Playlist
Show Playlist
Hide Playlist
Case: 50-year-old Woman with Lower Extremity Weakness
-
Slides Diseases of the Spinal Cord.pdf
-
Download Lecture Overview
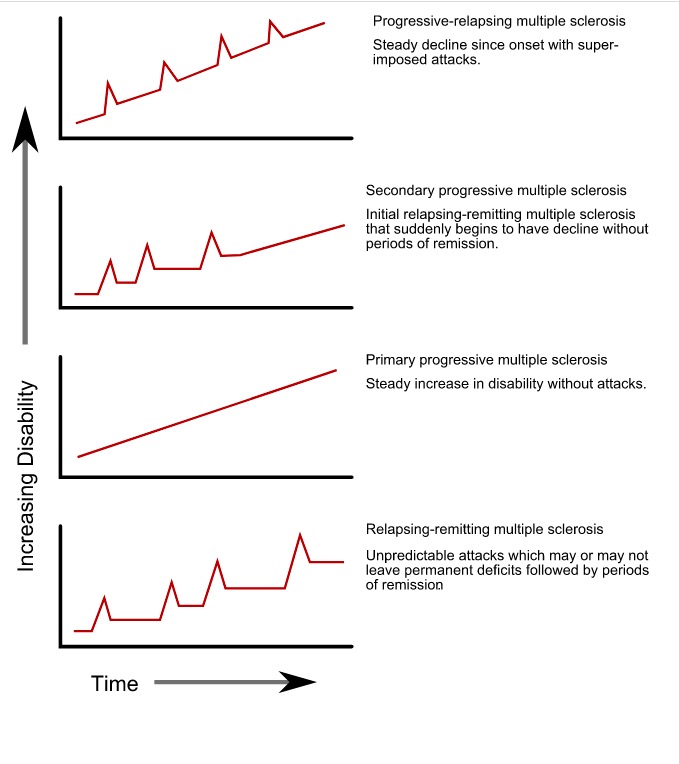
00:00 Now, let's talk about intradural and intramedullary processes affecting the spinal cord, and let's turn to a case. This is a 50-year-old with a past medical history of tobacco abuse who presents to the neurosurgery service for evaluation of lower extremity weakness. The patient suffered a motor vehicle accident several months ago and went to rehab for post acute therapy. She progressed well and got to the point of running upstairs. So, really dramatic improvement after this accident. One week prior to admission she was putting her vacuum cleaner into her car and had sudden bilateral lower extremity numbness and weakness. So the signs and symptoms that are pointing to a spinal cord disorder. The next day, she remained weak and had to use a friend's walker for ambulation. She had 2 episodes of urinary incontinence concerning again for a spinal cord process. Examination shows a paraparesis, weakness below the legs with 4+ strength in the bilateral hip flexors, 4+ dorsi and plantarflexion and normal strength in the arms. So the strength examination supports a paraparesis, weakness below the legs. There is 3+ deep tendon reflexes throughout and clonus at the ankles bilaterally, so hyperreflexia. Upper motor neuron findings. And sensation is decreased to light touch to the mid shin bilaterally which is not inconsistent with the spinal cord process. So when thinking about those key features of this case, the strength exam shows a distribution that's suggestive of a myelopathy, a paraparesis. The reflex exam supports an upper motor neuron process again suggestive that this is likely a myelopathy and the sensory exam is consistent with that as well. We also have this wildcard. Important here that we see evidence of bowel or bladder dysfunction and can see bowel dysfunction which should point towards the need to evaluate the spinal cord. This patient underwent cervical spine MRI with and without contrast and we're looking at that here and here we see a little bit of degenerative change, very mild, in this patient's cervical spine but nothing like what we saw in our prior patient. Here we see increased signal within the spinal cord on the left, that's a T2 image showing edema that is expanding somewhat the cord and internal enhancement. To the right we have a T1 post contrast gadolinium enhanced image and we see enhancement at this region. Something is going on within the spinal cord. This is an intradural intramedullary process and our differential diagnosis would include infectious, inflammatory, or neoplastic causes of this patient's myelopathy. The patient ultimately underwent MRI of the brain and additional sectioning of the spine and on the left we see the MRI of the brain showing multiple old areas of abnormality around the ventricles, periventricular white matter lesions emanating or appearing to emanate from the ventricles. That's something we can see in inflammatory pathology of the central nervous system and specifically in MS. 03:07 And in the spinal cord we see enhancement within the spinal cord itself suggesting an acute process and perhaps acute inflammation affecting the spinal cord. So here we have a process, non-traumatic myelopathy that by MRI and clinical exam is suggestive of an intradural intramedullary process, something affecting the spinal cord itself. These patients require or should undergo CSF sampling to look for an infectious myelopathy versus an inflammatory or autoimmune myelopathy and evaluate for potential neoplastic myelopathy. Angiography MRA or catheter angiogram, spinal angiogram maybe needed and systemic inflammatory markers may also be helpful in these patients. The differential diagnosis includes vascular demyelinating infectious and other causes and this patient's presentation is most consistent with MS. We have multiple areas of the central nervous system that's involved, the brain and the spinal cord. We have a distribution or separation of this pathology in both space, the brain and spinal cord and time. We have a new lesion in the spinal cord that is enhancing with contrast and old lesions in the brain which is the classic presentation of the patient with multiple sclerosis. So let's learn a little bit more about what the spine MRI and spine pathology looks like in patients with MS. First, we often see that the pathology is located peripherally or laterally and posterior in the white matter. MS is a lesion, a disorder of the white matter tracts and we typically see pathology affecting those areas. We see that the pathology typically spans less than 2 vertebral segments occupying less than half the cross-sectional area of the spinal cord. When we see a long length of pathology within the spinal cord, that's termed a longitudinally extensive transverse myelitis, transverse myelitis just means inflammation at 1 segment of the spinal cord and longitudinally extensive means 3 or more vertebral segments are involved. So that pathology, that white disease, the white matter disease and enhancement that we see spans 3 or more spinal segment and this is suggestive of alternative inflammatory disorders, a disorder called neuromyelitis optica or MOG antibody disorder. We see the pathology in MS often affects the cervical cord. Typically we see that these lesions occupy the lateral or posterior white matter. Typically there is not sparing of the central gray matter and approximately 90% of patients will present initially with clinically definite MS with a single cord lesion and also multiple other lesions that are evidenced at the time of their initial presentation and may have been asymptomatic or unknown to the patient. There is some key features that are supportive of a diagnosis of MS in evaluating an MRI of the spine for patient presenting with myelopathy. First approximately half of the cord shows regions of abnormal T2-weighted signal that's suggestive of MS. During the acute exacerbation, spinal cord enlargement may be seen and typically when the cord is enlarged we think of a cancer or a neoplasm, a space occupying lesion, but we can see expansion of the cord early in acute inflammatory lesions like MS. Spinal cord atrophy is ultimately what's seen. So overtime that area of inflammation results in degeneration of the nerves and we see loss of tissue or atrophy of the spinal cord with longer duration of disease and greater disability.
About the Lecture
The lecture Case: 50-year-old Woman with Lower Extremity Weakness by Roy Strowd, MD is from the course Diseases of the Spinal Cord.
Included Quiz Questions
Which of the following describes a typical presentation of a patient with intradural intramedullary myelopathy?
- Symptoms begin in the arms and progress to the legs; dysfunction of the bowel or bladder is common.
- Symptoms are often asymmetric and localized to one segment of the spinal cord.
- Symptoms begin in the legs and progress to the arms, often with pain.
- Symptoms begin simultaneously in the arms and legs, and pain is common.
Which of the following represents a classic MRI presentation of a patient with multiple sclerosis?
- A new (enhancing) lesion in the cervical spinal cord and multiple old (healed) lesions in the brain in the periventricular white matter
- New lesions in the spinal cord extending for more than two vertebral segments
- Lesions mostly occupying the gray matter
- Spinal cord lesions, usually arising first in the lumbar segment
What is the differential diagnosis of a cervical spinal cord lesion detected by MRI and suspected to be multiple sclerosis? (Select all that apply.)
- Infection
- Acute trauma
- Noninfectious inflammatory process
- Neoplastic process
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |