Playlist
Show Playlist
Hide Playlist
Case: 31-year-old Woman with Pruritic Vesicles
-
Slides Neuropathic Pain Syndromes.pdf
-
Download Lecture Overview
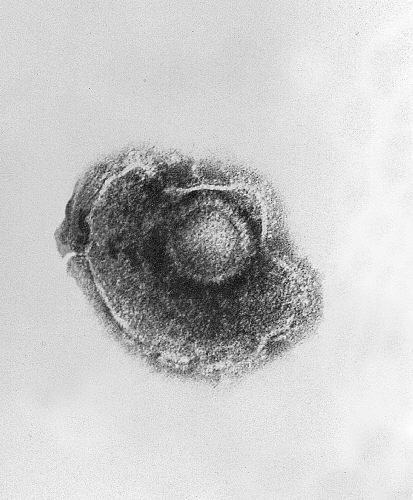
00:01 Now, let's talk about postherpetic neuralgia. 00:04 Let's review a case. This is a 31-year old woman who presents with pruritic vesicles on the right side of her torso. 00:12 She notes that the lesions appeared two days ago and have not improved. 00:16 One day prior to their appearance, she says that she experienced a burning or even electric sensation in the affected area. 00:24 The patient is afebrile and vital signs are within normal limits. 00:28 Upon physical examination, there is painful vesicles noted that are localized to the right T10 skin dermatome. 00:36 So when we think about this case, there are a number of important features that can help to point us to the cause of this neuropathic pain. 00:44 First, is this a central or peripheral nervous system problem? This is squarely a peripheral nervous system problem. 00:51 There are no findings to suggest central nervous system dysfunction. 00:54 And the symptoms, the pain, and the vesicles follow a dermatome which is suggestive of peripheral nervous system localization. 01:03 In addition, there's some other wildcard features in this case. 01:05 The presence of pruritic vesicles raises strong suspicion that this neuropathic pain may be related to a zoster infection. 01:13 So which of the following complications is associated with this patient's most likely diagnosis? One, bacterial superinfection of the affected skin. 01:23 Two, pneumonia. Three, cerebellar ataxia, or four, postherpetic neuralgia. 01:29 This patient wouldn't be at strong risk for bacterial superinfection of the skin. 01:34 Certainly, trauma to the skin, a result of itching, scratching, or damaging these vesicles could contribute to an infection. 01:41 But bacterial infection is uncommon in patients experiencing acute zoster. 01:46 The patient has no findings to suggest risk of pneumonia. 01:50 There's no fever, breathing difficulty, or a systemic process that would raise concern for pneumonia. 01:56 The patient has no symptoms to suggest a central nervous system disorder or cerebellar ataxia which would be quite uncommon in a patient presenting with these symptoms. 02:05 The most common complication for this patient would be a risk of postherpetic neuralgia. 02:11 This is burning sensation, neuropathic pain that's localized to that dermatomal region that develops before, during, and can persist after an acute zoster reaction. 02:23 So let's talk a little bit more about postherpetic neuralgia. 02:27 This is one of the most common complications of Herpes zoster. 02:30 It's characterized by persistence of significant pain, sometimes, for up to months after the development of the initial rash. 02:39 zoster is an infection that has a predilection, a tropism for the peripheral nerves. 02:44 It affects the dorsal root ganglion of a peripheral nerve, causing rash in a dermatome, and potentially, irritating that nerve, resulting in long-term neuropathic pain. 02:55 Here, we can see a good example of the typical zoster rash. 02:59 We see vesicles localized to a single area of the body. 03:03 The vesicles should not cross the midline and should be localized to a specific dermatome or multiple dermatomes, depending on the extent of the zoster infection. 03:14 Postherpetic neuralgia is the pain that develops after a zoster infection. 03:18 Pain arises as the acute Varicella zoster viral infection subsides, and may often persist for a prolonged period of time, or indefinitely post-infection. 03:31 And this can be one of the causes of chronic neuropathic pain syndrome. 03:35 Here, we're looking at a graph. 03:37 And you can see on the x-axis the months since the initial zoster infection and the percent of patients on the y-axis that develop pain. 03:44 We see that any pain is extremely common at the time of infection within the first month. 03:49 Clinically significant pain subsides overtime in the first one to two months after infection, but a small minority of patients will have severe and persistent neuropathic pain syndromes. 04:00 This is why we vaccinate for zoster. It's really not to prevent the acute dermatologic findings, but the long-term risk of postherpetic neuralgia. 04:11 Let's talk a little bit more about the types of pain we can see with postherpetic neuralgia. 04:15 Many patients will describe continuous burning pain or paroxysmal episodes of paresthesias, tingling, numbness, as well as mechanical allodynia, just slightly rubbing over the surface of that skin can result in severe, painful sensation and response. 04:33 There are a number of potential mechanisms that may contribute to this peripheral neuropathic pain syndrome. 04:38 Irritable nociceptors may be one. The infection lies in the nerves. 04:43 And when those nerves become irritated. 04:45 This results in allodynia in regions of preserved sensation. 04:51 Differentiation reorganization. This results in allodynia in regions of sensory loss. 04:57 Where there is sensory loss, allodynia may occur as a result of this mechanism. 05:02 And then loss of interneuron inhibition. 05:05 The infection is actually in the proximal aspects of the nerve and loss of interneuron inhibition may contribute to a higher pain for - pain response and a lower threshold for firing of those peripheral nociceptors that feel pain. 05:21 What are the treatments for postherpetic neuralgia? This can be very difficult to treat in patients. 05:26 We think about topical application with a lidocaine patch or capsaicin cream to sort of override that peripheral painful response, or oral agents like gabapentin and the tricyclic antidepressant which are typically, considered first line. 05:40 And then glucocorticoids or occasionally, opioids can be used for short courses in severe or refractory cases.
About the Lecture
The lecture Case: 31-year-old Woman with Pruritic Vesicles by Roy Strowd, MD is from the course Neuropathic Pain Syndromes.
Included Quiz Questions
What is the most common complication of herpes zoster?
- Postherpetic neuralgia
- Paralysis
- Cerebellar ataxia
- Meningitis
- Pneumonia
What is one of the typical agents used to treat postherpetic neuralgia?
- Gabapentin
- Hydrocodone
- Acetaminophen
- Naproxen
- Carbamazepine
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |