. 03:04 What about a cerebellar stroke? This doesn't sound like cerebellar disequilibrium. 03:09 The patient's description is more of a syncopal episode as opposed to a cerebellar disequilibrium. 03:15 It's also not acute and onset. 03:17 This patient's presentation is subacute over several months. 03:20 And we would expect a cerebellar stroke to present acutely. 03:26 This doesn't sound like BPPV. 03:29 The exam findings aren't consistent with BPPV. 03:32 We tend to see nystagmus or a rotary nystagmus. 03:35 It is episodic. 03:37 And BPPV is an episodic condition, but patients frequently described vertigo and room spinning that is initiated or provoked by head turning. 03:46 This patient describes episodes that are initiated by standing. 03:50 So BPPV is not our favored diagnosis. 03:55 What about a seizure? This patient describes seizure. 03:57 His episode of convulsion was convulsive syncope. 04:01 The description where he fainted first, and then convulsed is more consistent with convulsive syncope. 04:07 Seizures begin with shaking or convulsing first, followed by passing out. 04:12 There was also no post-event confusion as we would expect from a seizure. 04:17 So the right answer here is syncope. 04:19 The patient describes tunnel vision and lightheadedness, were which are common descriptions of syncope. 04:25 The episodes are provoked by standing up, which is common from orthostasis, and the presentation overall is suggestive of an orthostatic neurally mediated syncope.
About the Lecture
The lecture Case: 68-year-old Man Presenting with Fainting Episodes by Roy Strowd, MD is from the course Vertigo, Dizziness, and Disorders of Balance.
Included Quiz Questions
Which statement is the most accurate with respect to orthostatic hypotension?
- Treatment significantly improves the condition in most cases.
- Patients experience episodes of orthostatic hypotension when laying down too quickly.
- Medications will not cause this condition.
- Orthostatic hypotension is always benign and rarely warrants further testing.
- Orthostatic hypotension has a progressively worsening course.
Which statement is the most accurate with respect to syncope?
- Tunnel vision is a commonly reported symptom.
- The underlying cause of presyncope will never cause syncope.
- Patients typically describe a feeling of drunkenness and a loss of coordination.
- Convulsions precede the loss of consciousness.
- Head turning is a common provocative maneuver.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Good summary of a difficult topic. The key points are covered well.