Playlist
Show Playlist
Hide Playlist
Case: 43-year-old Woman with Sharp Pain on the Right Side of Her Face
-
Slides Neuropathic Pain Syndromes.pdf
-
Download Lecture Overview
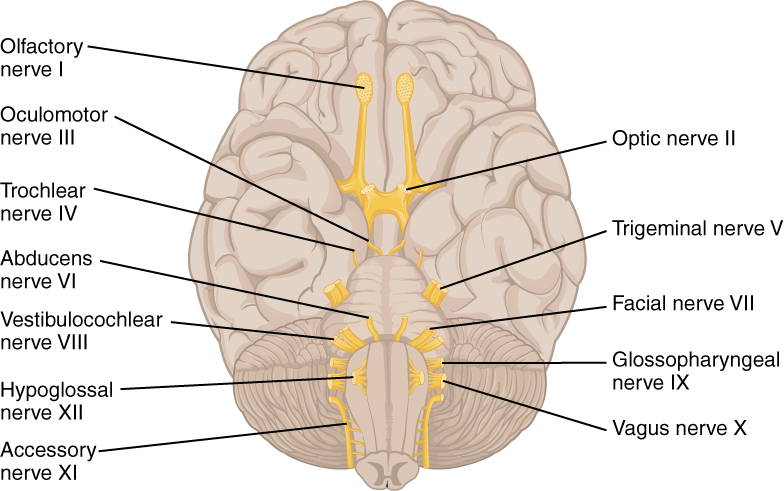
00:01 Now, let's talk about trigeminal neuralgia. Let's start with a case. 00:06 This is a 43-year-old woman who presents to the neurology clinic with significant pain. 00:11 She reports sharp, stabbing electric-like pain on the right side of her face. 00:17 The pain started suddenly two weeks ago. 00:19 She reports that the pain is so excruciating that she can no longer laugh, speak, or eat her meals, as these activities cause episodes of pain. 00:29 She had to miss work last week as a result of this. Her pain attacks last three minutes and resolve when she goes to sleep. 00:36 Currently, she typically has two to three attacks per day. 00:40 Her blood pressure's normal, 132/84, heart rate, 79, respiratory rate, 14. 00:46 A neurologic exam shows no loss of crude touch, tactile touch, or pain sensation on the left side of the face. 00:53 The pupillary light and accommodation reflexes are normal, and there's no drooping of her mouth, or ptosis, or anhidrosis that's noted. 01:02 So what are some of the key features going on in this case? Well, first, we have a neuropathic pain description. 01:08 The patient describes the stabbing, electric-like shooting pain that is very consistent with neuropathic pain. 01:16 Second, we have aggravating factors. The pain is induced by eating, by laughing, by speaking. 01:23 Even touching the face could induce a painful response. 01:26 That's a non-painful stimulus resulting in a painful response which is typical of neuropathic pain. 01:33 This occurs in episodes, maybe worse at night when she's going to sleep and resolves with sleep which is also consistent with neuropathic pain. 01:43 So which of the following is the most likely diagnosis in this patient? Is this cluster headache, postherpetic neuralgia, Bell's palsy, or trigeminal neuralgia? Well, this doesn't sound like a typical description of cluster headache. 01:57 Cluster headaches can be short. They can occur in episodes or clusters, but we often see autonomic symptoms on the side of the head pain. 02:08 This doesn't sound like postherpetic neuralgia. 02:10 There's no history of herpes, there's no vesicular reaction or other cutaneous manifestations to suggest a herpes outbreak. 02:17 We need to watch for that as pain can be the first sign of a Zoster infection, but we don't have evidence for that on our clinical exam as of yet. 02:27 This isn't a Bell's palsy. 02:29 There's no facial weakness that would suggest problems with the facial nerve. 02:33 And this is a classic description of trigeminal neuralgia. 02:37 The patient has lancinating neuropathic pain and the distribution of the trigeminal nerve occurring in episodes unilaterally. 02:44 So let's talk a little bit more about trigeminal neuralgia. 02:48 This is one of the common central neuropathic pain syndromes that I'd like for you to know about. It's a chronic disorder of severe, sudden electrical shock-like burning paresthetic sensations along the trigeminal nerve. 03:02 And there are a few things that are important. 03:04 It has a neuropathic pain description and the neuropathic pain follows the trajectory of the trigeminal nerve. 03:11 It can be induced by activation of the trigeminal nerve as a result of eating, chewing wind, or even touching the face. 03:18 So by activating those sensory nerve fibers, this can induce pain. 03:22 And pain is severe. It can cause severe depression, mood changes, even suicidality because of the severe intensity of pain in these patients. 03:31 This can be a medical emergency. So what's going on? What causes trigeminal neuralgia? Well, I'd like for you to understand the concept of ephatic transmission. 03:43 And what this generally means is a demyelinating nerve when it fires can activate a nociceptive nerve, a painful nerve that's sitting right next to it. 03:52 And this is what happens in trigeminal neuralgia. 03:55 So here we see on the top, a normal sensory nerve. 03:58 It's been focally demyelinated as a result of a blood vessel coming in close proximity or a demyelinating event or some infectious process. 04:06 And that demyelination results in an open area of nerve that can communicate with all the nerves around it. Activation of the sensory nerve can then fire action potential down into the peripheral nociceptor that's not damaged but sitting next to it. 04:23 And we can see here activation of the A-beta fiber results in activation of the painful C fiber, and this is why patients develop neuropathic pain. 04:35 How do we diagnose and manage patients with trigeminal neuralgia? In terms of diagnosis, we need to evaluate for vascular compression, compression from a blood vessel of the trigeminal nerve is one cause and requires surgical intervention. 04:49 We also need to consider perineural invasion in cancer patients, patient with a head and neck cancer that develops new trigeminal neuralgia should be evaluated for spread of the cancer along the nerve. 05:01 In terms of treatments, we think about neuropathic pain agents like carbamazepine or oxcarbazepine. Lamictal, tricyclic antidepressants, and gabapentin or pregabalin can also be used. 05:12 In a surgical intervention, microvascular decompression to relieve the trigeminal nerve in the area around the brain stem can also be successful.
About the Lecture
The lecture Case: 43-year-old Woman with Sharp Pain on the Right Side of Her Face by Roy Strowd, MD is from the course Neuropathic Pain Syndromes.
Included Quiz Questions
What are the symptoms of trigeminal neuralgia?
- Intermittent sharp, stabbing, electric-like pain localized to one side of the face
- Sharp, stinging pain in a dermatomal distribution typically associated with a rash
- Intermittent electric shock–like sensations down the back of the leg
- Shooting pains down the sides of the legs or arms
- Paroxysmal, lancinating pain originating at the base of the skull
What is the term for the phenomenon observed when a demyelinating nerve activates a nociceptive nerve adjacent to it?
- Ephaptic transmission
- Saltatory conduction
- Synaptic transmission
- Interneuron reflex
- Degenerative transmission
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |