Playlist
Show Playlist
Hide Playlist
Case: 49-year-old Man with Headache
-
Strowd CNS Tumors Glioma.pdf
-
Download Lecture Overview
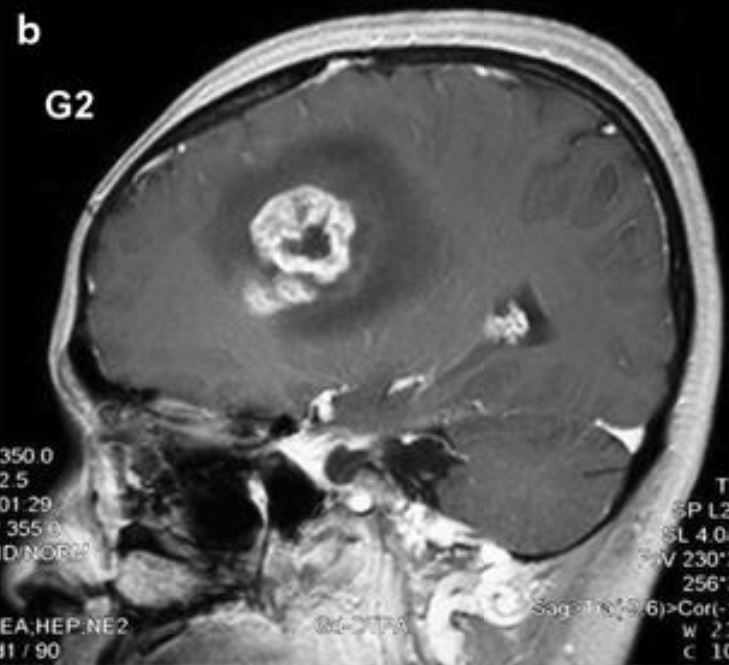
00:01 In this lecture, we're going to talk about gliomas, or that most common type of malignant brain tumor. 00:08 We're going to follow a patient's course through diagnosis and treatment, and learn about how we both approach patients in clinical vignettes for this common and complex type of brain tumor. 00:20 Let's start with a case. 00:22 This is a 49-year-old man who presented with headache. 00:25 He presented with six month history of cognitive complaints, which culminated in persistent dull headaches, and intermittent episodes of word-finding difficulty, possible seizure. 00:37 After presenting to the emergency department with an episode of more prolonged aphasia, a CT scan showed left brain lesions or a left brain lesion. 00:46 and he was admitted to the hospital for MRI of the brain with and without gadolinium contrast. 00:52 Ultimately, the MRI showed a non-enhancing lesion in the left temporal lobe. 00:57 So what's the diagnosis? Well, let's think about some of the features of this case. 01:02 First of all, this patient presents with headache and some type of paroxysmal episode. 01:08 When we think about paroxysmal episodes, episodes that have the same thing every single time, make us concern for a seizure. 01:16 And this sounds concerning for a seizure. 01:19 The second is the imaging. We have a parenchyma lesion, a lesion that appears to be inside the brain, where we think about the cell types that are in the brain in terms of an imaging differential, and this is a non-enhancing lesion, suggesting that it may be lower-grade, which is consistent with the six month history of presentation. 01:38 Here's the imaging for this patient. 01:40 And we're looking at two types of scans here. 01:43 On the left, we see a T2 image that shows us swelling and gliosis anything that's abnormal around this lesion. 01:50 And on the right we see a T1 post-contrast image with gadolinium in the veins but not in this lesion. 01:58 This is a non-enhancing lesion. 02:00 So in summary, this is a lesion in the left temporal lobe without enhancement. 02:05 And this makes us concerned for a low-grade lesion, a low-grade tumor. 02:12 So what's the diagnosis? Is this a brain metastasis, a meningioma, a pituitary adenomas, a glioma, or a vestibular schwannoma? Brain metastasis could be the case but this patient's history is quite long and no systemic malignancy to suggest a clinical history suggestive or consistent with brain metastasis. 02:32 The patient doesn't present with symptoms of a vestibular schwannoma and imaging is not consistent with that. 02:38 The lesion is not in the pituitary or the sella turcica, to suggest a pituitary adenoma. 02:44 This lesion looks to be inside the brain as opposed to developing from the dural surface. 02:49 And imaging would be inconsistent with a dural base lesion like a meningioma. 02:53 This is a glioma. 02:55 And this is the typical a classic presentation for a patient with a low-grade glioma. 03:01 Let's take a different case. 03:03 The same 49-year-old man, but this gentleman presents with a one-month history of cognitive complaints, a shorter time course of presentation that culminated in severe headaches, gait dysfunction and falls and right-sided weakness. 03:18 We don't see a history suggestive of seizure. 03:21 This patient has a focal neurologic deficit, suggesting that this lesion, this mass, maybe this tumor is growing more rapidly. 03:28 Again, after presenting to the emergency department, a CT scan shows multi-focal brain lesions and he's admitted the hospital for an MRI, which shows a ring-enhancing mass involving the corpus callosum. 03:41 So again, the time course is suggestive of more rapid growth. 03:45 We see focal neurologic deficits, which means this patient needs imaging. 03:49 And on imaging, we see a ring-enhancing lesion, which could conjure up an important differential diagnosis for this patient. 03:56 Let's look at this patient's imaging. 03:58 Here again, we're looking at T1 post-contrast imaging on the left, and on the right, the T2 imaging showing this area of edema or swelling, abnormal finding around this tumor. 04:10 This enhancement pattern, the ring of enhancement is concerning for a higher-grade lesion, and a possible tumor. 04:18 So what's the tumor? Is this a brain metastasis, a lymphoma, a low-grade glioma, a high-grade glioma? Or could this be multiple sclerosis? Well, low-grade glioma, we just saw what that looks like. 04:30 and that's typically a nonenhancing or tumor without enhancement, and this one prominently enhances. 04:36 We don't like low-grade glioma. 04:38 Could it be a brain metastasis? It could be, but we've seen in brain metastases that those tumors like the gray-white junction, that area between the cortical gray matter and the subcortical white matter. 04:50 This lesion is in the white matter. 04:51 It's along the corpus callosum, the white matter tracks and actually has a butterfly appearance spreading and emanating from the corpus callosum. 05:00 Could this be lymphoma? It could be. Lymphomas can look tricky. 05:04 But typically lymphomas are homogeneously enhancing. 05:07 And this has a ring-enhancing pattern that really favors an alternative diagnosis. 05:13 What about inflammation? Could this be multiple sclerosis? There's this a type of multiple sclerosis that can cause a tumor like lesion it's called tumefactive MS or tumefactive multiple sclerosis but typically inflammatory lesions don't have a complete ring of enhancement. 05:30 There's an incomplete ring of enhancement. 05:32 And so here the imaging features in clinical presentation favor a high-grade glioma or glioblastoma.
About the Lecture
The lecture Case: 49-year-old Man with Headache by Roy Strowd, MD is from the course CNS Tumors.
Included Quiz Questions
Which of the following is most associated with gliomas?
- Seizures
- History of systemic malignancy
- Hearing loss
- Lesions within the sella turcica
- Dural-based lesions
Which of the following findings on imaging would be most suggestive of a high-grade glioma?
- A ring-enhancing lesion
- A non-enhancing lesion
- A lesion at the gray–white matter junction
- Incomplete ring enhancement due to inflammation
- Diffuse hyperintense lesions
Which of the following is the test of choice to help diagnose a glioma?
- Gadolinium-enhanced MRI
- Non-contrast-enhanced CT
- Contrast-enhanced CT
- Non-enhanced MRI
- CT angiogram
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |