Playlist
Show Playlist
Hide Playlist
Case: 57-year-old Woman with Seizure-like Episodes
-
Slides Seizures Epilepsy Partial Onset Epilepsy & Top Ten Seizure Treatment Tips.pdf
-
Download Lecture Overview
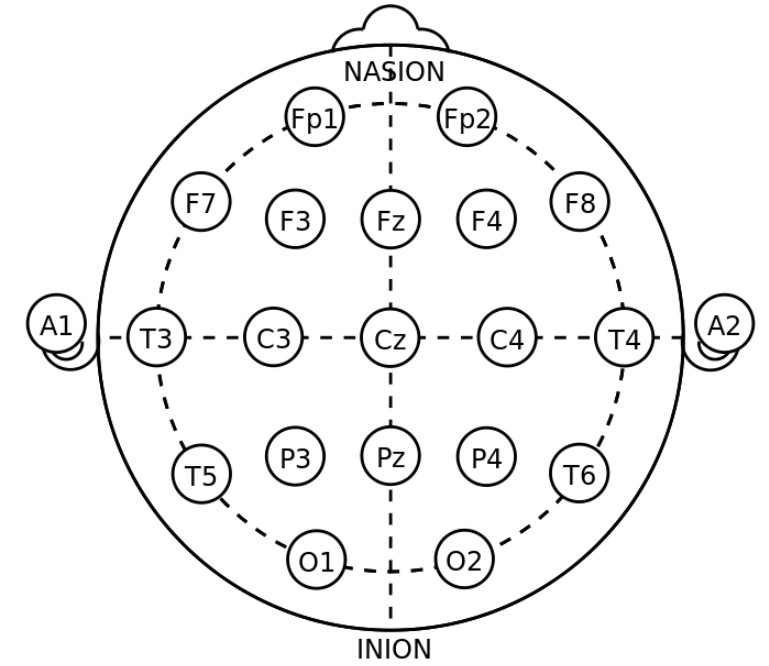
00:01 In this lecture, we'll talk about partial-onset epilepsy and specifically focus on the treatment for partial-onset epilepsy. 00:10 Let's start with a case. 00:12 This is a 57-year-old woman who presents for evaluation of seizure like episodes. 00:17 The first spell occurred while at home at the table when she developed a severe pain in her right upper quadrant that progressed to a rising sense of nausea, and then her husband saw her slumped over in her chair. 00:31 This lasted 30 seconds to a minute. 00:32 And afterwards, she felt "hot on the inside", and was "clammy and disoriented". 00:38 She had a second spell that was very similar to the first and occurred at a restaurant. 00:43 During which the patient felt hot, clammy, flushed, developed this rising nausea from the right upper quadrant, followed by slumping over in her chair. 00:52 By presentation, she had multiple more spells, all beginning with the rising nausea, progressing to lightheadedness, and a near sense of passing out. 01:02 But did she did not actually pass out. 01:04 Again, we're seeing that stereotypic nature to these episodes. 01:09 There's no history of febrile seizures, encephalitis, meningitis, head injury, with or without loss of consciousness, no motor vehicle accidents, no family history of seizure, no staring spells as a child, no reported nocturnal events, and no myoclonus is reported. 01:25 So what's the diagnosis? Well, as with other seizures, we can walk through the typical features that we evaluate for these patients. 01:34 What happened before the episode, during the episode, after the episode, and any wildcard features? Prior to the episode for this patient, she describes this rising sense of nausea. 01:46 It's stereotypic. 01:47 It happens before every single episode, and is consistent with an aura. 01:53 That aura here may localize to the medial temporal lobe. 01:58 The second thing we look at is the event. 02:00 The description of the event. 02:02 She slumped over in a chair or described slumping over in the restaurant, in a chair. 02:07 That slumping over altered awareness puts us into a certain category of possible seizure. 02:13 And then after the event, particularly with the first one she's disoriented or confused, which is consistent with an epileptic phenomenon. 02:21 There are also some wildcard features here. 02:23 She's had multiple spells, all stereotypic, and really the review of seizure symptoms is all negative for any potential nidus that would have contributed to this. 02:33 So what's the diagnosis? Is this seizure/epilepsy, syncope, TIA, or GI pathology? Well, we don't like syncope. 02:42 The clinical description just does not support syncope. 02:45 The events are not provoked by standing. 02:48 and there's not the lightheadedness or fainting appearance. 02:51 It's not convulsive syncope that's described. 02:54 This is inconsistent with the description of syncope. 02:57 TIA. 02:58 TIAs can present with sudden onset of neurologic symptoms, post to your circulation, ischemia can cause sudden alteration in awareness and consciousness. 03:09 But these are very stereotypic in their description. 03:13 This rising nausea happens at the beginning of each of them. 03:16 There's post event confusion. 03:18 They're very short in the description of the actual event itself, which is inconsistent with what we'd see with a TIA. 03:25 And that would be much lower on our differential. 03:28 How about GI pathology? She describes this nausea and this sense of abdominal pain. 03:32 And GI symptoms can be seen as a result of seizure. 03:35 And here with the co-occurrence of all the other symptoms in this patient, we would not favor GI pathology. 03:42 The right answer is seizure or epilepsy. 03:45 These events are stereotypic, meaning the same event occurs in the same way every time. 03:50 That's critically important when we're evaluating these patients and should raise suspicion for a seizure. 03:58 So let's talk about what happened for her. 04:00 She was sent to a cardiologist for a syncope evaluation, had a negative EKG and TTE. 04:06 Except she did have a clinically insignificant Patent Foramen Ovale. 04:09 And a negative tilt table test. 04:12 She was sent to a GI physician who performed a CT chest, abdomen, pelvis to work up the abdominal pain and rising nausea, which was negative. 04:19 Then had an EGD or an upper endoscopy that was also negative for GI pathology. 04:25 She was then sent to a neurologist where EEG was normal. 04:29 And the MRI was normal except for some subtle chronic microvascular changes on the brain, which are likely unrelated. 04:36 So what treatment would you select? Ethosuximide, levetiracetam, phenobarbital, or the ketogenic diet? Ethosuximide is a great anti-epileptic but it's used primarily for primary generalized epilepsy and specifically for patients with absence epilepsy or childhood absence epilepsy. 04:57 This patient's description is inconsistent with a generalized epilepsy. 05:00 And so ethosuximide would not be the treatment of choice. 05:05 Phenobarbital is a commonly used medication for status epilepticus. 05:09 And the historically was one of our first seizure medications. 05:13 It is used for focal-onset epilepsy. 05:16 And it's typically not used for patients where we're concerned about drug-drug interactions. 05:21 There's a risk of sedation and other side effects. 05:23 And so it's frequently reserved for patients who have refractory epilepsy who fail other therapies. 05:30 How about the ketogenic diet? This is something we do use in epilepsy. 05:34 It's typically reserved for pediatric patients or patients with medically refractory epilepsy. 05:40 And so it would not be the first choice of an intervention for this patient. 05:45 So the right answer here is levetiracetam. 05:47 This is an appropriate treatment for a focal-onset epilepsy, and it's one of the most commonly used medications for a first line agent for new onset epilepsy or seizures.
About the Lecture
The lecture Case: 57-year-old Woman with Seizure-like Episodes by Roy Strowd, MD is from the course Seizures and Epilepsy.
Included Quiz Questions
Which description is the most accurate with respect to partial-onset epilepsy?
- Stereotypic aura with nausea or déjà vu
- Asymptomatic postictally
- Loss of consciousness prior to convulsions
- EEG with simultaneous depolarization
- Ethosuximide is the preferred treatment
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |