Playlist
Show Playlist
Hide Playlist
Case: 67-year-old Woman with Gait Dysfunction
-
Slides Approach to Dysequilibrium Cerebellum.pdf
-
Download Lecture Overview
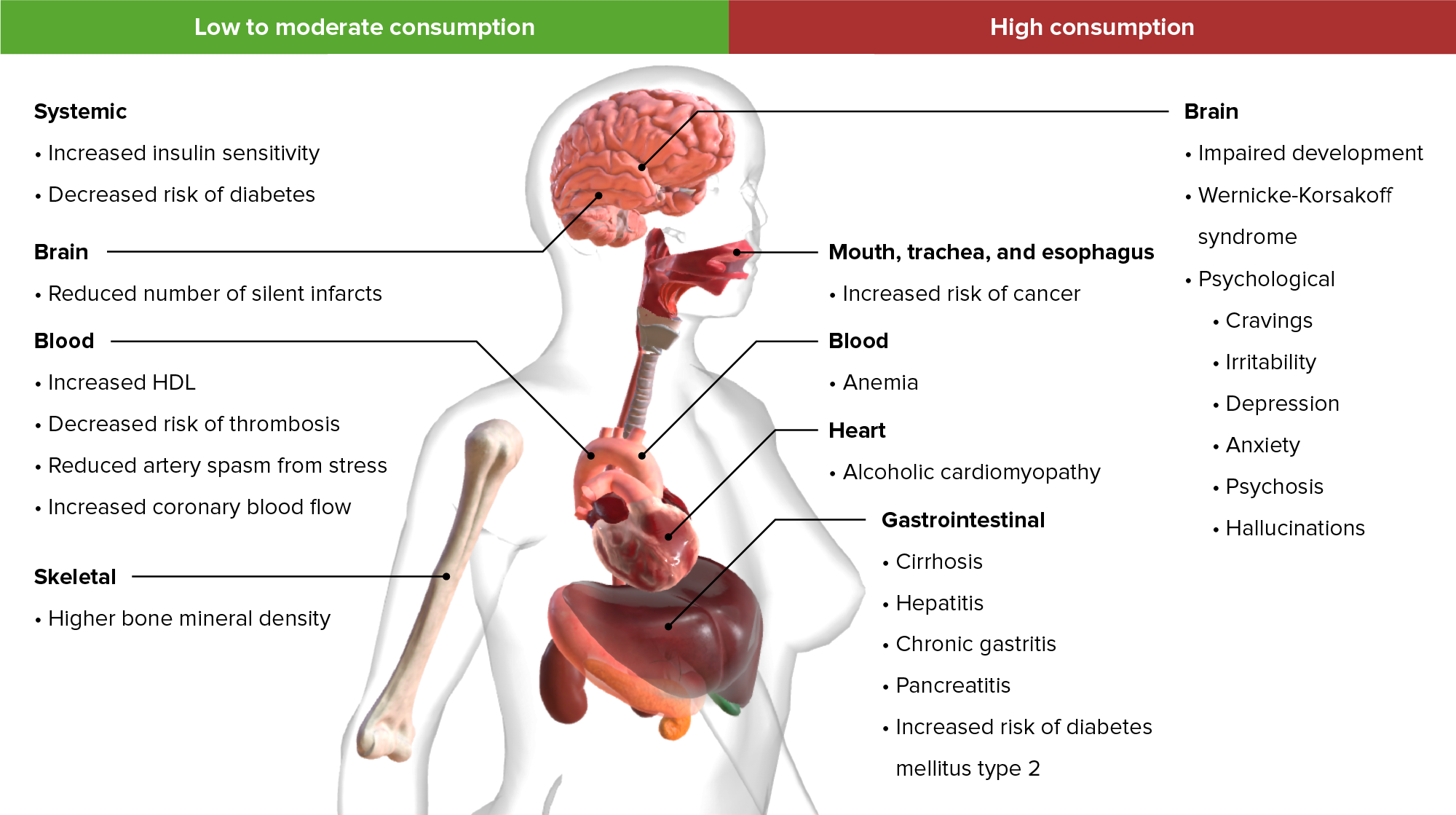
00:01 So let's understand the clinical relevance of the cerebellar hemispheres, subcortical white matter and gray matter by focusing on a case. 00:09 This is a 67-year-old African American woman who presents with a two-year history of progressive gait dysfunction, which became progressively worse after a recent hospitalization when she was noted to have severe truncal ataxia. 00:24 The ataxia is improved at rest and worsens considerably when she's sitting on the bed. 00:29 She's swaying from side to side. 00:31 Or when she's standing or walking, so really with any movement. 00:35 Her exam shows a severe wide base gait, which we see with cerebellar problems, horizontal nystagmus and saccadic overshoot, where the eyes are not coordinated. 00:46 when you look in one direction or the other. 00:48 Finger-to-nose-to-finger test is slightly abnormal with mild overshoot, and again we see or seeing problems with coordination. 00:56 An MRI is performed and reveals cerebellar atrophy, preferentially affecting the superior vermis more than other areas of the cerebellum. 01:05 So which of the following is the most likely diagnosis? Well, there are a number of key features of this case. 01:11 The first is the timeline of onset. 01:13 There's a progressive two-year history of this cerebellar disorder. 01:18 That means it's chronic and onset, and that already us thinking about some of those acquired causes of cerebellar dysfunction. 01:26 The second is the propagating factors. 01:28 This patient's dizziness or balance problem is provoked by moving and improved with rest. 01:34 That's very common with cerebellar pathology. 01:37 It can be seen with vertigo and vestibular pathology. 01:40 But that movement component is something that the cerebellum does. 01:43 So when we see problems that are provoked by movement, we want to think about the cerebellum. 01:49 In addition, this patient's exam shows problems with cerebellar dysfunction, wide base gait, nystagmus, saccadic overshoot, and difficulty with finger nose finger, are all cerebellar signs. 02:00 That means this dizziness problem is a problem with the cerebellum and disequilibrium. 02:06 Let's look more closely at this patient's MRI scan. 02:10 We see atrophy of the cerebellum, and here we're looking at a midline cut. 02:15 This is a sagittal MRI, looking right at the middle of the cerebellum, right at the area of the vermis. 02:21 We see atrophy across the cerebellum, but preferentially affecting the upper part of the cerebellum, that superior lobe, that top lobe along the vermis. 02:31 And there are certain conditions that will affect only the hemispheres, only the vermis, and one that we think about that has a predilection for the superior cerebellar vermis. 02:42 So what's the most likely diagnosis for this patient? Is this a post-infectious cerebellitis, a Chiari malformation, alcohol-related cerebellar ataxia, or a cerebellar stroke? Well, this doesn't sound like a post-infectious cerebellitis. 02:57 Typically, we would recognize the initial infection, which we don't see in this case. 03:01 Post-infectious cerebellitis is an inflammatory condition. 03:05 It's often subacute and onset, and this is chronic and onset. 03:10 It's been going on over multiple years, or two years for this patient. 03:14 In addition, and most importantly, post-infectious cerebellitis typically affects the hemispheres. 03:19 And this is a problem that is very specific to the cerebellar vermis. 03:23 So post-infectious cerebellitis is not the most likely diagnosis in this patient. 03:30 Cerebellar stroke is also unlikely for this patient. 03:33 Strokes present acutely. 03:35 And again, this patient's symptoms was chronic and onset over two years. 03:39 In addition, we often see strokes affecting the lateral circumferential vessels that feed the cerebellar hemispheres, and would present with prominent appendicular dysmetria and ataxia as opposed to vermis dysfunction. 03:56 Chiari malformation often presents with headache and really uncommonly presents with an ataxic syndrome. 04:02 A Chiari is a description of malformation for the cerebellar tonsils descending down below the foramen magnum. 04:10 We don't see that on imaging on that midline cut, and it doesn't have this type of presentation. 04:16 And so this patient is suffering from alcohol-related cerebellar ataxia. 04:20 The patient has an ataxic syndrome with a predilection or that superior vermis, which is something that's very typical for alcohol-related cerebellar syndromes. 04:31 So let's talk a little bit more about Cerebellar Vermis Atrophy in Alcoholism. 04:35 This is the clinical relevance of understanding, how the cerebellum is organized? In terms of definition, this is a primary long-term effect of chronic alcoholism, which results in degeneration or atrophy of the cerebellum. 04:49 The entire cerebellum is involved and alcohol has a predilection for affecting the cerebellar purkinje fibers, but the superior vermis is most specifically affected, and often one of the earliest areas that we see. 05:02 Patients typically present with a slowly progressive gait dysfunction and truncal ataxia. 05:07 The vermis is involved in truncal coordination. 05:10 And that's more so affected than the appendicular functions, as in this case. 05:15 On imaging, MRI shows atrophy of the diffusely across the cerebellum, but preferentially affecting the superior cerebellar vermis more so than the hemispheres. 05:25 And pathologically, what we see is loss of cerebellar and purkinje cells primarily in the superior vermis, as well as the vestibular nuclei. 05:33 And so we can see, eye movement dysfunction as was present in this case, and can be seen in up to 43% of patients. 05:39 So it's common, something we look for.
About the Lecture
The lecture Case: 67-year-old Woman with Gait Dysfunction by Roy Strowd, MD is from the course Vertigo, Dizziness, and Disorders of Balance.
Included Quiz Questions
Which of the following would suggest cerebellar pathology?
- Nystagmus
- Vertigo
- Unequally dilated pupils
- Bilateral leg weakness
- Narrow gait
Which region of the cerebellum is most commonly impacted by a stroke?
- Lateral hemispheres
- Subcortical gray matter
- Flocculonodular lobe
- Inferior vermis
- Superior vermis
Which statement is the most accurate with respect to alcohol-related cerebellar ataxia?
- The superior vermis is highly susceptible to alcohol toxicity.
- Patients show an acute onset of symptoms.
- Symptoms are isolated to the appendages.
- MRI usually shows isolated degeneration of the lateral hemispheres.
- The lateral hemispheres are not susceptible to alcohol toxicity.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |